>Corresponding Author : Thomas M Johnson
>Article Type : Case Series
>Volume : 3 | Issue : 1
>Received Date : 17 Nov, 2023
>Accepted Date : 30 Nov, 2023
>Published Date : 05 Dec, 2023
>DOI : https://doi.org/10.54289/JDOE2300103
>Citation : Lincicum AR, Capetillo JF, Vargas SM, Smallidge MJ, McLaughlin JB, et al. (2023) Dental Implant Treatment Planning in the Post-Traumatic Rehabilitation of the Anterior Maxilla: A Report of Three Cases. J Dent Oral Epidemiol 3(1): doi https://doi.org/10.54289/JDOE2300103
>Copyright : © 2023 Lincicum AR, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Case Series | Open Access | Full Text
1Department of Periodontics, Army Postgraduate Dental School, Postgraduate Dental College, Uniformed Services University, Fort Eisenhower, GA, USA
2Department of Periodontics, 618th Medical Company (Dental Area Support), Camp Humphreys, South Korea
3Department of Periodontics, Army Postgraduate Dental School, Postgraduate Dental College, Uniformed Services University, Fort Liberty, NC, USA
4Medical Capability Development Integration Directorate, U.S. Army Futures Command, San Antonio, TX, USA
5Private Practice, Middle Tennessee Prosthodontics, Brentwood, TN, USA
6Private Practice, Elite Endodontics, Pensacola, FL, USA
7Department of Endodontics, United States Army Dental Activity, Fort Meade, MD, USA
8Department of Prosthodontics, United States Army Dental Activity, Fort Stewart, GA, USA
9Department of Endodontics, Army Postgraduate Dental School, Postgraduate Dental College, Uniformed Services University, Joint Base Lewis-McChord, WA, USA
*Corresponding author: Thomas M Johnson, Department of Periodontics, Army Postgraduate Dental School, Postgraduate Dental College, Uniformed Services University, Fort Eisenhower, GA, USA
Abstract
Evidence-based algorithms guiding treatment of traumatic dentoalveolar injuries prescribe specific interventions in the presence of various sets of historical and clinical cues. However, the staging of dental implant placement in post-traumatic rehabilitation—indeed, whether to consider implant therapy at all—remains more art than science, prior authors cautioning that universal rules do not apply. The purpose of this report is to present treatment approaches applied in three traumatic episodes involving the anterior maxilla. Three patients presented to the Department of Periodontics, Army Postgraduate Dental School, Postgraduate Dental College, Fort Eisenhower, GA, USA, following traumatic injuries to the anterior maxilla with varying degrees of severity. In two cases, central incisors were replaced using immediate implants and immediate provisionalization (IIPP). At one IIPP site, extraction was delayed for eight weeks to permit healing of an alveolar fracture. In the third case, the patient received a non-implant rehabilitation due to severe alveolar destruction.
Both patients receiving IIPP expressed satisfaction with immediate esthetics, and in both cases, the provisional restoration prevented extraction-related soft tissue collapse. Trauma adds an element of uncertainty to the technically demanding task of implant placement in the esthetic zone. When appropriate, IIPP in the post-traumatic rehabilitation of the anterior maxilla may mitigate some of the known biopsychosocial consequences of oral trauma and facilitate development of favorable mucosal and osseous architecture at the site. Individualized treatment planning is critically important due to wide variability in site characteristics and injury complexity.
Keywords: Dental Implants; Clinical Protocols; Alveolar Process; Wounds and Injuries; Dental Anxiety; Treatment Outcome
Abbreviations: IIPP: Immediate Implants and Immediate Provisionalization, AAE: American Association of Endodontists, IADT: International Association of Dental Traumatology, PRICE: Preferred Reporting Items For Case Reports in Endodontics, CBCT: Cone-Beam Computed Tomography, IIPP: Implant Placement And Immediate Provisionalization, FDBA: Freeze-Dried Bone Allograft, ARP: Alveolar Ridge Preservation, OMS: Oral and Maxillofacial Surgery, TBI: Traumatic Brain Injury
Introduction
Although the oral cavity represents only one percent of total body volume, oral trauma accounts for almost five percent of all injuries [1]. Severe trauma to the anterior maxilla predictably leads to a cascade of negative biopsychosocial consequences in both children and adults [2-14]. In contrast to caries or periodontitis, an oral traumatic episode commonly involves sudden, unexpected, severe pain under disorienting and distressing circumstances. Emergency treatment can be painful or otherwise unpleasant, potentially leading to anxiety and dental avoidance [6,15,16]. Apart from obvious financial concerns, patients experiencing oral trauma may sacrifice substantial time away from work or school. Treatment of 111 traumatized incisors in an educational setting required a median of eight visits over a median period of 21 months [17]. Trauma resulting in anterior tooth loss, or a comparable esthetic deficiency, may diminish confidence and produce a sense of bereavement [6,9,18]. Indeed, smile and facial attractiveness are strongly associated, the later influencing social interaction, personality, employment opportunities, and performance [18-22]. Female patients with esthetic defects in anterior teeth may be especially likely to experience negative emotions and feelings of insecurity [23]. Among elderly patients, presence of an unfilled anterior space has been shown to affect oral health-related quality of life more than having few (zero to three) posterior occluding pairs [13-24].
