>Corresponding Author : Chelsea E Harris
>Article Type : Commentary
>Volume : 4 | Issue : 2
>Received Date : 08 March, 2024
>Accepted Date : 19 March, 2024
>Published Date : 23 March, 2024
>DOI : https://doi.org/10.54289/JDOE2400108
>Citation : Harris CE, Bane WE, McDaniel CR, Blyleven GM, Choi AY, et al. (2024) Advances in Surgical Template Design in Dental Implantology. J Dent Oral Epidemiol 4(2): doi https://doi.org/10.54289/JDOE2400108
>Copyright : © 2024 Harris CE, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Commentary | Open Access | Full Text
1Department of Periodontics, Army Postgraduate Dental School, Postgraduate Dental College, Uniformed Services University, Fort Eisenhower, GA, USA
2Department of Periodontics, Army Postgraduate Dental School, Postgraduate Dental College, Uniformed Services University, Fort Sill, OK, USA
3Department of Periodontics, United States Army Dental Activity, Fort Riley, KS, USA
4Department of Periodontics, United States Army Dental Activity, Fort Liberty, NC, USA
5Department of Periodontics, Army Postgraduate Dental School, Postgraduate Dental College, Uniformed Services University, Fort Meade, MD, USA
6Department of Periodontics, Dental College of Georgia, Augusta University, Augusta, GA USA
7Department of Periodontics, United States Army Dental Activity, Fort Wainwright, AK, USA
*Corresponding author: Chelsea E Harris, Department of Periodontics, Army Postgraduate Dental School, Postgraduate Dental College, Uniformed Services University, Fort Eisenhower, GA, USA
Abstract
Background: Expansion of three-dimensional (3D) printing technology and improvements in planning software have led to increased accuracy and precision in dental implant positioning and new applications for surgical templates in implantology. The objective of this report is to demonstrate the application of locally printed surgical templates in various dental implant surgeries and site development procedures.
Methods: Nine patients were referred to the Department of Periodontics, Army Postgraduate Dental School, Postgraduate Dental College, Fort Eisenhower, GA, USA, for replacement of missing or hopeless teeth using dental implants. All surgeries were planned virtually and completed using customized surgical templates produced within the local facility. The presented cases demonstrate use of surgical templates to simplify surgery across a wide spectrum of clinical scenarios—placement of multiple adjacent implants, immediate implant placement, immediate provisionalization, sinus elevation in dentate and edentulous patients, removal of a retained root fragment in conjunction with implant surgery, alveoloplasty to increase interarch distance, and fully guided implant surgery.
Results: In the presented dental implant surgeries, use of locally produced surgical templates permitted transfer of the planned implant positions to the patients with high reliability. Use of surgical templates in sinus elevation procedures ensured augmentation in the appropriate positions and simplified intraoperative management of complex anatomy.
Conclusions: Specialized surgical templates have the potential to reduce the duration of surgery, limit patient morbidity, enhance communication among clinicians, and simplify the restorative phase of therapy. Accessibility to new technology has allowed implant surgeons to move beyond the era of accurate implant placement into a period characterized by creative solutions to clinical problems.
Keywords: Dental Implants; Clinical Protocols; Alveolar Process; Bone Regeneration; Treatment Outcome
Abbreviations: CAD/CAM: Computer-Aided Design/Computer-Aided Manufacturing, SES: Sinus Elevation Surgery, CBCT: Cone-Beam Computed Tomography, FDBA: Freeze-Dried Bone Allograft, GBR: Guided Bone Regeneration
Introduction
In dental implantology, the importance of three-dimensional (3D) implant position as a critical determinant of both clinical and patient-reported outcome measures has become irrefutable [1-3]. Intuitively, use of a surgical template to restrict implant placement should enhance accuracy compared with reliance upon operator skill to achieve a prosthetically-determined position using anatomic landmarks. Indeed, numerous laboratory-based and clinical investigations support this assumption [4-6]. Beyond guiding implant position, surgical templates serve as a means of communication among dental professionals. In some cases, the template may represent a prescription from the restorative dentist to the surgeon. Today, surgical templates have an extensive taxonomy, ranging from simple conventional restrictive and nonrestrictive templates to elaborate templates used in “fully guided” full-arch rehabilitations [7-9]. Transfer accuracy in template-based implant surgery has been shown to depend on multiple factors including fabrication method, surgical protocol, number of drills, surgeon experience, edentulous site type, and use of template fixation [8,10,11]. Increased effort and expense to produce a low-tolerance surgical template may be justified in cases requiring exquisite accuracy and precision.
In addition to prescribing and guiding implant position, surgical templates have other purposes in dental implantology. Multiple implant site development procedures can be simplified using surgical templates. For example, implant-supported full-arch rehabilitation requires substantial interarch distance, thus compelling preoperative computation of the space requirement and appropriate surgical reduction of the alveolar bone height [12]. A wide variety of alveolar reduction templates have been used to ensure sufficient restorative space without undue hard tissue removal [13,14]. With modern in-office computer-aided design/computer-aided manufacturing (CAD/CAM) techniques, implantologists now have unprecedented flexibility in surgical template design, and creative solutions to clinical problems are often accessible. The purpose of this report is to demonstrate application of innovative CAD/CAM-generated templates to simplify surgery and enhance accuracy in implant surgery and site development procedures.
Multiple Adjacent Implant Sites
At dental implant sites bounded by two normally positioned adjacent teeth, an elaborate surgical template may be unnecessary, particularly for an experienced surgeon [15]. In such cases, the mesiodistal center of the crown space is readily identifiable, and the central grooves of the adjacent teeth provide landmarks demarking ideal orofacial platform position. An intraoperative radiograph during the drilling sequence can confirm proper angulation relative to adjacent roots, and the osseous crest can be used to gauge the platform depth. Multiple adjacent implant placement, by contrast, involves added complexity. At these sites, mesiodistal spacing is not delineated by an adjacent anatomic landmark. Clinicians must provide at least 3 mm between adjacent implants and 1.5 mm (preferably 2 mm) between implants and teeth [1]. In addition, parallelism between adjacent fixtures is often desired. Thus, relative to single implant placement, the importance of a precise surgical template is usually heightened when a clinician plans multiple adjacent fixtures. Fully templated implant surgery may maximize transfer accuracy in multiple adjacent implant cases [8,9]. However, a convenient and cost-effective technique is to print a restrictive 2-mm twist drill template and a non-restrictive confirmation template (Figure 1). The confirmation template can be used to assess the fidelity of the actual versus planned implant position through the drilling sequence. This approach offers efficient placement of multiple adjacent implants with favorable accuracy and the convenience of on-site design and fabrication of relatively inexpensive surgical templates.
