>Corresponding Author : Eslam A Tabl*
>Article Type : Research Article
>Volume : 3 | Issue : 1
>Received Date : 20 Nov, 2022
>Accepted Date : 22 Dec, 2022
>Published Date : 12 Jan, 2023
>DOI : https://doi.org/10.54289/JOP2300101
>Citation : Drali O. (2022) Bone Deformities in Healthy Children Secondary to Hypovitaminosis D. J Orthop Pract 2(1): doi https://doi.org/10.54289/JOP2300101
>Copyright : © 2022 Drali O. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Research Article | Open Access | Full Text
Orthopaedic surgery Department, Faculty of Medicine, Benha University, Benha, Egypt
*Corresponding author: Eslam Abdelshafi Tabl, Orthopaedic surgery Department, Faculty of Medicine, Benha University, Benha, Egypt
Abstract
Background: Distal tibial fractures are usually associated with significant soft tissue injury caused by high energy trauma, which may result in a series of complications such as fixation failure, skin flap necrosis or deep infection.
The aim of this study was to evaluate the result of minimally invasive percutaneous osteosynthesis for treatment of distal tibial fractures associated with soft tissues injuries. including preoperative planning, operative technique, and complication encountered during the study period.
Methods: This prospective study included 20 trauma patients with distal tibial fractures. Patient selection was mainly based on the fracture pattern and the severity of soft tissue status. Patients were subjected to history taking, clinical examination and radiological evaluation.
Results: All fractures were united in a mean period 9 weeks. According to American Orthopedic Foot and Ankle Society (AOFAS) score, 15 patients (75%) were graded as excellent, good in 3 patients (15%) and fair in 2 patients (10%). Complications: This study had 17 patients (85%) with no complication, 2 patients (10%) with skin infection and one patient (5%) had malunion of fracture.
Conclusions: On the basis of the finding of this study it can be concluded that MIPO technique yields good to excellent clinical outcomes with accepted functional outcome for the management of closed distal tibia fractures. Being minimally invasive, it preserves the biological environment by preserving the soft tissue and vascularity and reduces incidence of wound complications.
Keywords: MIPO; External Fixation; Distal Tibial Fractures; Intramedullary Nail
Abbreviations: ORIF: Open Reduction and Internal Fixation, ILN: Intramedullary Nailing, Ex Fix: External fixators, ROM: Range of motion, AOFAS: American Orthopedic Foot and Ankle Society
Introduction
Distal tibial fractures are usually associated with significant soft tissue injury caused by high energy trauma, which may result in a series of complications such as fixation failure, skin flap necrosis or deep infection [1]. The most important predictors that influence the outcome of these injuries are soft-tissue management, the type of fracture, and quality of reduction [2]. Recognizing and managing soft tissue injury is the most important aspect of treating closed fractures [3].
Open Reduction and Internal Fixation (ORIF) in high-energy distal tibia fractures, were associated with infection rates as high as 55%, wound sloughing rates as high as 36% and a few patients in multiple studies eventually required amputation [4].
Intramedullary Nailing (ILN) has the lowest infection rates, but it is associated with other complications such as angular malunion, compartment syndrome and anterior knee pain [5,6]. For ILN, fractures should be > 2 cm from the articular surface with a minimum 2 and preferably 3 well distributed locking screws to provide sufficient stability [2].
External fixators (Ex. Fix) can be used in fractures with soft tissue damage that precludes plate and nail fixation. Its assembly should not jeopardize the attainment of an eventual coverage flap and avoid the course of a possible incision for future surgical treatment [7-9].
Several authors combine an ankle-spanning Ex. Fix with percutaneous screws or wires fixation of articular fragments with good results and low complication rates [10,11]. Instead other authors suggested a staged treatment protocol consists of initial stage of fibular fixation and tibial Ex. Fix followed by a second stage of ORIF when soft tissue swelling has significantly diminished [12,13].
Recently, less invasive biological techniques were introduced in treatment of distal tibial fractures associated with expected fewer soft tissue complications and improve healing. The emphasis lies on indirect reduction and stable fixation preserving most of the vascularization and the osteogenic fracture hematoma which contains all growth factors necessary for bony healing [13].
The aim of this study was to evaluate the result of minimally invasive percutaneous osteosynthesis for treatment of distal tibial fractures associated with soft tissues injuries. including preoperative planning, operative technique, and complication encountered during the study period.
