>Corresponding Author : Bhargav Ram
>Article Type : Original Research Article
>Volume : 2 | Issue : 1
>Received Date : 13 June, 2022
>Accepted Date : 24 June, 2022
>Published Date : 27 June, 2022
>DOI : https://doi.org/10.54289/JDOE2200104
>Citation : Ram B, Mahabaleshwara CH, Rachana PB, Ravindra I, Jayaram S, et al. (2022) Comparison Between Preoperative Inflammation Based Scores and TNM Staging in Patients with Oral Cancer. J Dent Oral Epidemiol 2(1): doi https://doi.org/JDOE2200104
>Copyright : © 2022 Ram B, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Original Research Article | Open Access | Full Text
1Post graduate, Department of Oral and Maxillofacial Surgery, KVGDCH, Sullia, DK, Karnataka, India
2Professor, Department of Oral and Maxillofacial Surgery, KVGDCH, Sullia, DK, Karnataka, India
3Reader, Department of Oral and Maxillofacial Surgery, KVGDCH, Sullia, DK, Karnataka, India
4Dentist, Ongole, Andhra Pradesh, India
*Corresponding author: Bhargav Ram, Post graduate, Department of Oral and Maxillofacial Surgery, KVGDCH, Sullia, DK, Karnataka, India
Abstract
Background: India, one of the countries with the highest incidence of oral cancer, accounting for 30% of all new oral cancer cases in the world. Therefore, strong diagnostic markers are critical for the diagnosis and survival of patients suffering from oral cancer. Based on this relationship between inflammation and cancer progression, several inflammation-based scores have been demonstrated to have diagnostic and prognostic value in many types of malignant solid tumours.
Objective: To compare the correlation between systemic inflammation based prognostic scores and tumour node metastasis (TNM) stage in patients undergoing oral cancer treatment.
Methods: The inflammation-based scores were calculated for 120 patients with oral squamous cell carcinoma divided into four groups based on TNM staging. Neutrophil lymphocyte ratio (NLR), platelet lymphocyte ratio (PLR), tumour size, nodes involved were analysed. Statistics were performed to compare the diagnostic value of the selected scores and TNM stage.
Results: This current study compares 30 patients in each stage of TNM stages 1,2,3 and 4. The mean tumour size is 1.8 x 1.41, 3.23x2.28, 2.85x2.43 and 3.78x 3.06 in stage 1,2,3 and 4 respectively. The largest lymph node measurable was 1.33x1.36 in stage 3 and 1.84x 1.38 in stage 4. The number of lymph nodes involved in stage 3 are 1.1 and 2.82 in stage 4. The mean NLR in stage 1,2,3 and 4 were 2.68, 2.72, 3.17 and 3.68 respectively. The mean PLR in stage 1, 2,3 and 4 were 106.4, 117.8, 108.2 and 182.2 respectively.
Conclusion: The present study indicates that elevated NLR and PLR values are associated with advanced stages of TNM staging for Oral squamous cell carcinoma.
Keywords: Oral Cancer, TNM staging, Inflammation-Based Score, Diagnostic Value
Abbreviations: TNM: Tumour Node Metastasis, NLR: Neutrophil Lymphocyte Ratio, PLR: Platelet Lymphocyte Ratio, OSCC: Oral Squamous Cell Carcinoma
Introduction
Oral squamous cell carcinoma (OSCC) is a commonly diagnosed cancer all throughout globe, with 377,713 occurrences reported in 2020. In 2018, Globocan discovered that oral malignancies accounted for 2% of all cancers and 1.9 percent of cancer-related deaths [1]. Oral cancer is a massive issue in the Indian subcontinent where it is one of the country's top three cancers. In India, age-adjusted rates of mouth cancer are high, at 20 per 100,000 people and oral cancer accounts for more than 10% of all cancers. The combined influence of ageing population, as well as regional differences in the prevalence of illness-specific risk factors, can be linked to the variance in disease incidence and pattern [2].
