>Corresponding Author : Joseph M Jankovich
>Article Type : Case Report
>Volume : 4 | Issue : 2
>Received Date : 02 March, 2024
>Accepted Date : 13 March, 2024
>Published Date : 17 March, 2024
>DOI : https://doi.org/10.54289/JDOE2400107
>Citation : Jankovich JM, Brockway DJ, Inouye KA, Millan CP, Lincicum AR, et al. (2024) Attachment Loss Attributable to Third Molar Malposition/Extraction: The Case for Classification 4(2): doi https://doi.org/10.54289/JDOE2400107
>Copyright : © 2024 Jankovich JM, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Case Report Article | Open Access | Full Text
1Department of Periodontics, Army Postgraduate Dental School, Postgraduate Dental College, Fort Eisenhower, GA, USA
2Private practice, Lowcountry Periodontics and Dental Implants, Hilton Head Island, SC, USA
*Corresponding author: Joseph M Jankovich, Department of Periodontics, Army Postgraduate Dental School, Postgraduate Dental College, Fort Eisenhower, GA, USA
Abstract
Background: The 2017 World Workshop on the Classification of Periodontal and Peri-implant Diseases and Conditions established a periodontitis staging and grading scheme that—for the first time—integrates an assessment of disease severity with an appraisal of therapeutic complexity and risk for disease progression. Individuals exhibiting attachment loss attributable to third molar malposition or extraction represent a large cohort of non-periodontitis patients highly likely to respond favorably to treatment. The purpose of this clinical report is to illustrate the value in formally categorizing this common periodontal condition.
Case Description: Two male patients were referred to the Department of Periodontics, Army Postgraduate Dental School, for evaluation of bone and attachment loss limited to distal surfaces of mandibular second molars. Each patient was treated using a combination of guided tissue regeneration and bone replacement grafts. Favorable clinical and radiographic outcomes were observed over follow-up periods ranging from 4 months to 4 years.
Practical Implications: Many patients experiencing bone and attachment loss attributable to third molar malposition or extraction lack periodontitis risk factors/indicators, have low susceptibility to the disease, and are highly likely to respond favorably to treatment. Future classification systems of periodontal diseases and conditions should formally categorize this commonly encountered periodontal condition.
Keywords: Third Molar; Periodontitis; Clinical Protocols; Regeneration; Allografts; Treatment Outcome
Abbreviations: BOP: Bleeding on Probing, PD: Probing Depths, GTR: Guided Tissue Regeneration, BRG: Bone Replacement Graft
Introduction
In 2017, the World Workshop on the Classification of Periodontal and Peri-implant Diseases and Conditions addressed multiple faults and limitations of the previous classification system [1,2]. Among other advancements, the workshop produced a new multidimensional periodontitis staging and grading system which aligned more closely with emerging research on periodontitis etiology and pathogenesis and an updated understanding of relevant local and systemic risk factors/indicators [1,3]. Given the complexity of periodontitis, it may be unsurprising that experienced clinicians demonstrate only moderate concordance when applying the new staging and grading criteria [4]. A predominant factor accounting for the variance in periodontitis classification among trained practitioners has been the discernment of “gray zones” within the 2017 system, which multiple authors have sought to clarify [5-7]. One focus of the clarification has been distinguishing periodontitis cases bordering between Stages III and IV, a task that often requires interpretation and integration of a broad collection of historical, clinical, and radiographic parameters [5-7]. Other examples of gray zones that require the subjective clinical judgement of a trained practitioner for proper classification include slight attachment loss in an older, radiographically intact patient lacking clinical signs of inflammation, localized periodontitis at single site, and cases compelling the clinician to “overrule” the staging algorithm despite the presence or absence of certain complexity factors [7].
Under the current classification system, clinical attachment loss attributable to third molar malposition or extraction is expressly excluded from the periodontitis case definition [3]. Indeed, periodontitis must be differentiated from conditions such as gingivitis, trauma-induced recession, vertical root fracture, cervical caries, necrotizing periodontal diseases, periodontal abscesses, and endo-periodontal lesions [3,8]. Workshop panelists recognized that conditions other than periodontitis present with loss of clinical attachment. Thus, adoption of the 2017 classification system appropriately excluded multiple groups of patients who, under the 1999 system, would have been classified within the periodontitis category [9]. In perspective, third molar malposition /impaction is extremely common, and impacted third molar extraction ranks among the most frequent procedures in oral and maxillofacial surgery [10,11]. Adjacent second molars commonly exhibit bone and attachment loss following third molar surgery; the ensuing defects may present with radiographic calculus, bleeding on probing (BOP), deep probing depths (PDs), and tooth mobility [10,11]. Periodontal lesions of this type require treatment, and the distinct etiology of these defects has relevant prognostic and therapeutic implications. The objectives of this report are to present two cases of clinical attachment loss attributable to third molar malposition/extraction, highlight similarities and differences of this condition in comparison with periodontitis, and articulate rationale for formally categorizing this common case type.