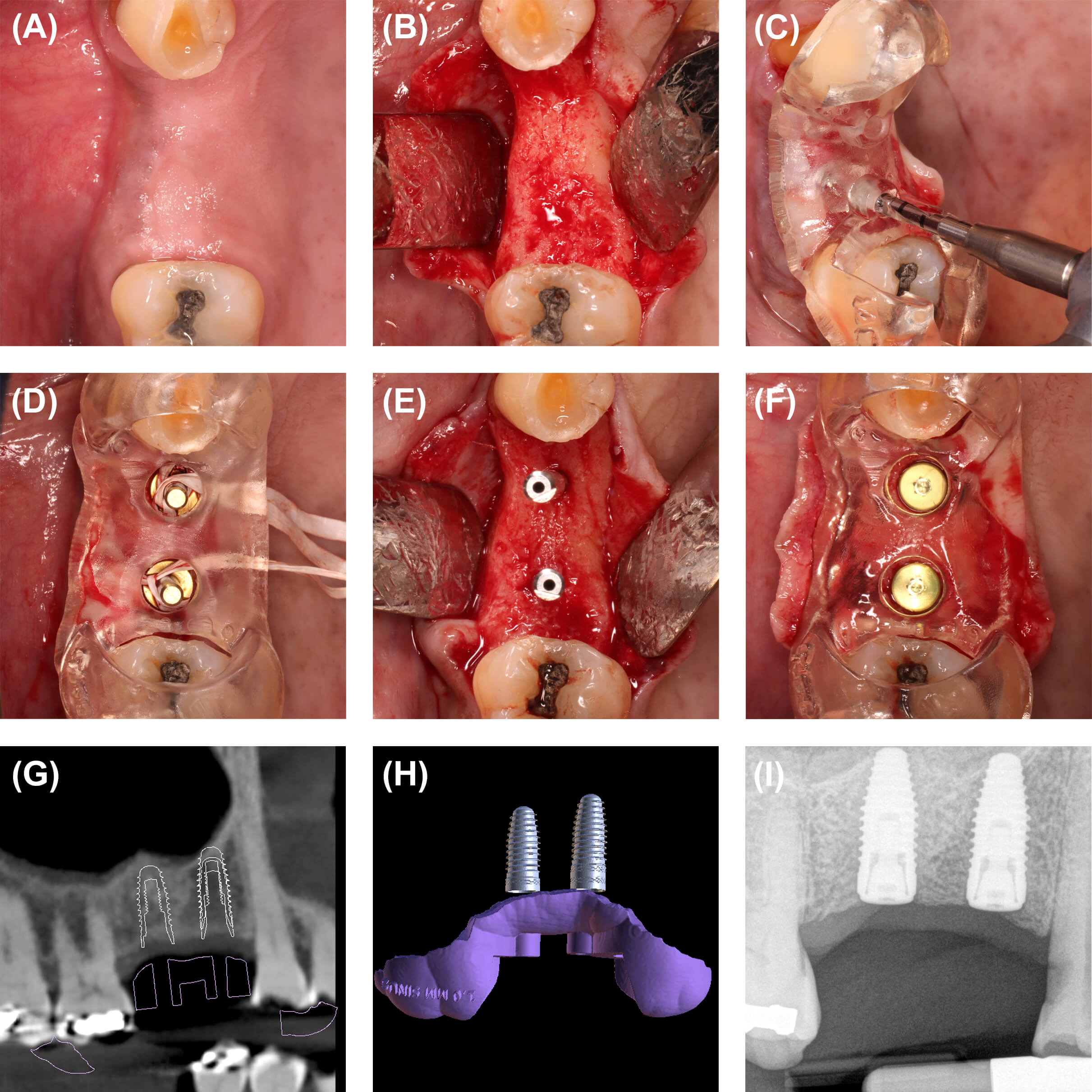
Figure 1: Multiple adjacent implant case. (A) Clinical appearance five months following sinus elevation surgery. Teeth #4 and 5 were missing. (B) Alveolar ridge upon flap reflection. (C) Use of a restrictive 2-mm twist drill template constructed using implant planning software (Blue Sky Plan, Blue Sky Bio, Libertyville, IL, USA) and a 3D printer (Form 3B, Formlabs, Somerville, MA, USA). (D) Nonrestrictive confirmation template used to evaluate osteotomy position throughout the drilling sequence. Sterile ligatures were attached to direction indicators. (E) 4.3 x 10-mm implants (NobelReplace Connical Connection, Nobel Biocare, Kloten, Switzerland) installed. (F) Cover screws in place with implant position assessed using the confirmation template. (G) Cone-beam computed tomography image demonstrating planned implant positions and a trace of the surgical template. (H) Digital representation of the completed surgical template in relation to the planned implant locations. (I) Favorable implant position confirmed radiographically at implant placement.
Immediate Implant Placement in the Esthetic Zone
Broad consensus holds that 3D implant position ranks among the most important factors in establishment of an esthetic implant-retained restoration at maxillary anterior tooth positions [1,16]. Surgical template use for immediate implant placement in this anatomic location can present a technical challenge. Implant drills may have insufficient length to pass through the template, enter the extraction socket, and engage the apical/palatal alveolar bone to the planned depth. To address this problem, the surgical template itself can be designed to enter the extraction socket, effectively restricting the osteotomy location while minimizing obstruction of the handpiece as it moves apically (Figure 2). A confirmation template can be used during the shaping drill sequence and after implant installation.
Immediate Provisionalization
Placement of an immediate provisional restoration at implant surgery may enhance patient satisfaction and help clinicians to develop favorable peri-implant mucosal contours [17,18]. Advancements in implant planning software and 3D printing technology now offer the ability to fabricate an implant template that can be converted chairside into an immediate provisional restoration (Figures 3-5). This approach requires additional preoperative planning but provides obvious advantages in terms of reduced chair time and enhanced patient-reported outcomes.