Patients and methods
This prospective study included 20 trauma patients with distal tibial fractures. Patient selection was mainly based on the fracture pattern and the severity of soft tissue status.
The study was done after being approved by the research ethics committee and informed consent was obtained from all participants included.
Inclusion criteria were patient age from 18 to 50 years old, acute fractures that the time between the injury and operation equal to or less than 15 days and closed fractures.
Exclusion criteria were open fractures, old fractures that the time of interval between the injury and operation over 15days, presence of neurovascular injury, pathological fractures and patients younger than 18 years of age.
All patients were subjected to history taking including (Age, sex, medical history, mode of trauma, time of trauma, associated injuries and special habits as smoking).
Clinical examination: Severity of soft tissue injury and neurovascular assessment.
Radiological evaluation: Plain X ray anteroposterior and lateral views and CT if needed to detect the pattern of the fracture.
Surgical technique: The patient position is supine, after provisional reduction, a 3-4 cm vertical incision was made over the medial malleolus towards proximally with care not to injure the saphenous nerve and vein. A subcutaneous tunnel was made using a specialized elevator. The plate was tunneled proximally across the fracture site using the locking sleeve as a handle for insertion of the plate. The plate was centered on the tibia, confirmed on AP & lateral views. When reduction is difficult despite of repeated attempt, a small incision is made using a Kirschner wire (3mm) as a joystick to aid in fracture reduction and towel clip or reduction clamp to hold reduction. Varus valgus angulation < 5° and anteroposterior angulation < 10° and shortening of < 15 mm are considered acceptable criteria for reduction. Cortical screws were inserted first depending on the need for reduction in proximal or distal fragment. After the reduction was confirmed, locking screws were inserted with aim of achieving a minimum of 6 cortices on either side of the fracture
With separate stab incision, at least three locking screws are applied on the either side of fracture. At the end of the procedure, closure was done in layers with non-absorbable sutures.
Postoperative management: Limb elevation over pillows and IV antibiotics are given for 5 days postoperatively. Switching over the oral antibiotics is done on the 5th postoperative day. Analgesics if required are given. All classic radiographic views (AP, lateral) will be obtained. Skin sutures are removed on the 14th postoperative day. Post-operative regimen was to immobilize the fracture in below knee walking cast for a period of 4 to 6 weeks with restricted weight bearing until there was radiological evidence of fracture healing. Full weight bearing was ensued after callus was seen in at least three cortices on AP & lateral views.
Follow up: Routine follow up visits done with X-rays were taken at 1month intervals to assess healing and alignment. On each follow-up, patients were subjected to clinical and radiological assessment: Clinical assessment: On each follow-up patients were asked about subjective symptoms such as pain, limping, need for support when walking. The patients were examined for range of active and passive movements as well as shortening and rotational deformities. Examination to assess union of the fractures was performed. Radiological assessment: The fracture was considered united radiologically on the following criteria: disappearance of the fracture line and good callus formation.
The fracture was considered united clinically on the following criteria: No pain, no tenderness and no abnormal mobility.
At final follow-up, clinical examination was made. Range of motion (ROM) was assessed with a goniometer and the American Orthopedic Foot and Ankle Society (AOFAS) ankle score determined [14]. This scoring system classified the evaluated items into three major categories: pain, function and alignment. In this scale, 50 points have been assigned to function, 40 points to pain, and 10 points to alignment. Usually, a score between 90 and 100 is excellent, 75-89 good, 50-74 fair and < 50 poor.
Cases
Case 1: Female patient 32 years old was presented by trauma due to road traffic injury to the left leg with associated fracture fibula. The patient was operated on 9th day of injury under spinal anesthesia. She had no past history of medical illness. No intraoperative or postoperative complication. Her result was excellent according to ankle hindfoot scale (Fig 1).
Case 2: Male patient 20 years old was presented by trauma due to road traffic injury to the right leg with associated fracture fibula. His result was excellent according to ankle hindfoot scale (Fig. 2).