Case Descriptions
Both patients described in this report presented to the Department of Periodontics, Army Postgraduate Dental School, Post Graduate Dental College, Uniformed Services University, Fort Eisenhower, Georgia, for evaluation of bone and attachment loss on the distal surfaces of the mandibular second molars attributable to third-molar malposition/extraction. Neither patient reported any systemic disease or condition, and both denied taking any medications. In addition, neither patient had ever used any tobacco product. Each patient received a detailed explanation of the attachment loss etiology and all available treatment options. Both patients elected a combination of guided tissue regeneration (GTR) and bone replacement graft (BRG) at the distal surfaces of affected mandibular second molars. Each patient completed an informed consent process consisting of verbal and written components.
Case 1
In February of 2023, a healthy male aged 34 years was referred for evaluation of bone and attachment loss on the distal surfaces of the teeth #18 and 31 (Figures 1-3). The patient’s third molars had been extracted at age 23. On examination, the modified O’Leary plaque index [12] was 90%, and the gingiva appeared pink and firm throughout, with minimal marginal erythema noted at the lingual and palatal aspects of molar areas. BOP was noted at 9% of sites. Isolated 4-mm PDs were recorded in posterior sextants, with 8- through 10-mm PDs limited to the distal surfaces of the mandibular second molars. The patient was diagnosed with gingival excess manifesting as pseudopocketing and excessive gingival display, and the clinical attachment loss on the distal surfaces of mandibular second molars was attributed to third molar malposition/extraction.

Figure 1: Case 1. Baseline clinical appearance. A and B. Maximum intercuspation. C and D. Mandibular posterior sextants, buccal view. Gingival excess, manifesting as excessive gingival display and pseudopocketing, was appreciated in all sextants.
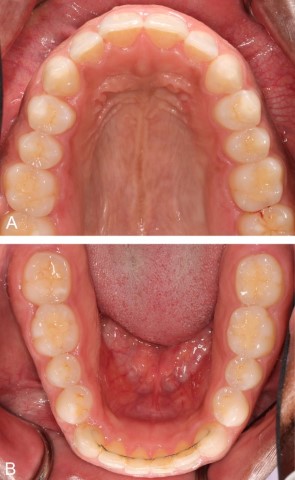
Figure 2: Case 1. Baseline clinical appearance, maxillary and mandibular occlusal views.
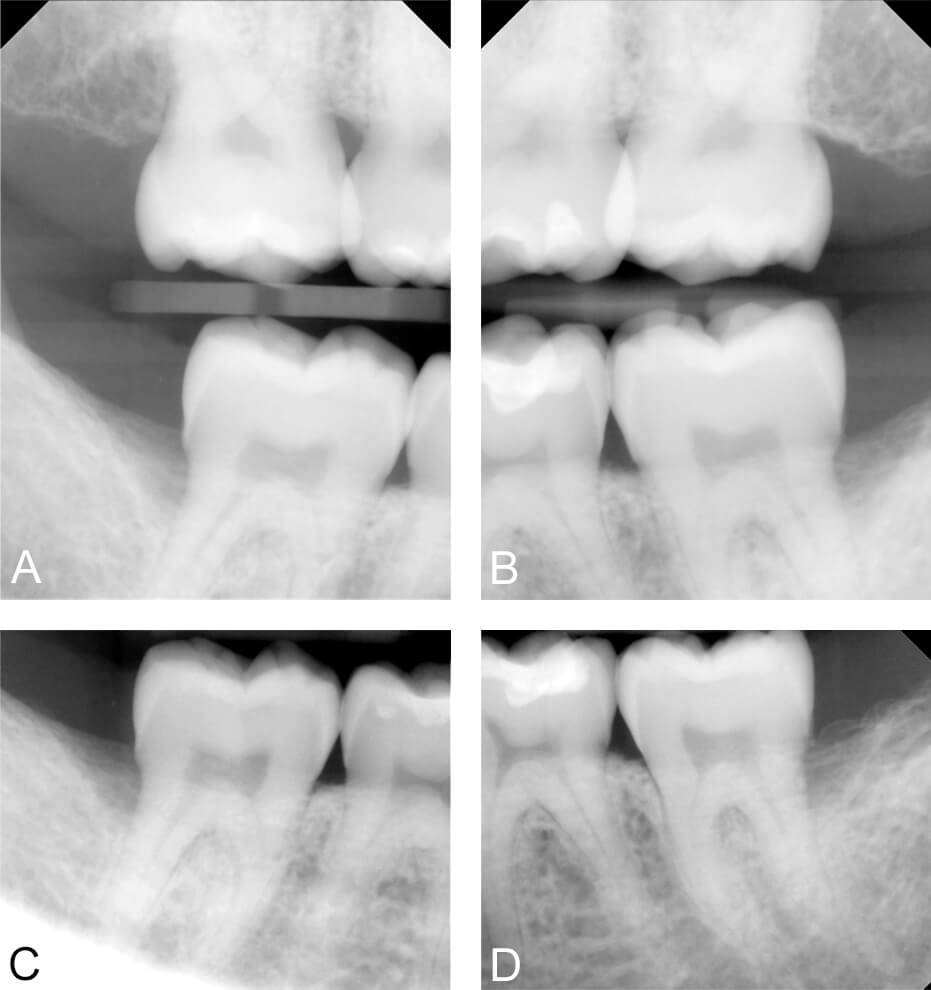
Figure 3: Case 1. Baseline radiographic appearance. A and B. Vertical bite-wing radiographs. C and D. Periapical radiographs. Wide, deep infrabony defects were appreciated at the distal surfaces of teeth #2, 18, and 31.