Oral trauma patients and their dental healthcare providers are fortunate that the American Association of Endodontists (AAE) and the International Association of Dental Traumatology (IADT) have established evidence-based algorithms for immediate/urgent management of dental and alveolar fractures, luxation injuries, and avulsions [25-28]. However, beyond the acute phase, many patients experiencing oral trauma require secondary and tertiary interventions [26]. Current dental trauma guidelines offer only cursory suggestions regarding the use and sequencing of dental implants [25-28]. Moreover, a recent systematic review of implant treatment after traumatic tooth loss did not include any reports involving immediate implant surgery [29]. Schwartz-Arad and Levin performed a retrospective analysis of 53 patients, each receiving an implant to replace a maxillary anterior tooth lost due to trauma [30]. Twenty-five of the patients received immediate implants [30]. In this study, timing of placement was unrelated to complication occurrence or implant failure [30]. Scrupulous assessment and individualized treatment planning appeared essential, the authors cautioning in two publications that “general rules do not apply” [30,31]. Given the lack of research informing clinical decision-making in post-traumatic dental implant placement, the purpose of this report is to present treatment approaches applied in three anterior maxilla trauma cases.
Case descriptions
This report complies with the 2020 Preferred Reporting Items for Case reports in Endodontics (PRICE) guidelines [32]. Patients described in this report were evaluated and treated in the Department of Periodontics, Army Postgraduate Dental School, Postgraduate Dental College, Fort Eisenhower, GA, USA. Each patient completed an informed consent process involving verbal and written components prior to treatment. All cone-beam computed tomography (CBCT) images in this report were acquired using a single scanner (3D Accuitomo 170, J. Morita, Kyoto, Japan) and evaluated using the system software (i-Dixel, version 2.3.0.3, J. Morita). In each case, CBCT imaging was indicated to assess dental and/or alveolar fractures. Brightness and contrast were adjusted to improve fracture detection, and slices in the axial, sagittal, and coronal planes were viewed at varying levels of magnification (up to 400%) within the software.
Case 1
In April of 2016, a healthy White male, aged 29 years, experienced trauma to the anterior maxilla after falling while running with a military rifle. The patient’s chief complaint was pain from the maxillary anterior teeth on the right side. Examination revealed fracture of the maxillary right lateral incisor involving enamel and dentin, with pulp exposure. The adjacent central incisor exhibited a crown fracture extending subgingivally onto the palatal root surface. Both teeth exhibited sensitivity to stimuli and normal mobility. A CBCT volume confirmed intact alveolar bone and no additional root fractures. The patient was diagnosed with a complicated crown fracture of the maxillary right lateral incisor and a crown/root fracture of the maxillary right central incisor. The fractured teeth received root canal therapy to alleviate pain and permit time for the patient to consider treatment options, including orthodontic extrusion or crown lengthening of the maxillary right central incisor. The patient elected restoration of maxillary right lateral incisor with a post/core and crown and replacement of the adjacent central incisor using immediate implant placement and immediate provisionalization (IIPP) (Figure 1).
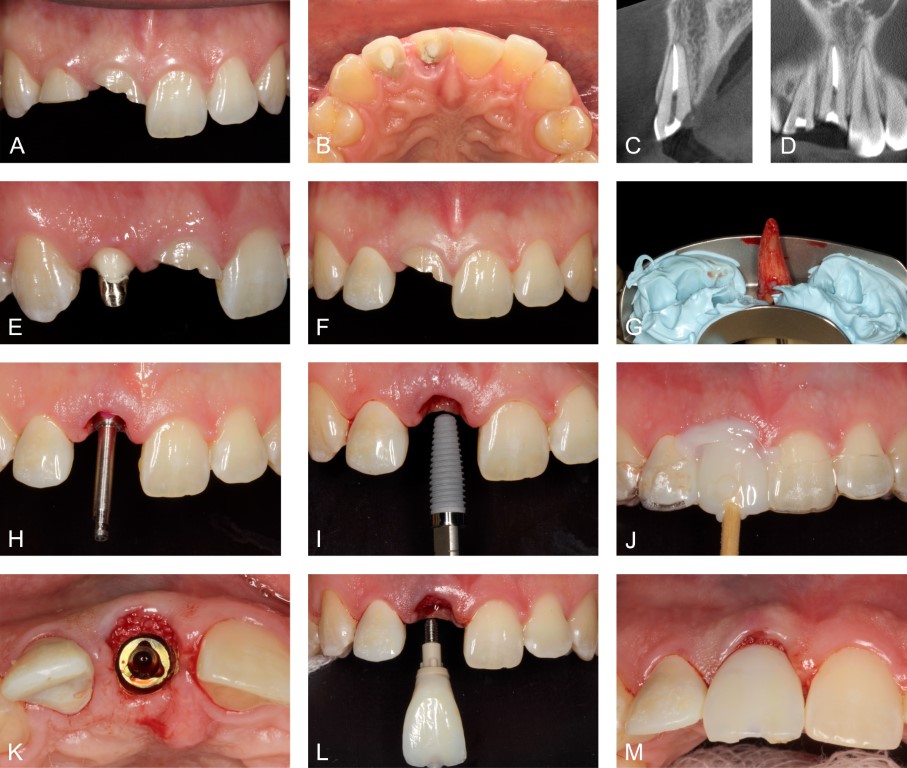
Figure 1: Case 1. Complicated crown fracture of the maxillary right lateral incisor and complicated crown/root fracture of the adjacent central incisor. A. Clinical appearance after completion of root canal therapy, facial view. B. Palatal view. C. Cone-beam computed tomography (CBCT) volume, parasagittal slice through the central incisor. Field of view 40 x 40 x 40 mm, isometric voxel size 0.08 mm, 90 kV, 5 mA, exposure time 30.8 s, arc of rotation 360 degrees. D. CBCT volume, coronal slice. E. The lateral incisor prepared for crown, cast post/core cemented. F. Provisional crown for the lateral incisor delivered prior to immediate implant placement in the central incisor position. G. Minimally traumatic extraction of the central incisor. H. Shaping drill indicating platform depth 3.5 mm apical to the midfacial peri-implant mucosa. I. Implant installation. J. Fabrication of provisional implant crown. K. Implant platform with particulate freeze-dried bone allograft (FDBA) in the peri-implant gap defect and positioned against the facial keratinized mucosa. L and M. Insertion of the provisional implant crown, sealing the socket and stabilizing particulate FDBA in the soft tissue zone.