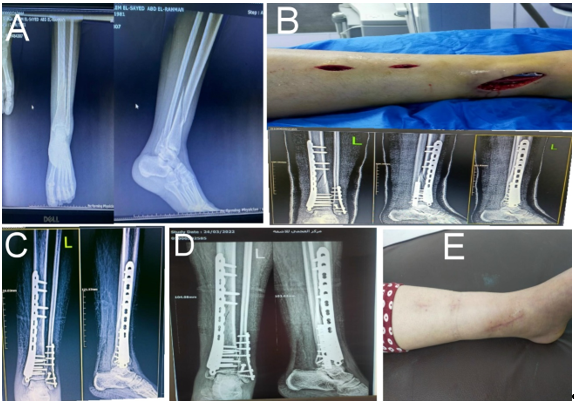
Figure 1: A) Preoperative x-ray, B) Intraoperative photo for incisions and immediate postoperative x-rays, C) 2 months postoperative x ray, D) 6 months x ray, E) Last clinical photo of scars.
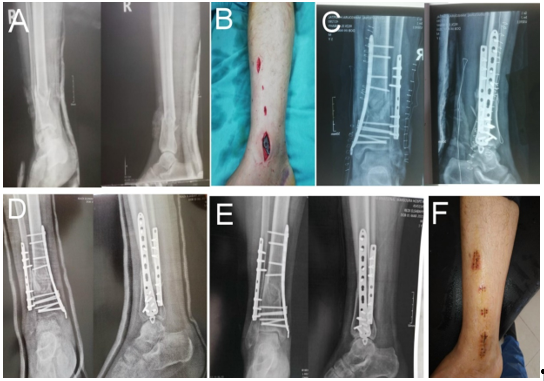
Figure 2: A) preoperative x ray, B) Intraoperative incisions, C) postoperative x ray, D) 2 months x ray, E) 5 months x ray, F) Scars of the operation 5 months postoperative.
Results
Socio-demographic characteristics of the studied cases were shown in Table 1.
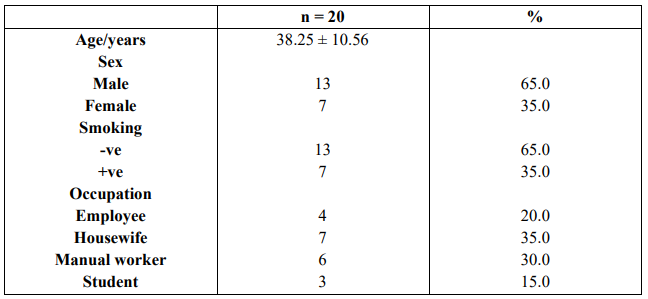
Table 1: Socio-demographic characteristics of the studied cases
Classification of the fracture: 16 patients (80%) were extra articular type A fractures, and 3 patients (15%) were partial intra articular type B.one patient (5%) was complete intra articular fracture type C according to AO/OTA classification Fig 3.
Associated medical disease: Nine patients (45%) had associated medical illness.4 patients (20%) had hypertension and 5 patients (25%) had DM. Clinical results: The result in this study was done according to American Orthopedic Foot and Ankle Society (AOFAS). The results were graded as excellent in 15 patients (75%), good in 3 patients (15%) and fair in 2 patient (10%). Complications: This study had 17 patients (85%) with no complication, 2 patients (10%) with skin infection and one patient (5%) had malunion of fracture. Range of motion: The range of ankle motion in this study in degrees was dorsiflexion (15-20) in 55% patients. and planter 6 (20-35) in 60% patients. Side affected: The right side was affected in 11 cases (55%) and the left side in 9 cases (45%). Mechanism of injury: The mechanism of injury in most cases was road traffic accident which occurs in 11cases (55 %) and falling down injury in 9 cases (45 %). Associated injures: In this study there is 13 patients have associated injuries, 12 of them have fracture lower third fibula and 1 has fracture upper third fibula Table2.
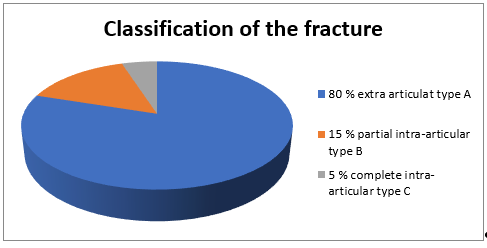
Figure 3: classification of the fracture according to AO/OTA classification.