After nonsurgical therapy and re-evaluation, the two sites were treated in separate procedures. Full thickness mucoperosteal flaps were reflected to permit defect access and visualization (Figure 4). Crestal 1-wall components of the osseous defects were reduced [13]. Root surfaces were thoroughly debrided with ultrasonic and hand instruments, then treated with a tetracycline hydrochloride solution (100 milligrams per milliliter) [14]. A solvent-dehydrated bone allograft was applied in each defect, then covered with an amnion-chorion membrane [15,16]. Wound closure for primary intention healing was achieved with simple interrupted sutures (Figure 5). Toothbrushing at the surgical sites was withheld for three weeks, and a 0.12% chlorhexidine mouth rinse was used for plaque control until the patient’s normal oral hygiene regimen could be reinstated. Ibuprofen (400 mg) and acetaminophen (325 mg) were utilized as needed for analgesia.
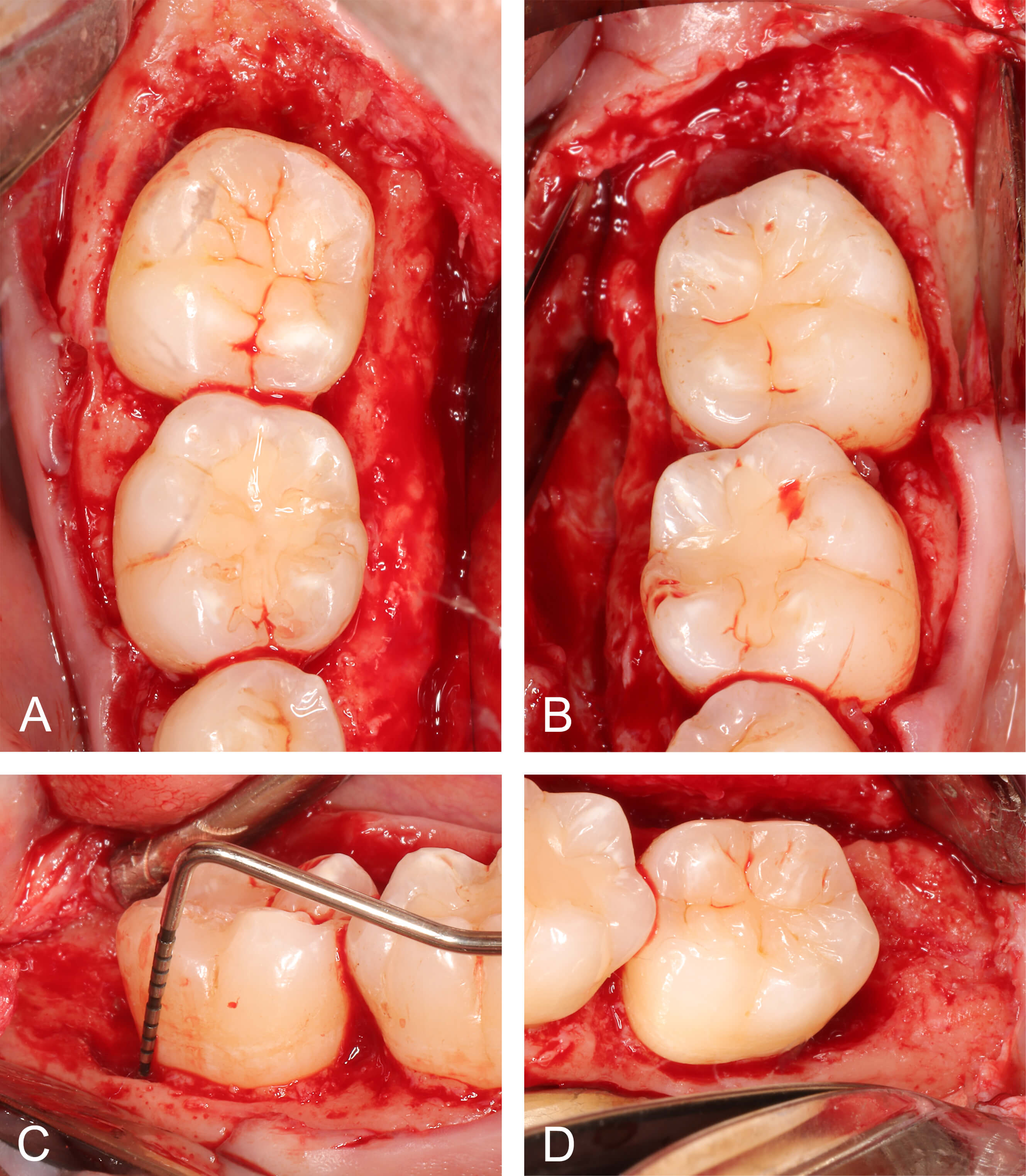
Figure 4: Case 1. Appearance of intrabony defects at distal surfaces of mandibular second molars following mucoperiosteal flap reflection. A and B. Occlusal views. C and D. Buccal views. Each defect measured > 5 mm at the deepest extent. Minimal osteoplasty was performed to eliminate the 1-wall component of each defect. Following osteoplasty, each defect exhibited a 3-wall configuration.