After administration of local anesthesia, the maxillary right central incisor was extracted with minimal trauma. The walls of the alveolus remained intact. A surgical guide directed a two-millimeter twist drill for the initial osteotomy. The osteotomy was then expanded according to the surgical protocol recommended by the implant manufacturer (Nobel Biocare, Kloten, Switzerland), and a 4.3 x 13 mm implant was stabilized with an insertion torque of 50 Newton-centimeters. A provisional restoration with favorable fit and finish sealed the extraction socket after placement of a particulate freeze-dried bone allograft (FDBA) (Oragraft, LifeNet Health, Virginia Beach, VA, USA) in the peri-implant gap defect and within the soft tissue zone. The patient received ibuprofen (400 mg) and acetaminophen (325 mg) three times daily as needed for analgesia. Tooth brushing was withheld at the surgical site for two weeks, the patient utilizing chlorhexidine plaque control until his normal oral hygiene routine could be reinstated.
The patient was satisfied with immediate postoperative esthetics, and he reported minimal discomfort during early healing. At one week, the patient described no discomfort. Favorable soft tissue contours were noted, with no implant mobility and no clinical signs of inflammation (Figure 2). The next week, the patient departed the area, and we transferred care to an out-of-state practitioner for the restorative phase.
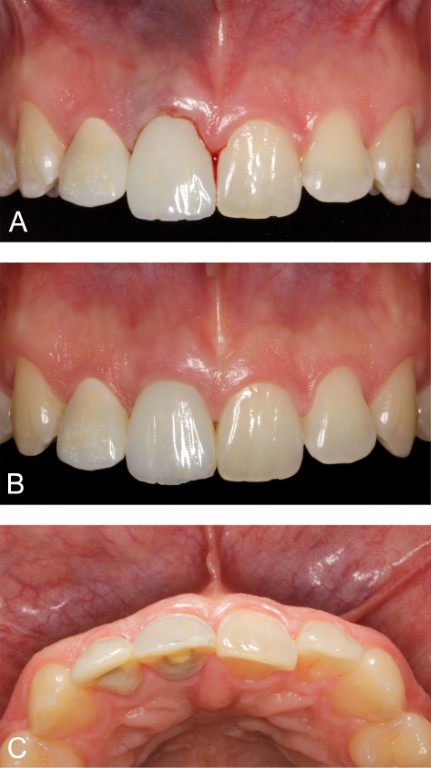
Figure 2: Case 1. Clinical appearance. A. Immediately following implant surgery. B and C. Postoperative week one, facial and palatal views, respectively.
Case 2
A White male patient, aged 43 years, presented to the emergency department in December of 2015 with blunt trauma to his face. The patient lost consciousness at a movie theater, fell forward, and struck the adjacent seat. He complained of pain, displacement of his one of his maxillary anterior teeth, and bleeding from his lips. The patient had not previously experienced loss of consciousness, and he had no systemic illnesses. Lacerations were present on the patient’s lower lip, and the maxillary left central incisor demonstrated lateral luxation. The dentist on call repositioned the tooth and applied a flexible splint to the maxillary anterior teeth. A CBCT volume revealed an alveolar fracture and an oblique middle-third root fracture of the left central incisor as well as internal root resorption of the right central incisor (Figure 3). Treatment options were explained in detail, the patient electing IIPP to replace the fractured tooth and root canal therapy for the right central incisor to arrest the resorptive process. Other management options included delayed implant placement and fixed dental prosthesis. An eight-week healing period with the flexible splint in place preceded IIPP. In addition, the patient understood that clinical inspection of the labial alveolar plate would be possible after tooth extraction and that the plan could shift to alveolar ridge preservation (ARP) with delayed implant placement if the alveolus appeared substantially compromised.