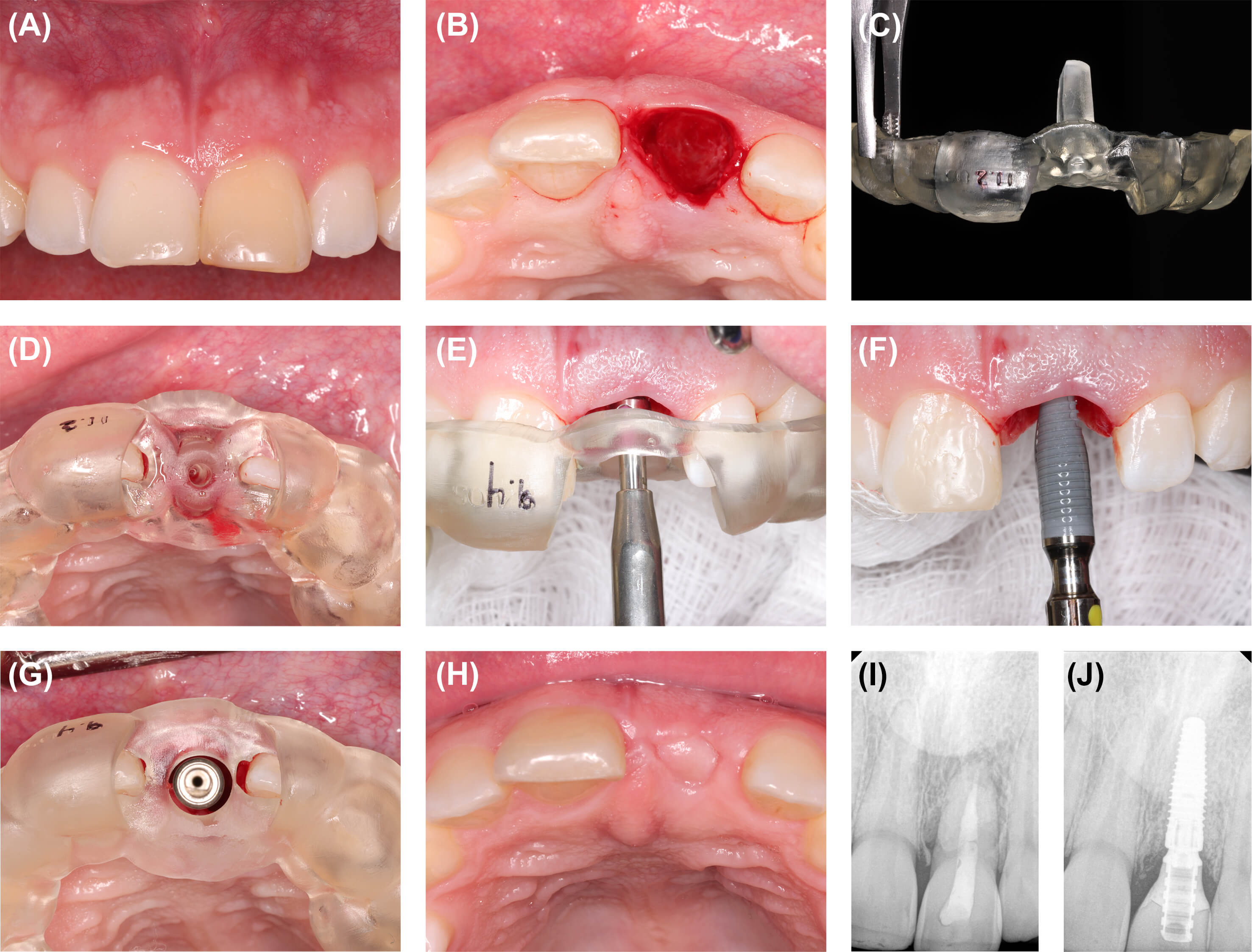
Figure 2: Immediate implant placement in the esthetic zone. (A) Baseline clinical appearance. Tooth #9 was nonrestorable due to root resorption and an unfavorable crown-to-root ratio. (B) Extraction socket. (C) 3D-printed 2-mm twist drill template (Form 3B, Formlabs, Somerville, MA, USA) designed to enter the extraction socket. (D) Restrictive 2-mm twist drill template in place. (E) Shaping drill sequence completed with confirmation template in place. Implant platform depth can be evaluated based on the position of the shaping drill relative to the incisal margin of the template. (F) A 4.3 x 10-mm implant (NobelReplace Connical Connection, Nobel Biocare, Kloten, Switzerland) was stabilized with insertion torque of 40 Ncm. (G) Implant position evaluated using the confirmation template. A particulate solvent-dehydrated bone allograft (Puros, ZimVie, Westminster, CO, USA) was placed in the peri-implant gap defect, and a free gingival graft was applied over the socket orifice. (H) Clinical appearance three months following implant placement. (I) Baseline radiograph. (J) Favorable radiographic peri-implant bone levels noted at postoperative month six.

Figure 3: Surgical template design for chairside conversion to immediate provisional implant-supported crown, tooth #12 area. (A) Combined template/provisional crown after completion of the intitial osteotomy. (B) A 4.1 x 10-mm implant (Osseotite Tapered Certain, ZimVie, Westminster, CO, USA) was installed with insertion torque of 90 Ncm. (C) Provisional abutment stabilized. (D) Surgical template converted to provisional implant-supported crown. (E) Appearance of provisional crown at postoperative month four.
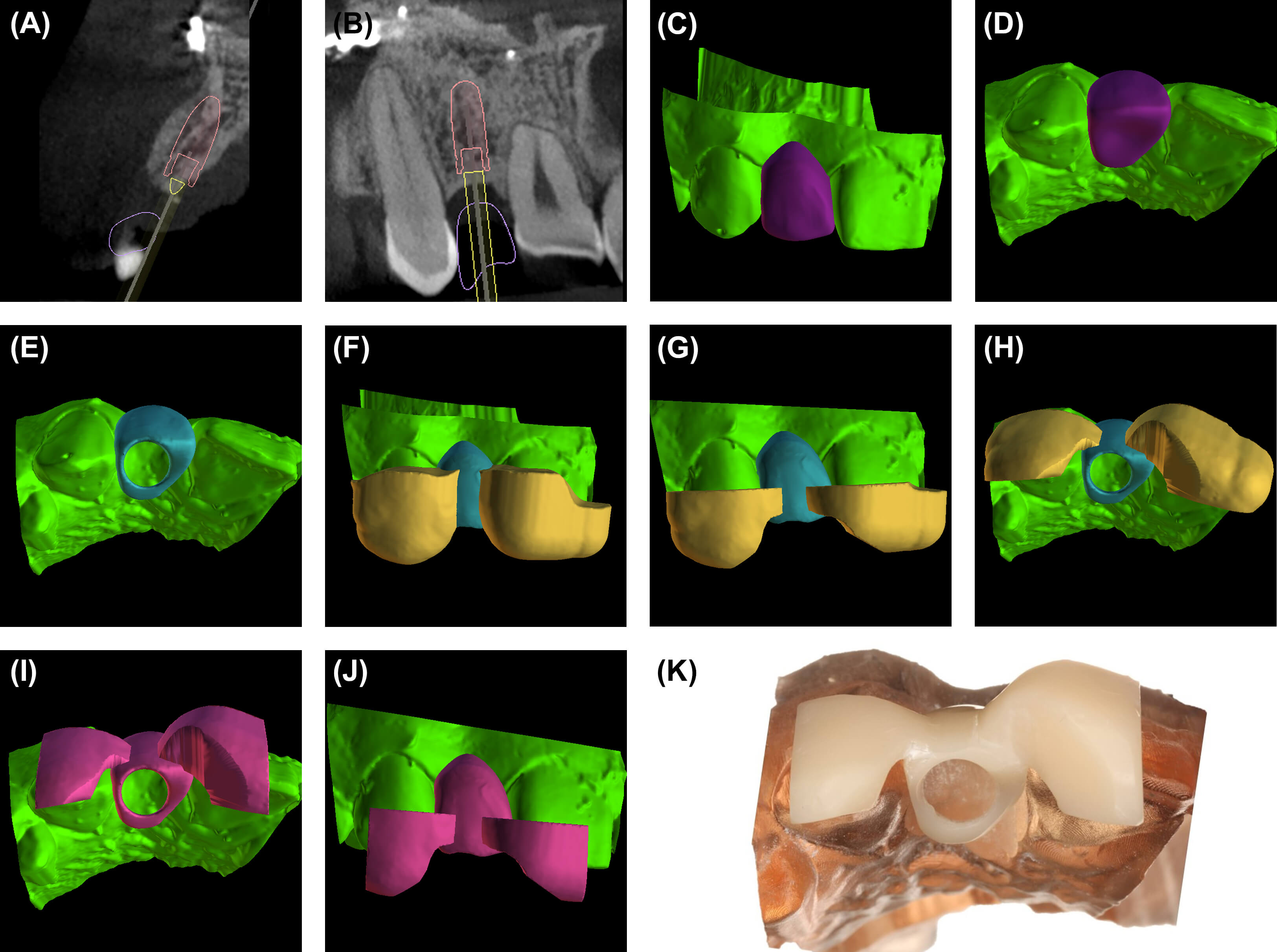
Figure 4: Surgical template design for chairside conversion to immediate provisional implant-supported crown, tooth #7 position. (A) Cone-beam computed tomography (CBCT) cross-sectional view five months following alveolar ridge augmentation, tooth #7 area. The retained screw is from prior orthognathic surgery. (B) Custom CBCT slice through teeth #6 and 8. (C) Digital wax-up of the planned implant-supported crown. (D) Incisal view of the digital wax-up. (E) Implant template channel placed in the digital wax-up. (F) Tooth-supported components of the surgical template established. (G) Surgical template trimmed to minimize contact of support elements with the temporary crown. (H) Incisal view. (I) Surgical template connected with digital wax-up. (J) Facial view. (K) Completed implant template that will be converted to the provisional crown at implant surgery (see Figure 5).