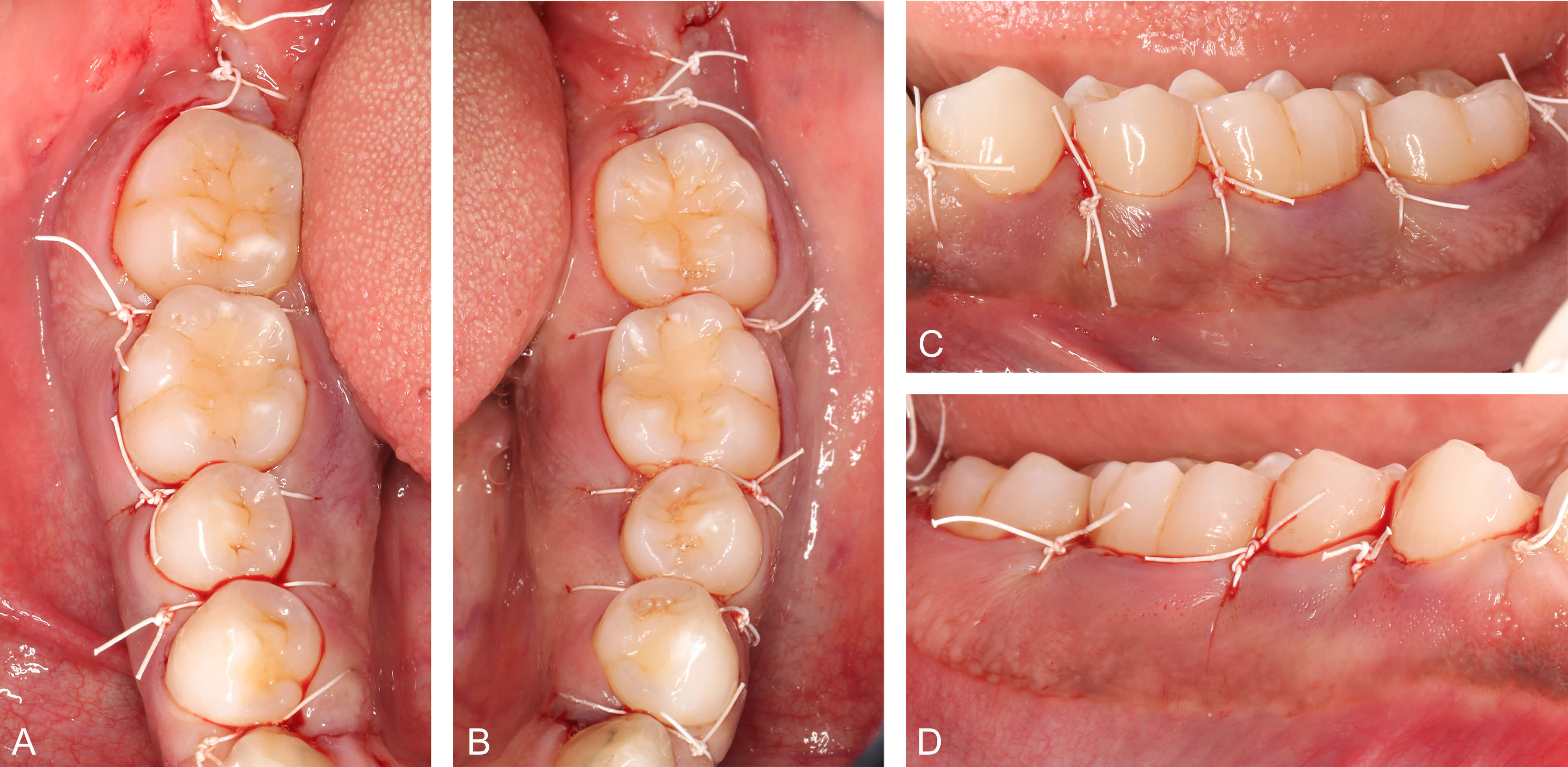
Figure 5: Case 1. Appearance of intrabony defects at distal surfaces of mandibular second molars following mucoperiosteal flap reflection. A and B. Occlusal views. C and D. Buccal views. Each defect measured > 5 mm at the deepest extent. Minimal osteoplasty was performed to eliminate the 1-wall component of each defect. Following osteoplasty, each defect exhibited a 3-wall configuration.