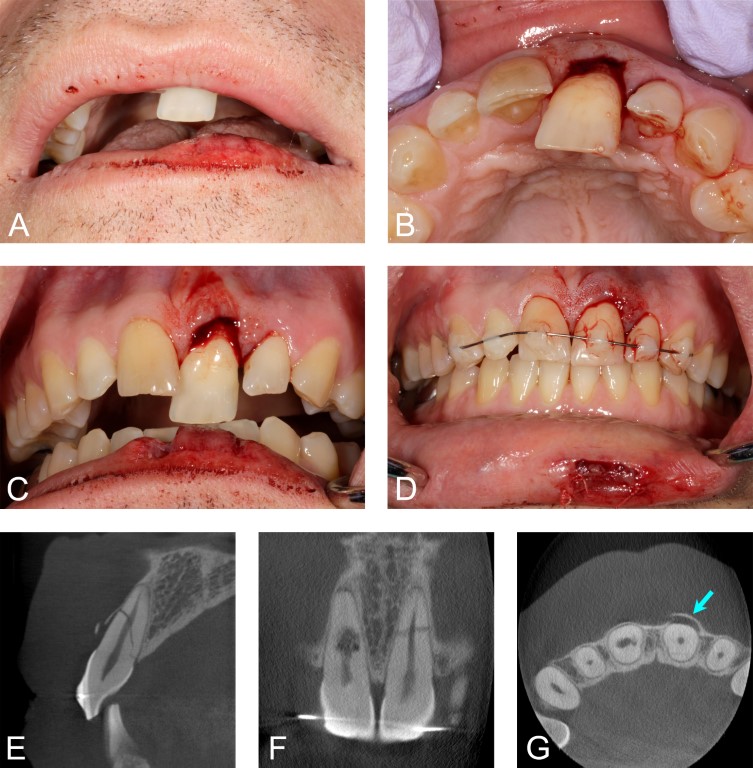
Figure 3: Case 2. This patient lost consciousness in a movie theater, fell forward, and sustained trauma to the anterior maxilla. A through C. Lateral luxation of the maxillary left central incisor. D. On an emergency basis, we repositioned the tooth, and the maxillary anterior teeth received a flexible splint. We monitored the pulpal status of the maxillary anterior teeth in the weeks following the injury. Ultimately, the right central incisor, the left lateral incisor, and the left canine received root canal therapy, with an unfavorable prognosis assigned to the left central incisor. E. Cone-beam computed tomography (CBCT), parasagittal slice through the maxillary left central incisor. Field of view 40 x 40 x 40 mm, isometric voxel size 0.08 mm, 90 kV, 5 mA, exposure time 30.8 s, arc of rotation 360 degrees. The facial cortical bone appeared fractured, with an oblique root fracture of the tooth from the palatal osseous crest to the apical third of the root on the facial aspect. F. Coronal slice demonstrating internal root resorption of the right central incisor and middle-third root fracture of the left central incisor. The patient consented to root canal therapy for the right central incisor to arrest the resorptive process. G. Axial slice. The facial alveolar bone adjacent to the left central incisor exhibited a fracture near the mesial line angle. The fractured segment remained attached on the distal aspect, with facial displacement of the alveolar bone (arrow). Due to the insult to the facial cortical bone, we permitted a healing period of eight weeks prior to immediate implant placement.
Tooth extraction, implant installation, FDBA placement, postoperative medications, and oral hygiene instructions were as described in Case 1. A 4.1 x 13 mm implant (Zimmer Biomet, Warsaw, Indiana, USA) was placed in the right central incisor position, and the provisional crown was slightly undercontoured to discourage apical migration of the marginal peri-implant mucosa (Figure 4). At completion of the surgery, labial gingival/mucosal margins in the central incisor areas were approximately symmetrical.
Early healing proceeded uneventfully without need for analgesics beyond the third postoperative day. At postoperative week two, an incisal shift was noted in the labial peri-implant mucosa—a change which remained stable at subsequent assessments. Six months following IIPP, the contours of the provisional crown were modified to improve symmetry (Figure 5). Delivery of the definitive implant-supported restoration occurred 11 months following IIPP, and a favorable esthetic result was noted at the 12-month assessment (Figure 6).
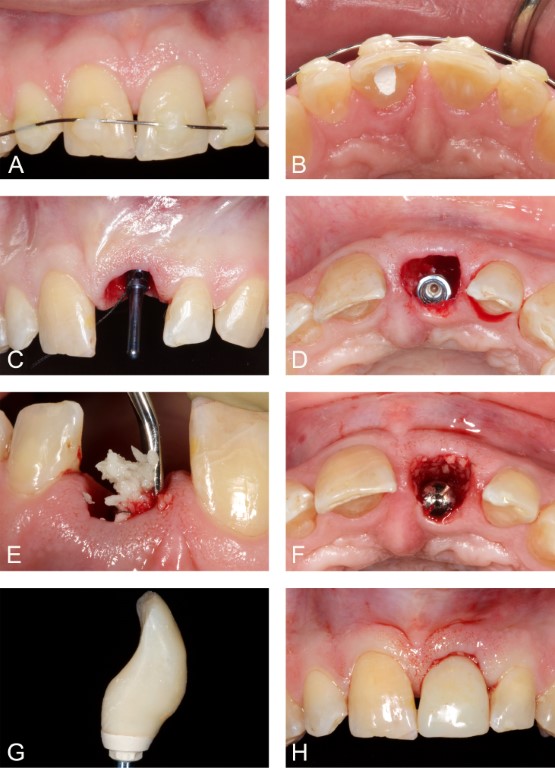
Figure 4: Case 2. Immediate implant placement with immediate provisionalization. A and B. Preoperative appearance, facial and palatal views, respectively. The right central incisor, the left lateral incisor, and the left canine had received root canal therapy prior to immediate implant surgery. C. Direction indicator in place. D. Implant stabilized in extraction socket. E. Particulate freeze-dried bone allograft (FDBA) applied in the peri-implant gap defect and the soft tissue zone. F. FDBA applied against the facial peri-implant mucosa. We used a healing abutment to exclude blood and FDBA particles from the internal aspect of the implant. G. Provisional implant crown fabricated. H. Provisional implant crown delivered.