Figure 5: Conversion of surgical template to provisional implant-supported crown (surgical template design shown in Figure 4). (A) Appearance of the alveolar ridge immediately prior to implant placement, tooth #7 area. (B) Minimal facial flap reflection. (C) Combined surgical template/provisional restoration connected with a provisional abutment. (D) Polished provisional crown after conversion of surgical template (facial view). (E) Distal view. (F) Flap sutured. (G) Favorable implant position confirmed radiographically at implant placement. (H) Appearance of provisional restoration at postoperative week four.
Sinus Elevation Surgery, Partially Edentulous Maxillary Arch
Various developmental and acquired conditions—such as presence of a prominent intraosseous artery, septum, or antral wall discontinuity—can increase the complexity of sinus elevation surgery (SES) and elevate the risk of an intraoperative or postoperative complication [19-21]. In patients with a partially edentulous maxillary arch, a tooth-supported surgical template can identify locations of anatomic structures such as the sinus floor and antral septae (Figure 6). These templates may simplify completion of the lateral wall osteotomy, reduce the duration of surgery, and decrease the risk of morbidity for the patient.
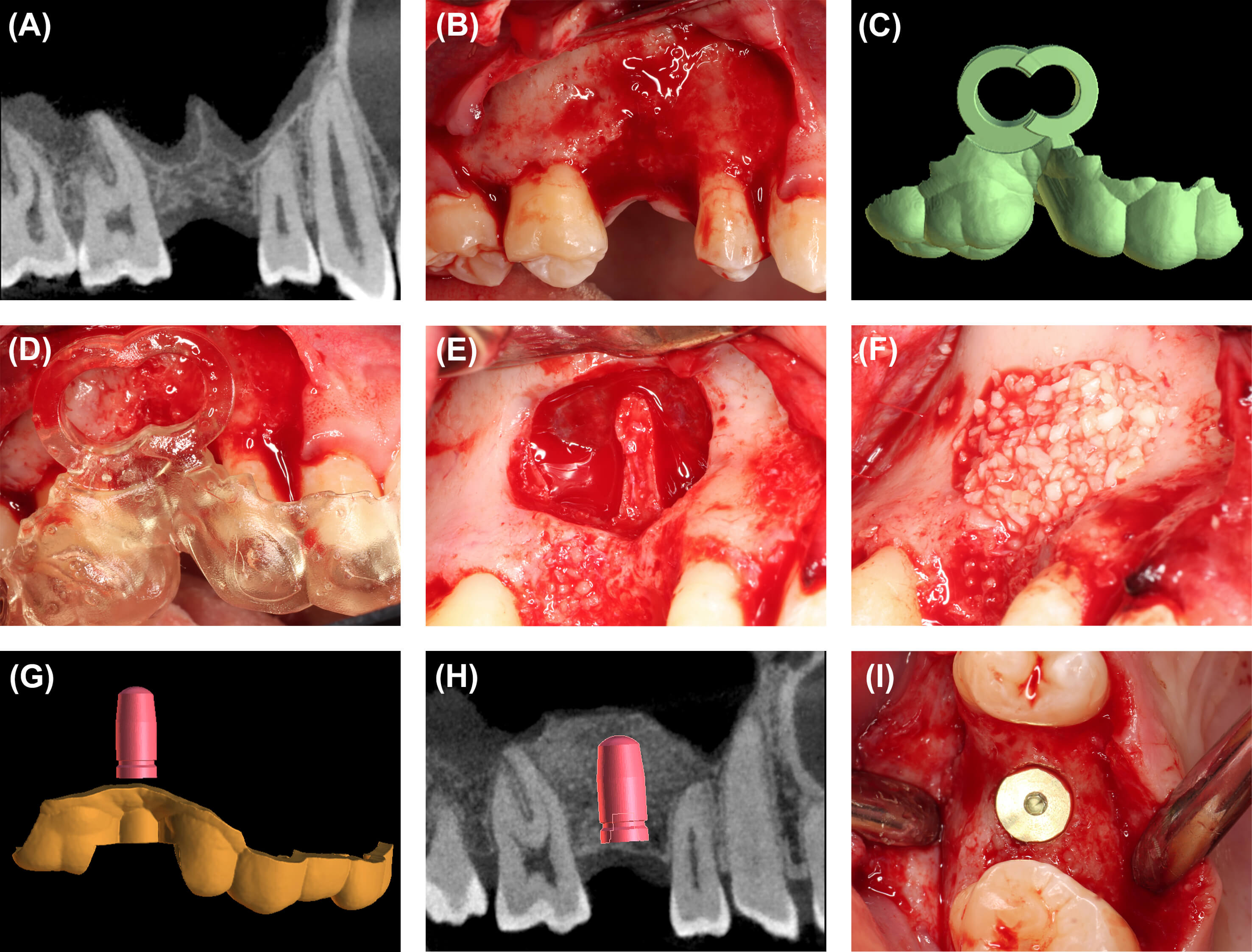
Figure 6: Sinus elevation surgery, partially edentulous maxillary arch, tooth #3 area. (A) Baseline cone-beam computed tomography (CBCT) image. (B) Buccal mucoperiosteal flap reflection. (C) Digital representation of the completed sinus elevation surgical template. (D) Tooth-supported surgical template outlining the lateral wall osteotomy and identifying the location of a prominent septum. (E) Schneiderian membrane reflected without perforation. (F) Freeze-dried bone allograft (Stryker, Kalamazoo, MI, USA) in place. (G) Volume rendering of the planned implant position and the surgical template for implant placement. (H) CBCT image five months following sinus elevation with virtual implant in place. (I) Clinical appearance of the 5 x 11.5-mm implant (Osseotite Tapered Certain, ZimVie, Westminster, CO) six months following sinus elevation.