The early postoperative period was uneventful following each procedure. Follow-up assessments at 5 months (tooth #18) and 4 months (tooth #31) revealed favorable radiographic bone fill (Figure 6) and improvements in clinical parameters. PDs at distal surfaces of teeth #18 and 31 were reduced to 3 through 4 mm with no BOP (Figure 7).
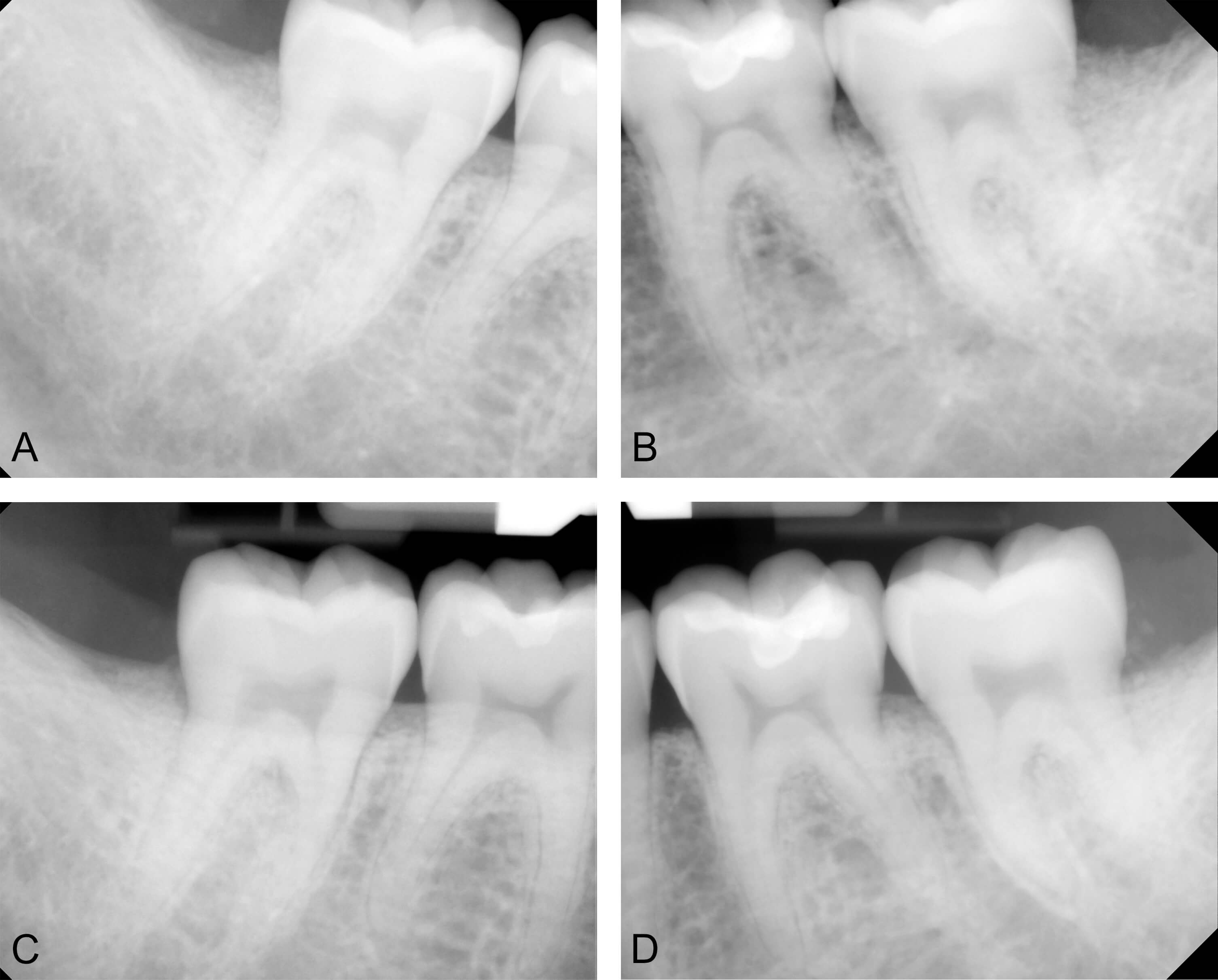
Figure 6: Case 1. Follow-up radiographic assessment. A and B. Immediate postoperative radiographic appearance after application of solvent-dehydrated bone allografts. C. Postoperative month 5, tooth #31 area. D. Postoperative month 4, tooth #18 area.