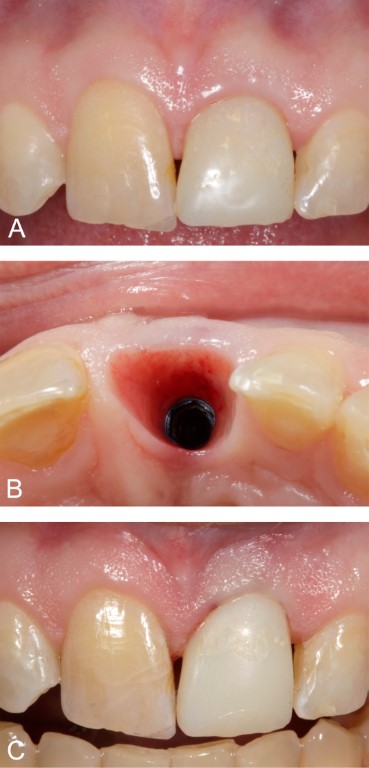
Figure 5: Case 2. Development of harmonious mucosal contours. A. Appearance at postoperative month six. The marginal peri-implant mucosa had moved in an incisal direction. We removed and recontoured the provisional crown to improve symmetry. B. Appearance of the peri-implant mucosal thickness at six months. C. Appearance after modifying the provisional crown. The marginal peri-implant mucosa exhibited temporary blanching upon delivery of the provisional crown.

Figure 6: Case 2. A. Definitive implant abutment, maxillary left central incisor position (11 months following surgery). B. Clinical appearance one year following immediate implant placement.
Case 3
In July of 2021, a healthy White male, aged 28 years, sustained repeated blows to the anterior maxilla while engaged in a hockey match. The patient lost consciousness and could not recall details of the traumatic episode. On the third day following the incident, the patient sought medical and dental care at our facility, complaining of oral pain and swelling. On examination, the patient demonstrated perioral and periorbital bruising/swelling along with cognitive symptoms. The maxillary right central incisor was missing, and the adjacent left central incisor exhibited lateral luxation with severe loss of periodontal support. After receiving extraction of the traumatized incisor, the patient became emotional. He was referred for neurologic assessment and oral and maxillofacial surgery (OMS) consultation at Dwight David Eisenhower Army Medical Center, with re-evaluation scheduled in the periodontics department. A physician diagnosed the patient with mild traumatic brain injury (TBI), and the OMS department noted a small nasal fracture, which did not require treatment.
CBCT imaging revealed severe alveolar destruction in the central incisor areas characterized by fractures of the facial, palatal, and interdental bone. Two sequestra were removed from the left central incisor area (Figure 7), the larger segment measuring ≈ 9 x 13 x 2 mm. One week later, an additional 10 x 14 x 2-mm segment of mobile, necrotic alveolar bone was removed. Restorative options were discussed in detail, including placement of a fixed dental prosthesis. The patient was advised that the sustained trauma severely compromised the site for an implant-based rehabilitation. Due to an out-of-state employment opportunity, the patient requested a temporary removable prosthesis at postoperative month two (Figure 8), stating that he planned to re-evaluate his options once established in his new occupation.
Discussion
The purpose of this report was to present treatment provided in the management of three instances of trauma to the anterior maxilla, two of the cases involving immediate implant surgery. Little more than one half century has passed since P.I. Brånemark fundamentally changed dentistry by defining osseointegration and promulgating the first reliable surgical procedure for dental implant placement [33-36]. Originally, Dr. Brånemark’s protocol required a lengthy healing period before loading, and the procedure was indicated for edentulous applications only [33-36]. Implants had to remain submerged upon wound closure, and emphasis on control of functional stresses exceeded current norms [33-36]. However, through accumulated understanding, incremental technological improvements, and periodic bursts of progress, investigators have steadily expanded the boundaries of implant dentistry. Over time, this evolution has considerably enhanced both clinical and patient-oriented treatment outcomes. Advancements in this field have included the appearance of nonsubmerged surgical protocols [36], the use of implants in partially edentulous patients under various conditions [37], the introduction of early/immediate loading [38], and the installation of implants into fresh extraction sockets [39]. Even so, multiple authors have urged caution when considering immediate implant surgery, particularly at esthetically demanding sites. In a systematic review, Niklaus Lang and colleagues reported an overall immediate implant survival rate of 98% but concluded that existing studies did not adequately characterize esthetic results, noting that post-extraction bone loss is an inevitable biological process affecting the treatment outcome [40]. Various authors have cited advanced midfacial recession (> one millimeter) as a concerning outcome following immediate implant surgery, with the potential to yield an unacceptable esthetic result [41-43].
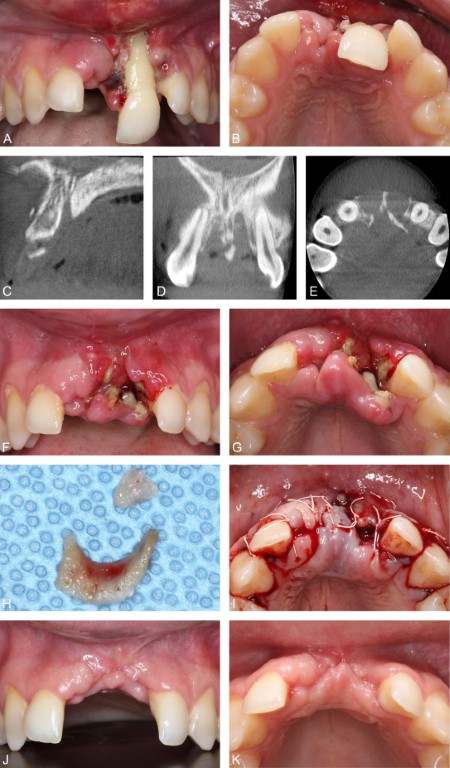
Figure 7: Case 3. Hockey injury. A and B. Initial presentation, facial and palatal views, respectively. C. Cone-beam computed tomography (CBCT) volume, midsagittal slice. Fractures of the facial, palatal, and interdental bone were present. Field of view 40 x 40 x 40 mm, isometric voxel size 0.08 mm, 88 kV, 7.9 mA, exposure time 30.8 s, arc of rotation 360 degrees. D. CBCT volume, coronal slice. E. CBCT volume, axial slice. The facial alveolar bone in the central incisor areas was virtually absent. Significant fractures in the palatal alveolar walls were also present. F and G. Clinical appearance five days following the injury (48 hours following extraction of the maxillary left central incisor and completion of medical and oral surgery consults), facial and palatal views, respectively. H. Sequestra removed from the left central incisor area. The larger segment measured ≈ 9 x 13 x 2 mm. I. Approximation of soft tissue following removal of the mobile bone segments. J and K. Clinical appearance seven weeks following the injury, facial and occlusal views, respectively.