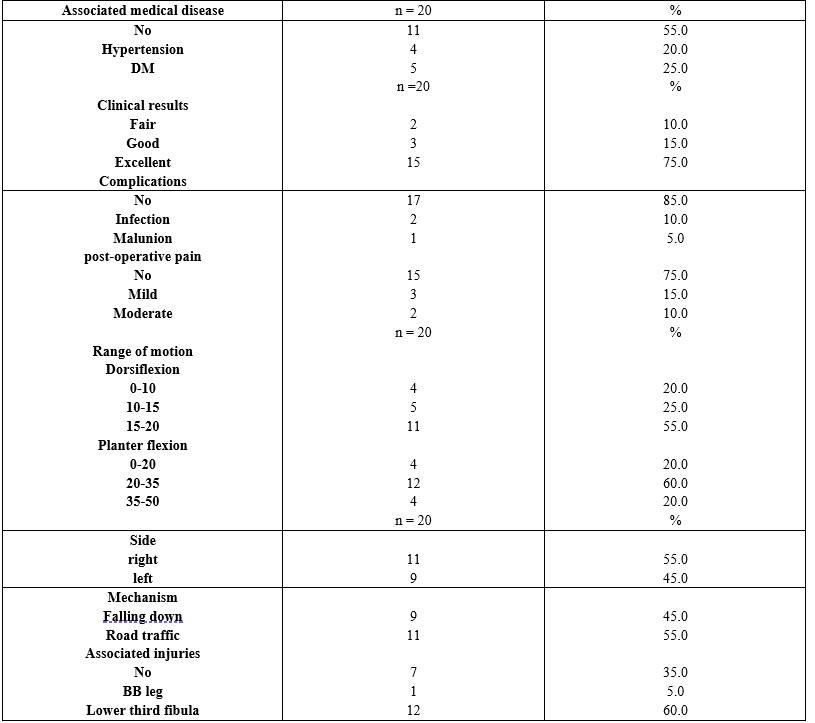
Table 2: Associated medical disease, Clinical results, complications and post-operative pain incidence, range of motion and Injury characteristics among studied cases
Time between injury and operation: Six patients were managed within two days (30%), 6 patients were managed within 2-7 days (30%) and 8 patients were managed more than seven days (40%) Table 3.
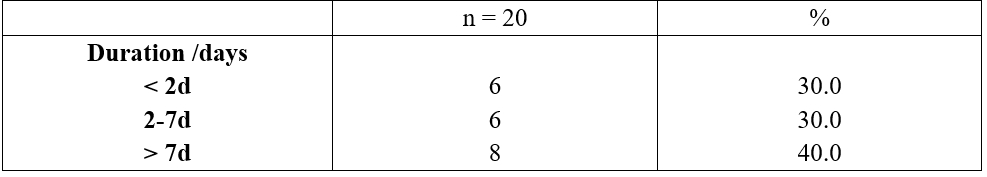
Table 3: Time between injury and operation.
Relation of the age to the results: The incidence of excellent results were in average age group 39.27 years. and the incidence of fair to good results were in average age group 35.20 years. The differences were found to be statistically insignificant (P > 0.05). Relation of the sex to the results: The incidence of excellent results were in male patients (60%) more than in female patients (40 %). The differences were found to be statistically insignificant (P > 0.05). Relation of the smoking to the results: The incidence of excellent results were more in non-smokers (73%). The differences were found to be statistically insignificant (P > 0.05). Relation of the associated medical disease to the results: The incidence of excellent results were more in patients with no associated medical disease (60%). The differences were found to be statistically insignificant (P > 0.05) Table 4.
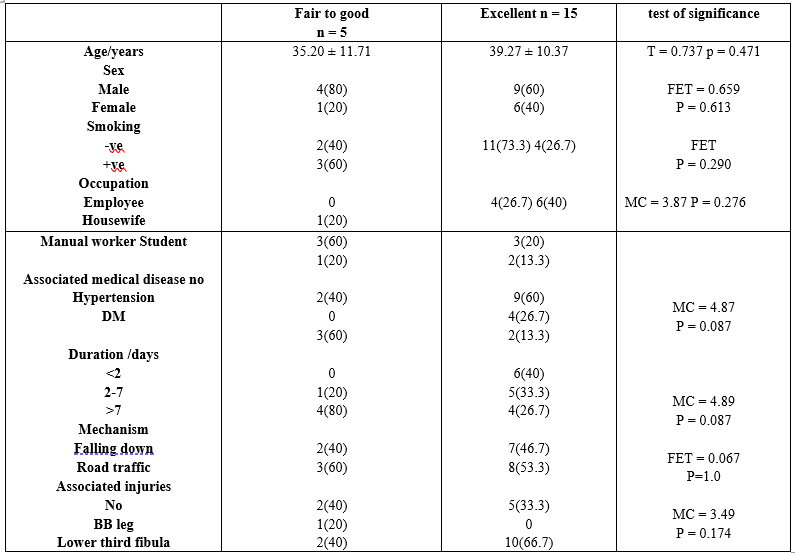
Table 4: Relation between sociodemographic, disease characters and incidence of excellent response among studied cases.