Figure 7: Case 1. Follow-up clinical assessment. A and C. Postoperative month 5, tooth #31 area. B and D. Postoperative month 4, tooth #18 area.
Case 2
In June of 2019, a male patient aged 34 years presented for evaluation of bone and attachment loss on the distal surface of tooth #31. The patient had a history of horizontally impacted mandibular third molars, which were extracted at age 29. On examination, the gingiva was generally pink and firm, with localized erythema, edema, bleeding, and suppuration at tooth #31. The modified O’Leary plaque index was 88%, and full-mouth BOP was < 10%. Isolated 4-mm PDs were noted on the lingual aspect of mandibular molars, with 10- through 12-mm PDs at the distal surface of tooth #31. Panoramic and intraoral radiographs revealed a distal infrabony defect extending to the apex of tooth #31. Tooth #31 responded normally to sensibility testing, and no fracture was detected. As in Case 1, the patient was diagnosed with pseudopocketing, and the clinical attachment loss at the distal surface of tooth #31 was attributed to third-molar malposition/extraction.
Following nonsurgical therapy, the infrabony periodontal defect was treated surgically in the manner described in Case 1. After 4 years, residual PDs at the distal of tooth #31 were ≤ 4 millimeters with no BOP, and favorable radiographic bone fill was noted (Figure 8).
Discussion
The aim of this report was to contrast periodontitis with clinical attachment loss attributable to third molar malposition/extraction. Classic animal and human studies have firmly established that periodontitis susceptibility varies widely within the population due to an array of genetic, epigenetic, microbial, behavioral, and environmental factors [17-21]. Although third-molar-related defects can be found in periodontitis patients, a large proportion of individuals experiencing attachment and bone loss on distal surfaces of second molars undoubtedly have low periodontitis susceptibility. Importantly, these patients initially lose bone and clinical attachment due to anatomic, developmental, and iatrogenic factors rather than an inflammatory response to periodontal pathogens. Moreover, mandibular anatomy in the third molar area often leads to a three-wall defect configuration, which is favorable for regenerative periodontal therapy (Figure 4) [22].
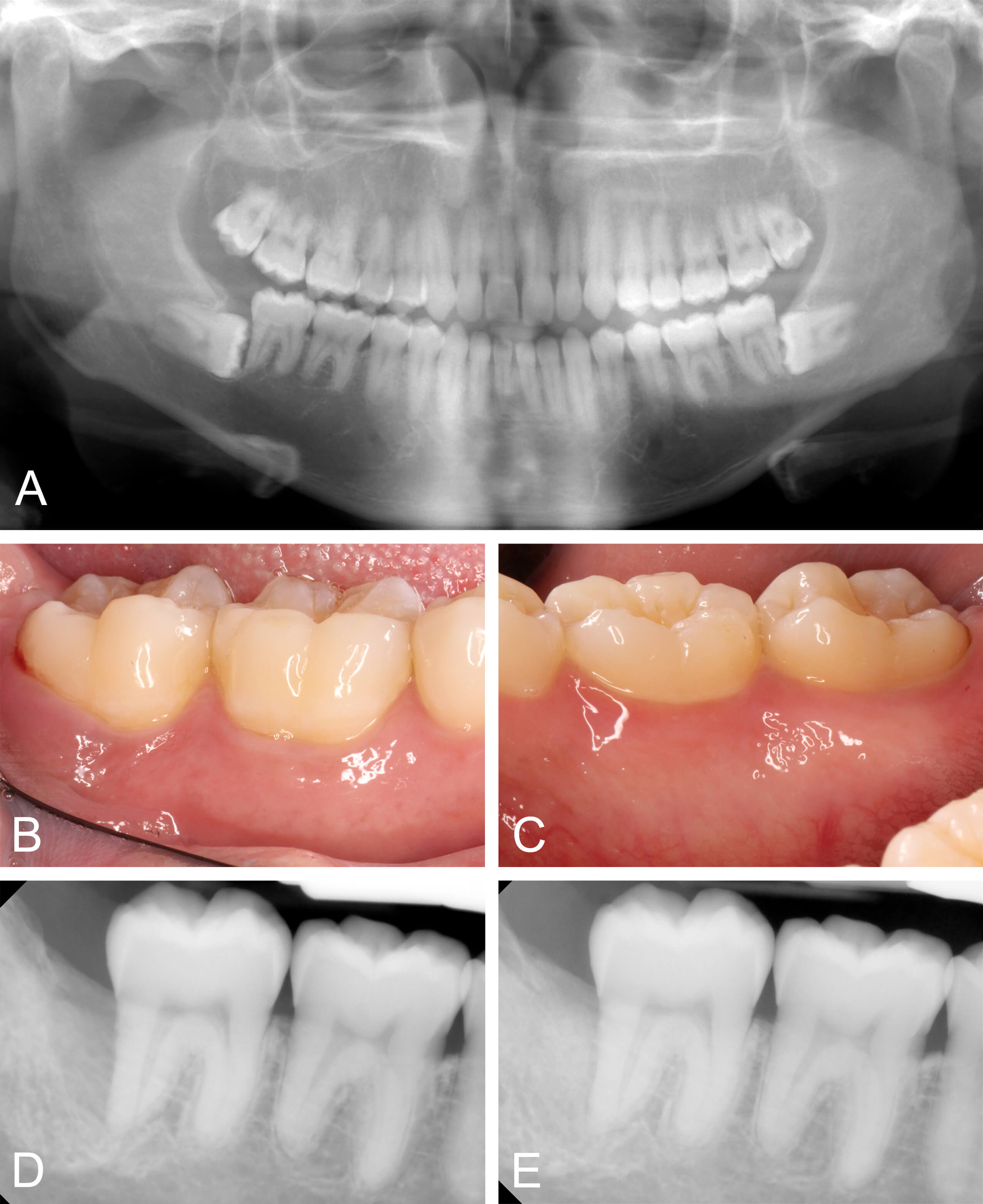
Figure 8: Case 2. A. Panoramic radiograph prior to extraction of horizontally impacted third molars (patient age 29). B and C. Baseline clinical appearance upon periodontal evaluation (patient age 34). D. Radiographic appearance four years following guided tissue regeneration and bone replacement graft.
In contrast to prior classification systems, the 2017 system goes beyond merely stratifying the severity of periodontal tissue destruction at presentation. The current staging and grading scheme integrates disease severity with an assessment of therapeutic complexity as well as risk for disease progression [1-3]. By accounting for complexity and risk, the current system improves the ability of a knowledgeable clinician to individualize care and optimize treatment. Toward that end, future iterations of the classification system should specifically categorize “Clinical Attachment Loss Attributable to Third Molar Malposition or Extraction” within the “Other Conditions Affecting the Periodontium” domain. Currently, this