Sinus Elevation Surgery, Edentulous Maxillary Arch
In a patient with an edentulous maxillary arch, determining the mesiodistal location where augmentation is needed can be challenging. No teeth are present to provide clinical and radiographic orientation, and fabricating a tooth-supported SES template is not possible. Fortunately, a tissue-supported template can help the clinician transfer the planned mesiodistal and inferosuperior osteotomy boundaries to the patient (Figure 7).
Removal of a Root Fragment, Pathologic Osseous Lesion, or Foreign Body
Some high-, low-, and mixed-density osseous lesions and conditions present low risk for implant failure and other postoperative complications. However, some entities presenting with similar radiological appearances contraindicate implant placement [22]. When removal of a lesion or entity is indicated, use of a trephine template can pinpoint the osteotomy location, substantively reduce surgical trauma, and permit simultaneous implant placement (Figure 8).
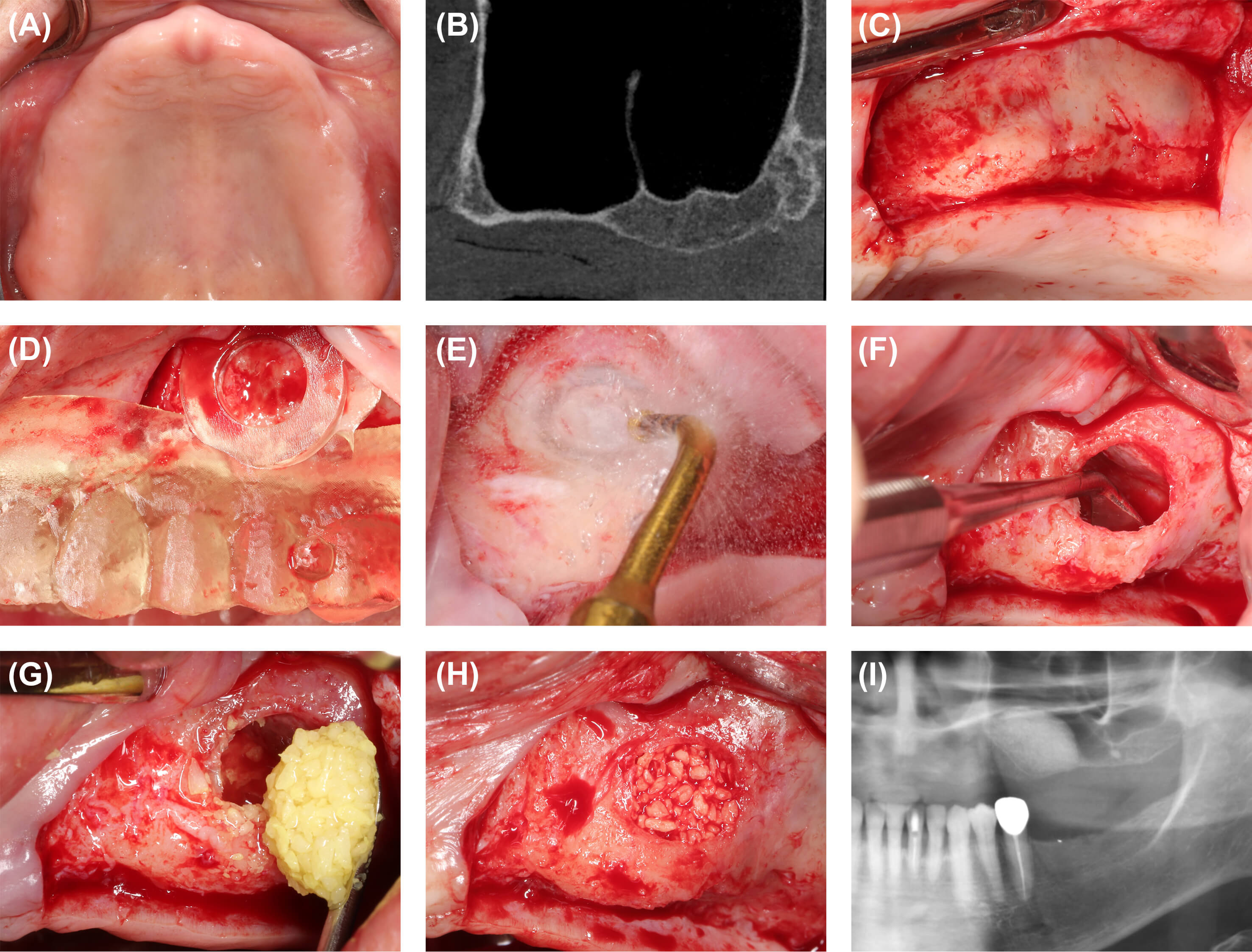
Figure 7: Sinus elevation surgery, edentulous maxillary arch. (A) Baseline clinical appearance of maxillary arch. (B) Baseline cone-beam computed tomography image of the left maxillary sinus. (C) Buccal mucoperiosteal flap reflection. (D) Tissue-supported sinus elevation surgical template demonstrating the planned location of the augmentation. (E) Antral access was achieved using a piezosurgery instrument (Mectron North America, Hilliard, OH, USA). (F) Reflection of the Schneiderian membrane. (G) Placement of a particulate freeze-dried bone allograft (FDBA) (Stryker, Kalamazoo, MI, USA) hydrated in a dilute tetracycline solution (100 mg/ml) then rinsed with copious normal saline. (H) FDBA in place. (I) Panoramic radiograph six months following sinus elevation. The augmentation was located in a favorable position for implant placement.