t: Student t test, MC: Monte Carlo test, FET: Fischer exact test, *statistically significant
Relation of the age to complications: The incidence of complications were in age group average 38 years. The differences were found to be statistically insignificant (P > 0.05) (Table 1). Relation of the sex to complications: The incidence of complications were more in male patients (100%). The differences were found to be statistically insignificant (P > 0.05). Relation of the smoking to complications: The incidence of complications were more in smoker patients (66.7%) than nonsmoker patients (33.3%). The differences were found to be statistically insignificant (P > 0.05). Relation of the occupation to complications: The incidence of complications were more in manual worker patients (100%). The differences were found to be statistically significant (P > 0.05). Relation of the associated medical disease to complications: The incidence of complications were more in diabetic patients (66.7%). The differences were found to be statistically insignificant (P > 0.05). Relation of the time between injury and operation to complications: The incidence of complications were more in delayed surgery more than 7 days (66.7%). The differences were found to be statistically insignificant (P > 0.05) Table 5.
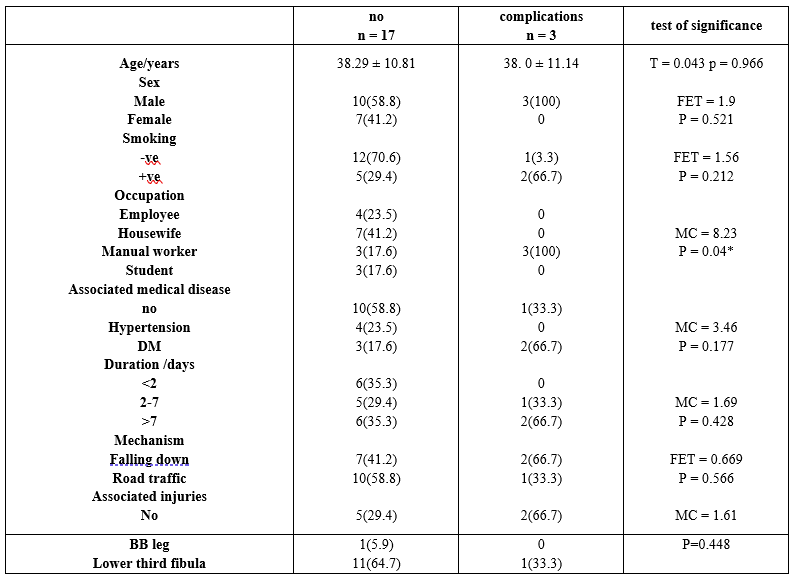
Table 5: Relation between sociodemographic, disease characters and incidence of complications among studied cases.
t: Student t test, MC: Monte Carlo test, FET: Fischer exact test, *statistically significant
Discussion
Minimally invasive plate osteosynthesis (MIPO) is the logical next step in the surgical treatment of fractures. It relies primarily on the indirect reduction of the fracture using various techniques. In this way, the fracture environment is better preserved, as well as the blood supply to the bony fragments [15]. Theoretical advantages include less infection and wound problems and better fracture healing.
Especially in the region of the distal tibia and ankle joint the soft tissues are frequently involved in the sustained trauma and play a central role in the choice of the surgical fracture treatment.
Very often, it is the initial condition of the surrounding soft tissues that limits the possibilities for osteosynthesis and directly relates to the outcome of distal tibial fractures [16].
The importance of a good, mechanically stable osteosynthesis in the treatment of fractures of the tibial plafond has been well emphasized. When fixing the often-comminuted metaphyseal fragment to the diaphysis in an attempt to restore proper axial alignment, very often considerable hardware and thus surgical dissection is required.
Percutaneous plating of the distal tibia offers a similar stability as classic ORIF, however without the need for extensive dissection. Therefore, fewer soft tissue complications can be expected, thus allowing the use of this technique even in the presence of moderate to severe soft tissue contusion or grade I or II open fractures. As such, it promises to be a valid alternative to external (hybrid) fixation, although two-stage procedures may be performed [17]. It is very important to restore the original length and rotation of the lateral column of the ankle joint [18].