Figure 8: Case 3. Temporary removable dental prosthesis at postoperative month two. A. Facial view. B. Smile.
Intuitively, post-traumatic immediate implant surgery—with or without immediate provisionalization—may heighten the probability of an unfavorable treatment outcome beyond the risks encountered at a site demonstrating pristine periodontal tissues. Nevertheless, IIPP offers clinical and patient-oriented advantages that are especially attractive in the management of acute oral trauma. IIPP may simplify treatment, reduce clinic visits and overall treatment time, offer favorable esthetics in the immediate postoperative period, and facilitate site development [44,45]. In addition, clinicians have for the most part overcome the risk of advanced midfacial recession through case selection and refinement of surgical techniques. Dennis Tarnow and other leading clinicians in implantology have identified factors associated with recession at immediate implant sites and offered clinical protocols to reliably develop harmonious peri-implant mucosal contours [45]. Factors that may protect against untoward peri-implant mucosal contours include proper orofacial implant position (i.e. avoiding an excessively facial position), presence of an intact facial cortex after tooth extraction, thick periodontal phenotype, flapless surgery, platform switching, use of a custom healing abutment or provisional restoration, and placement of a bone biomaterial in the peri-implant gap defect [43-48]. The volume of the graft may represent an important procedure-related influence. In a retrospective analysis, the horizontal distance between the facial cortex and the platform at implant installation was the main predictor of the vertical bone level after ≈ ten years [47]. Assuming appropriate case selection, IIPP may be a useful strategy for mitigating some negative psychosocial aspects of oral trauma and optimizing osseous and mucosal contours at the site. Conversely, post-traumatic IIPP in the presence of unfavorable site characteristics could place the patient at risk for an esthetic disaster.
The condition of the labial alveolar plate is one factor to consider in identifying candidates for post-traumatic IIPP. Consistent with the observed progress in various aspects of dental implantology since the late 1960s, Dr. Tarnow and colleagues have begun to investigate the predictability of immediate implant surgery at sites exhibiting labial alveolar deficiency—a prospect once considered heretical [48]. Ten patients with facial alveolar dehiscence defects at maxillary anterior sites received immediate implants and custom healing abutments, with serial cone-beam computed tomography scans acquired pre-extraction, at implant insertion, and six to nine months postoperatively [48]. At the follow-up assessment, all sites demonstrated labial peri-implant bone thickness of at least two millimeters [48]. In Case 2, IIPP was employed despite the obvious presence of an alveolar fracture. The patient exhibited a thick periodontal phenotype and favorable palatal/apical bone for implant stability. In addition, the planned platform position allowed placement of a relatively large FDBA volume in the peri-implant gap defect. To maintain optimal osseous and mucosal architecture, an eight-week healing period was permitted, then IIPP rather than ARP was performed. This approach allowed clinical assessment of the labial cortical plate prior to implant installation.
Many patients experiencing oral trauma are poor candidates for immediate implant surgery, Case 3 offering a clear example. Sites demonstrating severe alveolar destruction may require multiple site development procedures in advance of implant surgery, often leading to esthetic compromises. In some cases, a non-implant rehabilitation may produce superior outcomes. On the opposite end of the spectrum, some individuals suffering trauma to the anterior maxilla, such as the patient shown in Case 1, clearly benefit from IIPP and present low risk for an unfavorable result. Assessing risk in borderline cases represents a major challenge for implant surgeons, yet substantial benefits appear attainable when IIPP is a viable option. Proceeding cautiously with post-traumatic IIPP in the anterior maxilla when site- and procedure-related factors are favorable appears a reasonable approach. In addition, permitting a healing period following trauma may increase tissue stability at the site and offer time for further monitoring before finalizing the plan.
Limitations of this report are noteworthy. Due to the high mobility of the patient population, long-term follow-up was possible in only one of the presented cases, and in that case, follow-up was limited to 12 months. In addition, the patients in this report received treatment in an academic setting, thus limiting the generalizability of our findings. However, given the dearth of evidence guiding treatment decisions in this area, case reports demonstrating actions taken following oral trauma remain valuable for clinicians managing similar injuries. When appropriate, immediate implant surgery in the post-traumatic rehabilitation of the anterior maxilla may enhance clinical and patient-oriented treatment outcomes and mitigate some negative biopsychosocial consequences of trauma. Controlled clinical research is necessary to validate this assumption and clarify appropriate case selection.
Conclusions
Oral trauma involving the anterior maxilla commonly produces a set of negative biopsychosocial consequences, and in many instances, IIPP may mitigate several adverse effects of the traumatic episode. Although universal rules governing dental implant treatment planning in the post-traumatic rehabilitation of the anterior maxilla do not exist, preference toward immediate implant therapy should prevail when site characteristics are favorable. Limited evidence documenting positive outcomes achieved at maxillary anterior immediate implant sites with labial alveolar defects may imply that similar outcomes are attainable at sites exhibiting modest trauma-related alveolar damage, consistent with the outcomes reported herein. Clinical decisions in this context should encompass an individualized risk-benefit analysis and an informed decision-making process involving both the patient and the surgeon. Trauma adds additional uncertainty to the technically demanding task of implant placement in the esthetic zone. When in doubt, a conservative approach appears prudent.