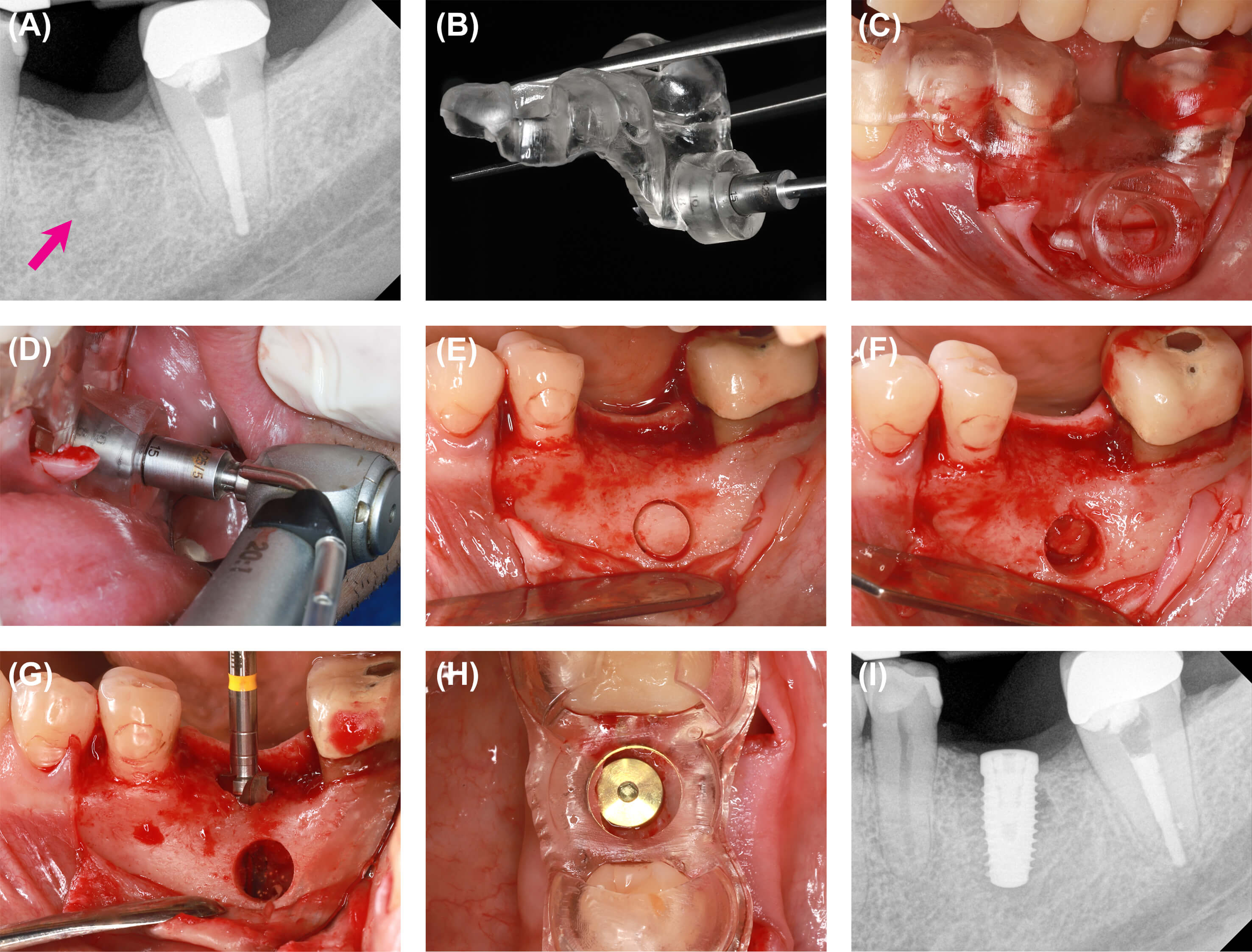
Figure 8: Removal of retained root fragment in conjunction with implant surgery. (A) Baseline periapical radiograph showing retained root fragment (arrow) at planned implant location (tooth #19 area). (B) 3D-printed surgical template (From 3B, Formlabs, Somerville, MA, USA) designed to template both implant position and placement of 6-mm trephine for root fragment removal. (C) Surgical template in place. Note use of the template to retract the buccal flap. (D) Placement of the handpiece for trephine drill use. (E) Initial trephine osteotomy. (F) Cortex overlying the root fragment removed. The root fragment was removed through the osteotomy. (G) Final shaping drill (5 mm in diameter). (H) 5 x 11.5-mm implant (Osseotite Tapered Certain, ZimVie, Westminster, CO, USA) stabilized with cover screw in place. Implant position was assessed using a nonrestrictive confirmation template. A particulate freeze-dried bone allograft (Stryker, Kalamazoo, MI, USA) was applied through the buccal osteotomy, and the segment of cortex removed to access the root fragment was reapplied at the trephine osteotomy prior to closure. (I) Favorable implant position confirmed radiographically at placement.
Alveoloplasty to Increase Interarch Distance
An implant-supported fixed complete denture represents one treatment option for a patient who desires to avoid a removable prosthesis for an edentulous arch [12]. A major disadvantage of this treatment is the requirement to establish sufficient interarch distance to accommodate the prosthesis and the transmucosal implant components. Almost invariably, substantial reduction of the alveolar bone is obligatory. Failure to create adequate interarch distance can compromise the treatment outcome or even preclude proceeding with a fixed reconstruction, yet excessive removal of alveolar bone could be catastrophic. Use of a bone reduction template allows the surgeon to efficiently place the alveolar bone at the planned vertical level (Figure 9).
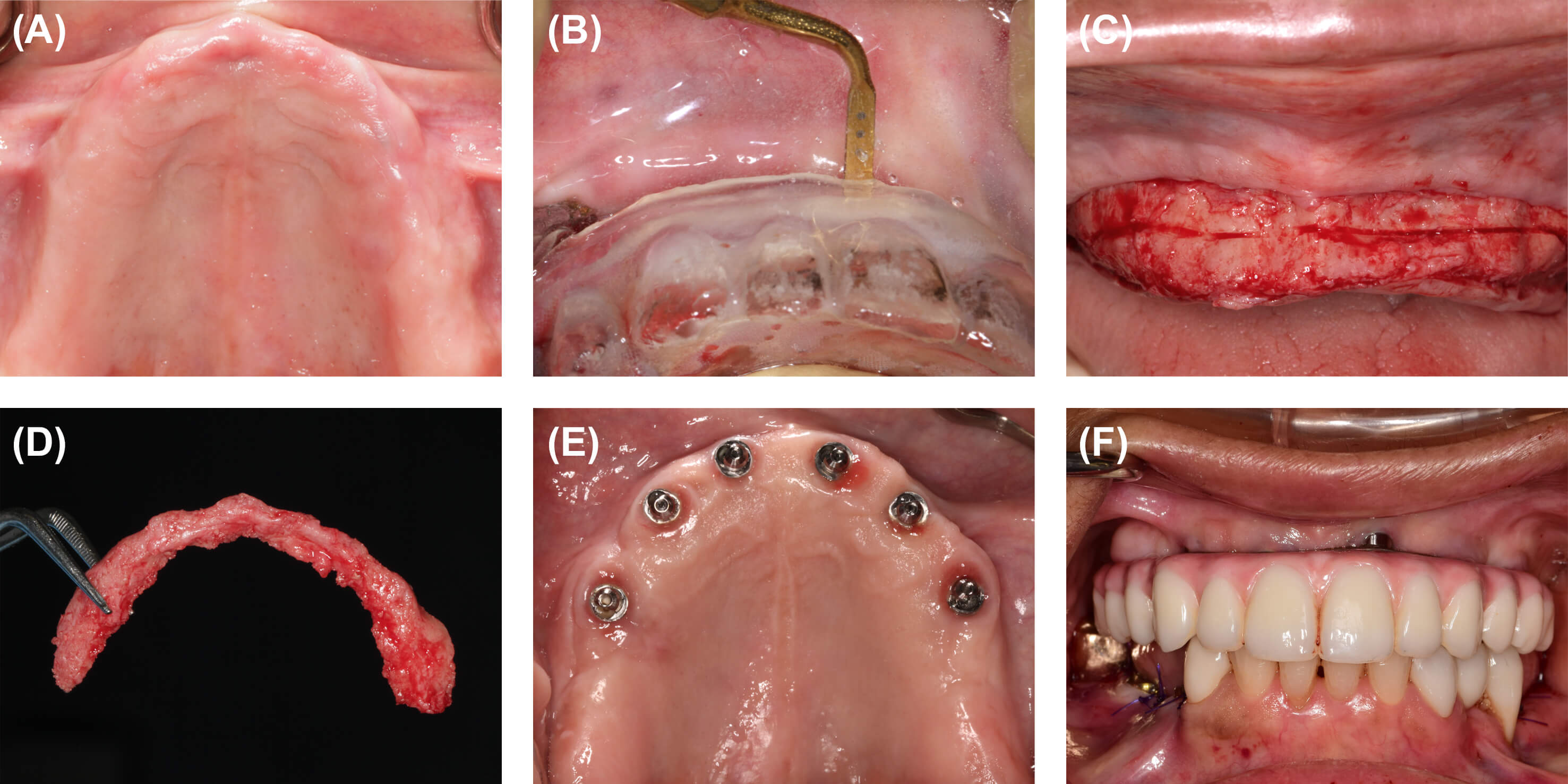
Figure 9: Alveoloplasty to increase interarch distance for implant-supported full-arch restoration. (A) Baseline appearance of maxillary arch. (B) Use of surgical template to accurately reduce alveolar bone height to the planned vertical level. (C) Initial osteotomy using a piezosurgery instrument (Mectron North America, Hilliard, OH, USA). (D) Crestal alveolar segment removed. (E) Appearance of six 4.3 x 10-mm implants (Nobel Replace Conical Connection, Nobel Biocare, Kloten, Switzerland) at postoperative month 24. The fixture in the #9 position was treated for peri-implant mucositis. (F) Facial view of the implant-supported full-arch prosthesis at postoperative month 24.