Limited open or percutaneous reduction and lagscrew fixation of the distal tibial articular fragments is overall well accepted as the preferred treatment. This is not always possible in complex, very comminuted pilon fractures where a small anteromedial incision needs to be performed to access the ankle joint in order to reconstruct the articular surface of the distal tibia. This same incision can be used to insert the medial plate. It is safe as long as the lateral incision is posterior enough to have a good skin bridge between both incisions.
Although this technique of MIPO offers the possibility of achieving a good mechanical fixation of the distal tibia even in the presence of a metaphyseal defect (as it acts as an “internal fixator” [19].
Recently we have started to use locking compression plates as they allow for the placement of locking head screws in the epiphysis and metaphyseal region, definitely contributing to the mechanical stability of the construct. Moreover, these plates do not have to be perfectly contoured to the bone to achieve optimum stability, which makes their use more simple.
Li et al. [20] have reported no delayed union or nonunion in their retrospective study involving twenty-three patients treated with MIPO. Guo et al. [21] reported no delayed union or nonunion in their prospective randomised study involving forty-one patients treated with MIPO. Seyhan et al. have reported two (5.6%) nonunion with MIPO in their retrospective study. Zou et al. [22] have reported three (7.1%) delayed union with open surgery. In the current study, no patients in the MIPO group had nonunion.
Lee et al. [23] have recommended that they had only three (3.4%) malunions in eighty-eight distal tibia fractures treated with open plating. Zou et al. [22] have reported no malunion in their study with open surgery. Recently, malunion has been common in the MIPO technique, ranging from 2% to 35%.
Zou et al. [22] have reported that malunion was seen in 9.6% of the patients treated with MIPO. The rate of malunion was 9.5% in Borg et al. [24] study with MIPO. In the current study, malunion was reported in one patient (5%) in the MIPO group, as it is difficult to achieve anatomic reduction of the fracture site with minimally invasive plating with indirect reduction.
There was no significant difference with respect to the time from injury to surgery. All surgeries were delayed till the wrinkle sign was diminished.
A greater number of days in hospital causes higher hospital costs to society. In this prospective study, the MIPO group had a significantly shorter hospital stay in the present study, two (10%) superficial infections was noted, it is well-known that distal part of the tibia has poor vascularity and soft tissue coverage, so infection is a common complication. Lee et al. [23] have stated seven (8.0%) superficial infections, Jensen et al. have reported nine superficial infections (9%) in one hundred and five patients. Guo et al. have reported 6 wound problems (14.6%) in thirty-eight patients plated with MIPO technique.
Open methods may have a higher infection rate than that of MIPO due to the risk of insufficient circulation at wound edges, which exposes to the superficial infection [23].
Conclusion
On the basis of the finding of this study it can be concluded that MIPO technique yields good to excellent clinical outcomes with accepted functional outcome for the management of closed distal tibia fractures. Being minimally invasive, it preserves the biological environment by preserving the soft tissue and vascularity and reduces incidence of wound complications.
Declaration of Conflicting Interests
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article. ICMJE forms for all authors are available online.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
ORCID iDs: Eslam Abdelshafi Tabl, MD, https://orcid.org/0000-0001-5561-6361
References
- Tang X, Tang PF, Wang MY, Lü DC, Liu MZ, et al. (2012) Pilon fractures: a new classification and therapeutic strategies Chin Med J (Engl). 125: 2487-2492. [PubMed.]
- Sirkin M, Sanders R, DiPasquale T, Herscovici D. (1999) A staged protocol for soft tissue management in the treatment of complex pilon fractures. J Orthop Trauma. 13: 78-84. [PubMed]
- Robinson CM, McLauchlan GJ, McLean IP. (1995) Court-Brown Distal metaphyseal fractures of the tibia with minimal involvement of the ankle Classification and treatment by locked intramedullary nailing. J Bone Joint Surg Br. 77: 781-787. [PubMed.]
- Bone L, Stegemann P, McNamara K, Seibel R. (1993) External fixation of severely comminuted and open tibial pilon fractures. Clin Orthop Relat Res: 101-107. [PubMed.]
- Im GI, Tae SK. (2005) Distal metaphyseal fractures of tibia: a prospective randomized trial of closed reduction and intramedullary nail versus open reduction and plate and screws fixation. J Trauma. 59: 1219-1223. [PubMed.]