Disclosure statement
The views expressed in this manuscript are those of the authors and do not necessarily reflect the official policy of the United States Government, the Department of Defense, the Defense Health Agency, the Department of the Army, the United States Army Medical Department, or Uniformed Services University.
Author contribution statement: All authors have contributed substantially to conceptualization of the article, writing the original draft, critical review, and editing. All authors have approved the final version of the manuscript.
Funding: The authors report no extramural funding.
Conflict of interest statement: The authors report no financial, economic, or professional interests that may have influenced the design, execution, or presentation of this work.
References
- Andersson L. Trauma in a global health perspective. Dent Traumatol. 2008;24(3):267. [PubMed.]
- Arhakis A., Athanasiadou E., Vlachou C. Social and psychological aspects of dental trauma., behavior management of young patients who have suffered dental trauma. Open Dent J. 2017;11:41–47. [PubMed.]
- Giannetti L., Murri A., Vecci F., Gatto R. Dental avulsion:therapeutic protocols and oral health–related quality of life. Eur J Paediatr Dent. 2007;8(2):69–75. [PubMed.]
- Teófilo LT., Leles CR. Patients' self–perceived impacts and prosthodontic needs at the time and after tooth loss. Braz Dent J. 2007;18(2):91–96. [PubMed.]
- Al–Omiri MK., Karasneh JA., Lynch E., Lamey PJ., Clifford TJ. Impacts of missing upper anterior teeth on daily living. Int Dent J. 2009;59(3):127–132. [PubMed.]
- Lee JY., Divaris K. Hidden consequences of dental trauma:the social and psychological effects. Pediatr Dent. 2009;31(2):96–101. [PubMed.]
- Brennan DS., Spencer AJ., Roberts–Thomson KF. Tooth loss., chewing ability and quality of life. Qual Life Res. 2008;17(2):227–235. [PubMed.]
- Bortoluzzi MC., Traebert J., Lasta R., Da Rosa TN., Capella DL., et al. Tooth loss., chewing ability and quality of life. Contemp Clin Dent. 2012;3(4):393–397. [Ref.]
- Okoje VN., Dosumu OO., Alonge TO., Onyeaso C. Tooth loss:are the patients prepared? Nigerian J Clin Pract. 2012;15(2):172–175. [PubMed.]
- Davis DM., Fiske J., Scott B., Radford DR. The emotional effects of tooth loss:A preliminary quantitative study. Br Dent J. 2000;188(9):503–506. [PubMed.]
- Kramer PF., Zembruski C., Ferreira SH., Feldens CA. Traumatic dental injuries in Brazilian preschool children. Dent Traumatol. 2003;19(6):299–303. [PubMed.]
- Forsberg CM., Tedestam G. Traumatic injuries to teeth in Swedish children living in an urban area. Swed Dent J. 1990;14(3):115–122. [PubMed.]
- Gerritsen AE., Allen PF., Witter DJ., Bronkhorst EM., Creugers NH. Tooth loss and oral health–related quality of life:a systematic review and meta–analysis. Health Qual Life Outcomes. 2010; 8:126. [PubMed.]
- Rao LN., Shetty A., Hedge MN. Psychological effects of trauma to anterior teeth. Indian J Public Health Res Dev. 2020;11:125. [Ref.]
- Litt MD. A model of pain and anxiety associated with acute stressors:Distress in dental procedures. Behav Res Ther. 1996;34(5–6):459–476. [PubMed.]
- Skaret E., Raadal M., Berg E., Kvale G. Dental anxiety and dental avoidance among 12– to 18–year–olds in Norway. Eur J Oral Sci. 1999;107(6):422–428. [PubMed.]
- Wong FS., Kolokotsa K. The cost of treating children and adolescents with injuries to their permanent incisors at a dental hospital in the United Kingdom. Dent Traumatol. 2004;20(6):327–333. [PubMed.]
- Van der Geld P., Oosterveld P., Van Heck G., Kuijpers–Jagtman AM. Smile attractiveness:self–perception and influence on personality. Angle Orthod. 2007;77(5):759–765. [PubMed.]
- Klages U., Bruckner A., Zentner A. Dental aesthetics., self–awareness., and oral health–related quality of life in young adults. Eur J Orthodont. 2004;26(5):507–514. [PubMed.]
- Dion K., Berscheid E., Walster E. What is beautiful is good. J Pers Soc Psychol. 1972;24(3):285–290. [Ref.]
- Bull R., Rumsey N. The Social Psychology of Facial Appearance. New York:Springer. 2012. [Ref.]
- Flanary C. The psychology of appearance and psychological impact of surgical alteration of the face. In:Bell WH., ed. Modern Practice in Orthognathic and Reconstructive Surgery. Philadelphia:Saunders. 1992;3–21. [Ref.]
- Gupta T., Sadana G., Rai HK. Effect of esthetic defects in anterior teeth on the emotional and social well–being of children:a survey. Int J Clin Pediatr Dent. 2019;12(3):229–232. [Ref.]
- Tsakos G., Marcenes W., Sheiham A. The relationship between clinical dental status and oral impacts in an elderly population. Oral Health Prev Dent. 2004;2(3):211–220. [PubMed.]