Fully Guided Surgery
Accuracy and precision in implant positioning may be maximized using fully guided surgery. In such procedures, every drill—even installation of the implant—is restricted by the surgical template. Fully guided surgery offers maximal control over all dimensions of the implant position including depth, angulation, orofacial and mesiodistal positions, and the orientation of the internal features of the implant. Because the timing of the internal aspect of the implant is controlled, it is possible to fabricate a high quality provisional crown prior to implant installation (Figure 10) [23]. Use of fully guided surgery often requires specialized surgical kits and may increase the planning time and overall cost of the procedure.
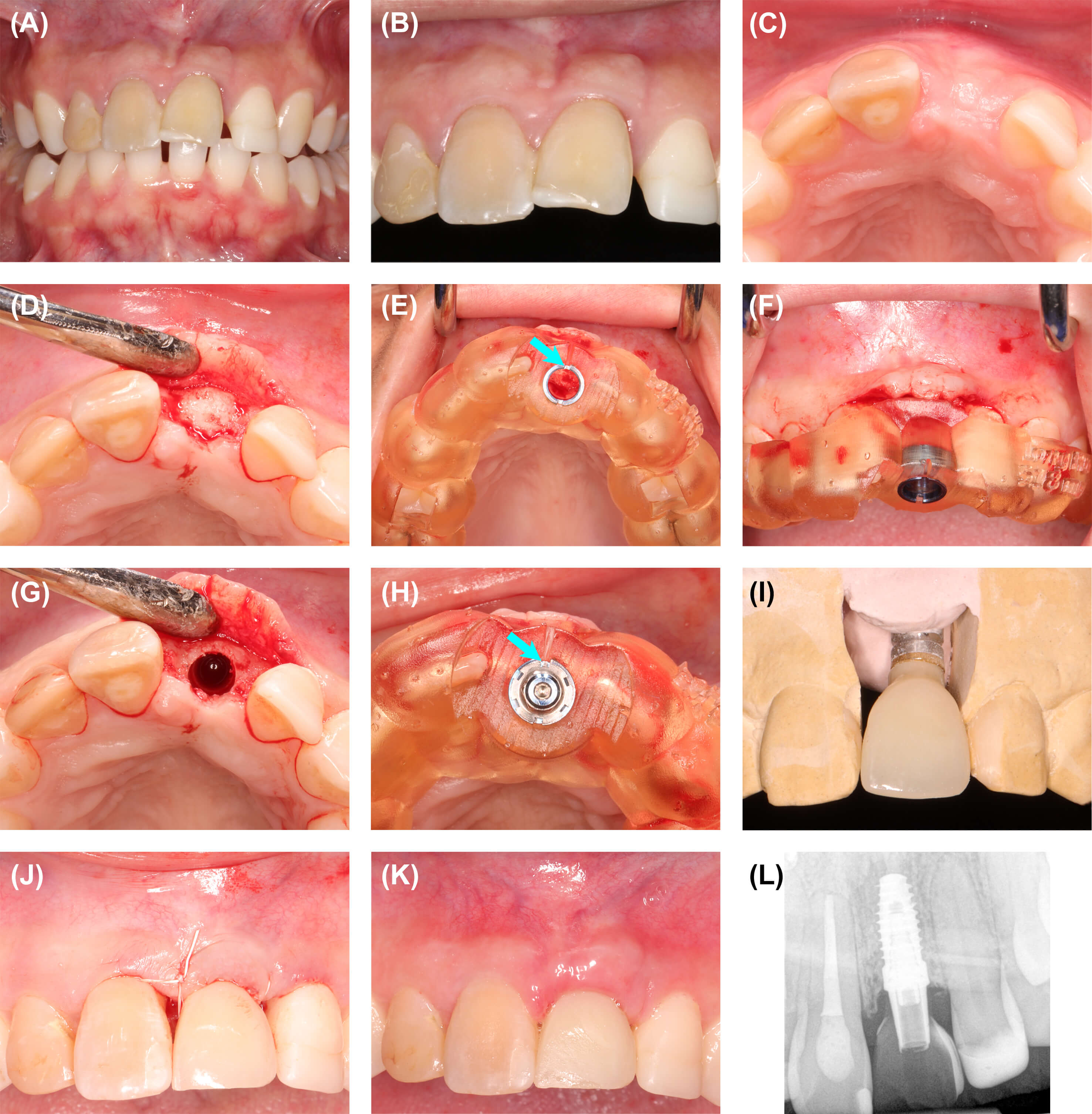
Figure 10: (A) Baseline clinical appearance. The patient had a history of trauma to the maxillary anterior. Tooth #9 had a hopeless prognosis due to severe root resorption. (B) Close-up view of maxillary incisors. (C) Alveolar ridge following extraction of tooth #9, alveolar ridge preservation, and guided bone regeneration (GBR). Following GBR, the site was allowed to heal for six months prior to implant surgery. (D) Flap reflection for implant placement. (E) A fully guided implant system (Navigator, ZimVie, Westminster, CO, USA) was used to position the implant. Facial and palatal channels in the guide tube (arrow) permitted control over the internal timing of the implant abutment connection. (F) Facial view of the surgical template. (G) Implant osteotomy completed. (H) Implant installed through the surgical template. A channel in the implant carrier (arrow) was aligned with the channel in the guide tube dictating the orientation of the internal aspect of the implant. (I) Provisional implant-supported crown fabricated in the lab prior to implant surgery. The timing of the implant abutment was matched with the planned implant orientation using a specialized laboratory kit (Navigator, ZimVie). (J) Wound closure at the completion of implant surgery. (K) Clinical appearance at postoperative week two. (L) Periapical radiograph at implant placement.