- Cheng W, Li Y, Manyi W. (2011) Comparison study of two surgical options for distal tibia fracture-minimally invasive plate osteosynthesis vs open reduction and internal fixation. Int Orthop. 35: 737-742. [Ref.]
- Mauffrey C, Vasario G, Battiston B, Lewis C, Beazley J, et al. (2011) Tibial pilon fractures: a review of incidence, diagnosis, treatment, and complications. Acta Orthop Belg. 77: 432-440. [PubMed.]
- Teeny SM, Wiss DA. (1993) Open reduction and internal fixation of tibial plafond fractures Variables contributing to poor results and complications. Clin Orthop Relat Res: 108-117. [PubMed.]
- Yildiz C, Ateşalp AS, Demiralp B, Gür E. (2003) High-velocity gunshot wounds of the tibial plafond managed with Ilizarov external fixation: a report of 13 cases. J Orthop Trauma. 17: 421-429. [PubMed.]
- Marsh JL, Bonar S, Nepola JV, Decoster TA, Hurwitz SR. (1995) Use of an articulated external fixator for fractures of the tibial plafond. J Bone Joint Surg Am. 77: 1498-1509. [PubMed.]
- Tornetta P, WeinerL, M Bergman, N Watnik, et al. (1993) Pilon fractures: treatment with combined internal and external fixation. J Orthop Trauma. 7: 489-496. [PubMed.]
- Calori GM, Tagliabue L, Mazza E, de Bellis U, et al. (2010) Tibial pilon fractures: which method of treatment? Injury. 41: 1183-1190 . [PubMed.]
- Papadokostakis G, Kontakis G, Giannoudis P, Hadjipavlou A. (2008) External fixation devices in the treatment of fractures of the tibial plafond: a systematic review of the literature. J Bone Joint Surg Br. 90: 1-6. [PubMed.]
- Farouk, Krettek C, Miclau T, Schandelmaier P, Guy P, et al. (1997) Minimally invasive plate osteosynthesis and vascularity: preliminary results of a cadaver injection study Injury. (28 Suppl 1): A7-12. [PubMed]
- Farouk O, Krettek C, Miclau T, Schandelmaier P, Guy P, et al. (1999) Minimally invasive plate osteosynthesis: does percutaneous plating disrupt femoral blood supply less than the traditional technique? J Orthop Trauma. 13: 401-406. [PubMed.]
- Kilian O, Bündner MS, Horas U, Heiss C, Schnettler R. (2002) [Long-term results in the surgical treatment of pilon tibial fractures A retrospective study. Chirurg. 73: 65-72. [PubMed.]
- Blauth M, Bastian L, Krettek C, Knop C, Evan S. (2001) Surgical options for the treatment of severe tibial pilon fractures: a study of three techniques. J Orthop Trauma. 15: 153-160. [PubMed.]
- Williams TM, Marsh JL, Nepola JV, DeCoster TA, Hurwitz SR, et al. (1998) External fixation of tibial plafond fractures: is routine plating of the fibula necessary? J Orthop Trauma. 12: 16-20. [PubMed.]
- Collinge CA, Sanders RW. (2000) Percutaneous plating in the lower extremity. J Am Acad Orthop Surg. 8: 211-216. [PubMed.]
- Li Y, Liu L, Tang X, Pei F, Wang G, et al. (2012) Comparison of low, multidirectional locked nailing and plating in the treatment of distal tibial metadiaphyseal fractures. Int Orthop. 36: 1457-1462. [Ref.]
- Guo JJ, Tang N, Yang HL, Tang TS. (2010) A prospective, randomised trial comparing closed intramedullary nailing with percutaneous plating in the treatment of distal metaphyseal fractures of the tibia. J Bone Joint Surg Br. 92: 984-988. [PubMed.]
- Zou J, Zhang W, Zhang CQ. (2013) Comparison of minimally invasive percutaneous plate osteosynthesis with open reduction and internal fixation for treatment of extra-articular distal tibia fractures. Injury. 44: 1102-1106. [PubMed.]
- Lee YS, Chen SH, Lin JC, Chen YO, Huang CR, et al. (2009) Surgical treatment of distal tibia fractures: a comparison of medial and lateral plating Orthopedics. 32: 163. [PubMed.]
- Borg T, Larsson S, Lindsjö U. (2004) Percutaneous plating of distal tibial fractures Preliminary results in 21 patients Injury. 35: 608-614. [PubMed.]