category is implied within the World Workshop proceedings but does not formally comprise a distinct category in the classification scheme [1,3]. Moreover, this condition is not included as a differential diagnosis for patients presenting with clinical attachment loss, although clinicians must rule-out third-molar-related attachment loss when diagnosing periodontitis [23]. Establishing this category would 1) clarify to the dental community, allied health professionals, insurers, and patients that surgical treatment is necessary despite lack of a periodontitis diagnosis and 2) identify a large group of patients with low periodontitis risk and high potential for a favorable therapeutic outcome.
Establishing and explaining the proposed category would also serve to clarify the periodontal status of patients in this group, which can be confusing. For example, under the 1999 classification system, the patients presented herein would have been diagnosed with localize severe chronic periodontitis, based on isolated sites exhibiting clinical attachment loss greater than five millimeters. Interestingly, under the current system, these patients fulfill the case definition of neither periodontitis nor gingivitis, the later requiring BOP at ≥ 10% of sites [24]. For many stakeholders, it may be counterintuitive that regenerative periodontal surgery should be so clearly indicated for a patient who has not received a periodontitis diagnosis.
Conclusion
Many individuals presenting with clinical attachment loss attributable to third molar malposition or extraction lack risk factors for periodontal disease and are highly likely to respond favorably to therapy. Based on the high incidence of third molar impaction/malposition, and the high frequency of third molar surgery worldwide, formally establishing a category for the case type described in this report appears warranted and clinically valuable.
Author contributions: All authors have contributed substantially to conceptualization of this report, drafting the article, critical review, and editing. All authors have approved the final version of the manuscript.
Conflicts of interest: The authors report no financial, economic, or professional interests that may have influenced the design, execution, or presentation of this work.
Disclaimers: The views expressed in this manuscript are those of the authors and do not necessarily reflect the official policy of the United States Government, the Department of Defense, the Defense Health Agency, or Uniformed Services University of the Health Sciences.
Funding: The Defense Health Agency funded this research entirely. The authors received no extramural funding.
References
- Caton JG., Armitage G., Berglundh T., Chapple ILC., Jepsen S., et al. A new classification scheme for periodontal and peri–implant diseases and conditions – Introduction and key changes from the 1999 classification. J Periodontol. 2018;89(Suppl 1):S1–S8. [PubMed.]
- Papapanou PN., Sanz M., Buduneli N., Dietrich T., Feres M., et al. Periodontitis:Consensus report of workgroup 2 of the 2017 World Workshop on the Classification of Periodontal and Peri–Implant Diseases and Conditions. J Periodontol. 2018;89(Suppl 1):S173–S182. [PubMed.]
- Tonetti MS., Greenwell H., Kornman KS. Staging and grading of periodontitis:Framework and proposal of a new classification and case definition. J Periodontol. 2018;89(Suppl 1):S159–S172. [PubMed.]