Conclusion
Widespread availability of 3D printing technology and advanced implant planning software has revolutionized treatment planning in complex dental implant cases. Practitioners now have unprecedented flexibility in designing surgical templates that simplify site development procedures and dental implant placement. In every implant surgery, ideal 3D positioning is a critical clinical aspiration, and the value of a high precision surgical template is proportional to case complexity. The surgical templates highlighted herein have demonstrated the use of locally produced CAD/CAM surgical templates to simplify placement of multiple adjacent implants, immediate implant surgery in the esthetic zone, immediate provisionalization, alveoloplasty to increase interarch distance, and removal of a retained root fragment in conjunction with implant surgery. Application of the techniques demonstrated in this report is limited primarily by operator creativity. As software and printing systems continue to evolve, and innovations involving artificial intelligence integrate with medicine and dentistry, advancements in surgical templates in dental implantology will likely continue at a rapid pace.
Disclaimer
The views expressed in this manuscript are those of the authors and do not necessarily reflect the official policy of the United States Government, the Department of Defense, the Defense Health Agency, or Uniformed Services University of the Health Sciences.
Conflict of interest statement: The authors report no financial, economic, or professional interests that may have influenced the design, execution, or presentation of this work.
Funding: The authors received no funding for this report.
Author contribution statement: All authors contributed substantially to conceptualization, original draft preparation, critical review, and editing of this manuscript. All authors approved the final version of the manuscript.
References
- Grunder U, Gracis S, Capelli M. (2005) Influence of the 3D bone-to-implant relationship on esthetics. Int J Periodontics Restorative Dent. 25(2): 113-119. [PubMed.]
- Cosyn J., Sabzevar MM., De Bruyn H. Predictors of inter–proximal and midfacial recession following single implant treatment in the anterior maxilla:a multivariate analysis. J Clin Periodontol. 2012;39(9):895–903. [PubMed.]
- Schwarz F., Derks J., Monje A., Wang HL. Peri–implantitis. J Periodontol. 2018;89 Suppl 1:S267–S290. [PubMed.]
- Scherer U., Stoetzer M., Ruecker M., Gellrich NC., von See C. Template–templated vs. non–templated drilling in site preparation of dental implants. Clin Oral Investig. 2015;19(6):1339–1346. [PubMed.]
- Bover–Ramos F., Viña–Almunia J., Cervera–Ballester J., Peñarrocha–Diago M., García–Mira B. Accuracy of implant placement with computer–templated surgery:A systematic review and meta–analysis comparing cadaver., clinical., and in vitro studies. Int J Oral Maxillofac Implants. 2018;33(1):101–115. [PubMed.]
- Behneke A., Burwinkel M., Behneke N. Factors influencing transfer accuracy of cone beam CT–derived template–based implant placement. Clin Oral Implants Res. 2012;23(4):416–423. [PubMed.]
- D'haese J., Ackhurst J., Wismeijer D., De Bruyn H., Tahmaseb A. Current state of the art of computer–templated implant surgery. Periodontol 2000. 2017;73(1):121–133. [PubMed.]
- Abduo J., Lau D. Accuracy of static computer–assisted implant placement in anterior and posterior sites by clinicians new to implant dentistry:In vitro comparison of fully templated., pilot–templated., and freehand protocols. Int J Implant Dent. 2020;6:1–3. [Ref.]
- Younes F., Cosyn J., De Bruyckere T., Cleymaet R., Bouckaert E., et al. A randomized controlled study on the accuracy of free‐handed., pilot‐drill templated and fully templated implant surgery in partially edentulous patients. J Clin Periodontol. 2018;45(6):721–732. [PubMed.]
- Putra RH., Yoda N., Astuti ER., Sasaki K. The accuracy of implant placement with computer–templated surgery in partially edentulous patients and possible influencing factors:A systematic review and meta–analysis. J Prosthodont Res. 2022;66(1):29–39. [PubMed.]
- Zhou W., Liu Z., Song L., Kuo CL., Shafer DM. Clinical Factors Affecting the Accuracy of Templated Implant Surgery–A Systematic Review and Meta–analysis. J Evid Based Dent Pract. 2018;18(1):28–40. [PubMed.]
- Carpentieri J., Greenstein G., Cavallaro J. Hierarchy of restorative space required for different types of dental implant prostheses. J Am Dent Assoc. 2019;150(8):695–706. [PubMed.]
- Fang T., Gao J., Wu Q., Xie C., Zhang Y., et al. Digital workflow of labial templates for alveolar ridge reduction during implant–supported full–arch rehabilitation. J Prosthodont. 2023. [PubMed.]
- Mijiritsky E., Ben Zaken H., Shacham M., Cinar IC., Tore C., et al. Variety of surgical templates and protocols for bone reduction prior to implant placement:A narrative review. Int J Environ Res Public Health. 2021;18(5):2341. [PubMed.]
- Cushen SE., Turkyilmaz I. Impact of operator experience on the accuracy of implant placement with stereolithographic surgical templates:an in vitro study. J Prosthet Dent. 2013;109(4):248–254. [PubMed.]
- Testori T., Weinstein T., Scutellà F., Wang HL., Zucchelli G. Implant placement in the esthetic area:Criteria for positioning single and multiple implants. Periodontol 2000. 2018;77(1):176–196. [PubMed.]
- Kan JYK., Rungcharassaeng K., Deflorian M., Weinstein T., Wang HL., et al. Immediate implant placement and provisionalization of maxillary anterior single implants. Periodontol 2000. 2018;77(1):197–212. [PubMed.]
- Ferrara A., Galli C., Mauro G., Macaluso GM. Immediate provisional restoration of postextraction implants for maxillary single–tooth replacement. Int J Periodontics Restorative Dent. 2006;26(4):371–377. [PubMed.]
- Kang SJ., Shin SI., Herr Y., Kwon YH., Kim GT., et al. Anatomical structures in the maxillary sinus related to lateral sinus elevation:A cone beam computed tomographic analysis. Clin Oral Implants Res. 2013;24(Suppl A100):75–81. [PubMed.]
- Wen SC., Chan HL., Wang HL. Classification and management of antral septa for maxillary sinus augmentation. Int J Periodontics Restorative Dent. 2013;33(4):509–517. [PubMed.]
- Capetillo JF., Johnson TM., Swenson DT., Herold RW. Managing Antral Wall Discontinuities in Sinus Elevation Surgery. Clin Adv Periodontics. 2021;11(1):27–32. [PubMed.]
- Akers JA., Johnson TM., Wagner JC., Vargas SM., Colamarino AN., et al. Dental implants at sites of focal high and mixed density osseous lesions:Treatment strategies. Clin Adv Periodontics. 2023;13(2):115–129. [PubMed.]
- Vargas SM., Dimalanta WG., Johnson TM. Guided protocol for indirect fabrication of a custom provisional restoration prior to immediate implant surgery in the esthetic zone. Clin Adv Periodontics. 2023;13(4):217–226. [PubMed.]