- American Association of Endodontists. The Recommended Guidelines of the American Association of Endodontists for The Treatment of Traumatic Dental Injuries. 2023. [Ref.]
- Levin L., Day PF., Hicks L., O'Connell A., Fouad AF., et al. International Association of Dental Traumatology guidelines for the management of traumatic dental injuries:General introduction. Dental Traumatol. 2020;36(4):309–313. [PubMed.]
- Bourguignon C., Cohenca N., Lauridsen E., Flores MT., O'Connell AC., et al. International Association of Dental Traumatology guidelines for the management of traumatic dental injuries:1. Fractures and luxations. Dental Traumatol. 2020;36(4):314–330. [PubMed.]
- Fouad AF., Abbott PV., Tsilingaridis G., Cohenca N., Lauridsen E., et al. International Association of Dental Traumatology guidelines for the management of traumatic dental injuries:2. Avulsion of permanent teeth. Dental Traumatol. 2020;36(4):331–342. [PubMed.]
- Nørgaard Petersen F., Jensen SS., Dahl M. Implant treatment after traumatic tooth loss:A systematic review. Dental Traumatol. 2022;38(2):105–116. [PubMed.]
- Schwartz‐Arad D., Levin L. Post‐traumatic use of dental implants to rehabilitate anterior maxillary teeth. Dent Traumatol. 2004;20(6):344–347. [PubMed.]
- Schwartz–Arad D., Levin L., Ashkenazi M. Treatment options of untreatable traumatized anterior maxillary teeth for future use of dental implantation. Implant Dent. 2004;13(1):120–128. [PubMed.]
- Nagendrababu V., Chong BS., McCabe P., Shah PK., Priya E., et al. PRICE 2020 guidelines for reporting case reports in Endodontics:a consensus‐based development. Int Endod J. 2020;53(5):619–626. [PubMed.]
- Branemark PI., Breine U., Adell R., Hansson BO., Lindström J., et al. Intra–osseous anchorage of dental prostheses:I. Experimental studies. Scand J Plasl Reconstr Surg. 1969;3(2):81–100. [PubMed.]
- Adell R., Hansson BO., Branemark PI., Breine U. Intra–osseous anchorage of dental prostheses. Scand J Plasl Reconstr Surg. 1970;4(1):19–34. [PubMed.]
- Adell R., Lekholm U., Rockler BR., Branemark PI. A 15–year study of osseointegrated implants in the treatment of the edentulous jaw. Int J Oral Surg. 1981;10(6):387–416. [PubMed.]
- Buser D., Mericske‐stern R., Pierre Bernard JP., et al. Long‐term evaluation of non‐submerged ITI implants. Part 1:8‐year life table analysis of a prospective multi‐center study with 2359 implants. Clin Oral Implants Res. 1997;8(3):161–172. [PubMed.]
- Buser D., Von Arx T. Surgical procedures in partially edentulous patients with ITI implants note. Clin Oral Implants Res. 2000;11(Suppl 1):83–100. [PubMed.]
- Degidi M., Piatelli A. Immediate functional and non–functional loading of dental implants:a 2– to 60–month follow–up study of 646 titanium implants. J Periodontol. 2003;74(2):225–241. [PubMed.]
- Schulte W., Heimke G. The Tübingen immediate implant. Quintessenz. 1976;27(6):17–23. [PubMed.]
- Lang NP., Pun L., Lau KY., Li KY., Wong MC. A systematic review on survival and success rates of implants placed immediately into fresh extraction sockets after at least 1 year. Clin Oral Implants Res. 2012;23(Suppl 5):39–66. [PubMed.]
- Cosyn J., Hooghe N., De Bruyn H. A systematic review on the frequency of advanced recession following single immediate implant treatment. J Clin Periodontol. 2012;39(6):582–589. [PubMed.]
- Cosyn J., Eghbali A., De Bruyn H., Collys K., Cleymaet R., et al Immediate single–tooth implants in the anterior maxilla:3–year results of a case series on hard and soft tissue response and aesthetics. J Clin Periodontol. 2011;38(8):746–753. [PubMed.]
- Chen ST., Darby IB., Reynolds EC. A prospective clinical study of non‐submerged immediate implants:clinical outcomes and esthetic results. Clin Oral Implants Res. 2007;18(5):552–562. [PubMed.]
- Cheng AW., Berridge JP., McGary RT., Erley KJ., Johnson TM. The extraction socket management continuum:a hierarchical approach to dental implant site development. Clin Adv Periodontics. 2019;9(2):91–104. [PubMed.]
- Chu SJ., Salama MA., Salama H., et al. The dual–zone therapeutic concept of managing immediate implant placement and provisional restoration in anterior extraction sockets. Compend Contin Educ Dent. 2012;33(7):524–532. [PubMed.]
- El–Chaar ES. Immediate placement and provisionalization of implant–supported., single–tooth restorations:a retrospective study. Int J Periodontics Restorative Dent. 2011;31(4):409–419. [PubMed.]
- Kuchler U., Chappuis V., Gruber R., Lang NP., Salvi GE. Immediate implant placement with simultaneous guided bone regeneration in the esthetic zone:10‐year clinical and radiographic outcomes. Clin Oral Implants Res. 2016;27(2):253–257. [PubMed.]
- Sarnachiaro GO., Chu SJ., Sarnachiaro E., Gotta SL., Tarnow DP. Immediate implant placement into extraction sockets with labial plate dehiscence defects:a clinical case series. Clin Implant Dent Relat Res. 2016;18(4):821–829. [PubMed.]