- Ravidà A., Travan S., Saleh MHA., Greenwell H., Papapanou PN., et al. Agreement among international periodontal experts using the 2017 World Workshop classification of periodontitis. J Periodontol. 2021;92(12):1675–1686. [PubMed.]
- Steigmann L., Sommer C., Kornman KS., Wang HL. Staging and Grading Discussion of Borderline Cases in Gray Zones. Clin Adv Periodontics. 2021;11(2):98–102. [PubMed.]
- Sirinirund B., Di Gianfilippo R., Yu SH., Wang HL., Kornman KS. Diagnosis of Stage III Periodontitis and Ambiguities of the "Gray Zones" in Between Stage III and Stage IV. Clin Adv Periodontics. 2021;11(2):111–115. [Ref.]
- Kornman KS., Papapanou PN. Clinical application of the new classification of periodontal diseases:Ground rules., clarifications and "gray zones". J Periodontol. 2020;91(3):352–360. [Ref.]
- Sanz M., Herrera D., Kebschull M., Chapple I., Jepsen S., et al. Treatment of stage I–III periodontitis–The EFP S3 level clinical practice guideline. J Clin Periodontol. 2020;47(Suppl 22):4–60. [PubMed.]
- Armitage GC. Development of a classification system for periodontal diseases and conditions. Ann Periodontol. 1999;4(1):1–6. [PubMed.]
- Zhang Y., Chen X., Zhou Z., Hao Y., Li H., et al. Effects of Impacted Lower Third Molar Extraction on Periodontal Tissue of the Adjacent Second Molar. Ther Clin Risk Manag. 2021;17:235–247. [PubMed.]
- Ye ZX., Qian WH., Wu YB., Yang C. Pathologies associated with the mandibular third molar impaction. Sci Prog. 2021;104(2):368504211013247. [PubMed.]
- O'Leary TJ., Drake RB., Naylor JE. The plaque control record. J Periodontol. 1972;43(1):38. [PubMed.]
- Ochsenbein C. Combined approach to the management of intrabony defects. Int J Periodontics Restorative Dent. 1995;15(4):328–343. [PubMed.]
- Mariotti A. Efficacy of chemical root surface modifiers in the treatment of periodontal disease. A systematic review. Ann Periodontol. 2003;8(1):205–226. [PubMed.]
- Tsao YP., Neiva R., Al‐Shammari K., Oh TJ., Wang HL. Effects of a mineralized human cancellous bone allograft in regeneration of mandibular Class II furcation defects. J Periodontol. 2006;77(3):416–425. [PubMed.]
- Holtzclaw DJ., Toscano NJ. Amnion–chorion allograft barrier used for guided tissue regeneration treatment of periodontal intrabony defects:A retrospective observational report. Clin Adv Periodontics. 2013;3(3):131–137. [Ref.]
- Lindhe J., Hamp SE., Löe H. Plaque induced periodontal disease in beagle dogs. A 4–year clinical., roentgenographical and histometrical study. J Periodontal Res. 1975;10(5):243–255. [PubMed.]
- Löe H., Anerud A., Boysen H., Smith M. The natural history of periodontal disease in man. The rate of periodontal destruction before 40 years of age. J Periodontol. 1978;49(12):607–620. [PubMed.]
- Löe H., Anerud A., Boysen H., Morrison E. Natural history of periodontal disease in man. Rapid., moderate and no loss of attachment in Sri Lankan laborers 14 to 46 years of age. J Clin Periodontol. 1986;13(5):431–445. [PubMed.]
- Neely AL., Holford TR., Löe H., Anerud A., Boysen H. The natural history of periodontal disease in man. Risk factors for progression of attachment loss in individuals receiving no oral health care. J Periodontol 2001;72(8):1006–1015. [PubMed.]
- Hajishengallis G., Chavakis T., Lambris JD. Current understanding of periodontal disease pathogenesis and targets for host–modulation therapy. Periodontol 2000. 2020;84(1):14–34. [PubMed.]
- Nibali L., Sultan D., Arena C., Pelekos G., Lin GH., et al. Periodontal infrabony defects:Systematic review of healing by defect morphology following regenerative surgery. J Clin Periodontol. 2021;48(1):100–113. [PubMed.]
- Sanz M., Herrera D., Kebschull M., Chapple I., Jepsen S., et al. Treatment of stage I–III periodontitis–The EFP S3 level clinical practice guideline. J Clin Periodontol. 2020;47(Suppl 22):4–60. [PubMed.]
- Chapple ILC., Mealey BL., Van Dyke TE., Bartold PM., Dommisch H., et al. Periodontal health and gingival diseases and conditions on an intact and a reduced periodontium:Consensus report of workgroup 1 of the 2017 World Workshop on the Classification of Periodontal and Peri–Implant Diseases and Conditions. J Periodontol. 2018;89(Suppl 1):S74–S84. [PubMed.]