Clinical TNM staging is now the sole valid predictive factor utilised in treatment-naive patients around the world. Despite the fact that pathological TNM staging provides more precise information, it is only available after therapy has begun and after patient has had surgical treatment [3].
Because of their susceptibility to phenotypic changes induced by the tumour microenvironment as well as their ability to influence the behaviour of other cancer-associated immune cells, neutrophils are widely acknowledged to play critical roles in all stages of tumorigenesis from initiation to primary tumour growth and metastasis. The inflammatory response has been reported to have a significant role in tumour growth and may impact cancer patient survival outcomes. High neutrophil, platelet, macrophage counts, low lymphocyte counts and high NLR, PLR have all been linked to a poor prognosis of cancer.
NLR and PLR are biomarkers that may be used to monitor diabetes, malignancies, obesity, metabolic syndromes, cardiovascular disease, renal failure, any chronic nutritional states, cerebrovascular disease, Alzheimer's, COPD and even mental diseases like delirium, among others. This measurement may also be used to track pharmacological therapy and to determine the prognosis of patients receiving various therapies for various cancers. As a result the neutrophil–to–lymphocyte ratio (NLR) which integrates the detrimental effects of neutrophilia and lymphopenia has been proposed as a simple and low-cost diagnostic biomarker in a variety of cancers [4].
Oral cancer is a serious concern in India according to public health agencies, private hospitals, and academic medical centres. Efforts to expand the body of literature on illness aetiology and regional distribution of risk factors have started to gain traction. Oral cancer will continue to be a serious public health issue but early identification and prevention measures will help to alleviate the burden. The aim of the current study is to evaluate, compare and find any significant co-relation between the diagnostic value of inflammation-based prognostic scores and Tumor node metastasis (TNM) stage by AJCC 8th edition in patients undergoing oral cancer treatment.
Materials and Methods
This retrospective study was conducted from December 2019 to June 2021. Case records and blood investigations of the patients who reported with diagnosis of oral squamous cell carcinoma data were collected regarding the age, gender, site of lesion, tumour size, number of nodes involved, largest node size, total leukocyte count, differential count and platelet count.
The patients aged between 18-70 years with clinically and histopathologically diagnosed oral squamous cell carcinoma are included and patients with past history of any major uncontrolled systemic illness such as liver disease, tuberculosis, diabetes, hypertension, history of trauma less than two months back, with acute illness, infection or pregnancy, patients undergoing radiotherapy/chemotherapy for treatment of cancer, patients with history of malignancy other than oral squamous cell carcinoma, patients with recurrent oral squamous cell carcinoma and terminally ill patients were excluded from the study groups. The patient were divided into four groups (stage 1,2,3 and 4) containing 30 subjects each based on four stages of AJCC 8th edition clinical TNM staging respectively. These groups were evaluated for the above parameters and compared between them. The institutional ethical committee approved the study in its presented format.
The data was checked for normality using Normality tests (Kolmogorov Smirnov and Shapiro Wilk test). The data follows “Normal distribution” (p value > 0.05) for age, neutrophil count, and platelets count. Hence parametric tests of significance were applied for comparisons between stages. The data shows “Non-normal distribution” (p<0.05) for lymphocyte count, NLR and PLR. The NLR and PLR were compared between the stages using non parametric tests of significance (Kaushal Willis ANOVA and post hoc Mann Witney test).
Results
A total of 120 individuals reported with oral squamous cell carcinoma from December 2019 to June 2021. The mean age was 50+11 years, and 93 (77.5%) patients were males and 27 (22.5%) were females. (Table 1)
This current study compares 30 patients in each stage of TNM stages 1, 2, 3 and 4. The mean age and gender distribution is similar in all the four groups and there is no significant difference between all the four groups. The commonest site involved in stage 1 is tongue followed by retro molar trigone and buccal mucosa. In stage 2, 3 and 4 the commonest involved sites are buccal mucosa followed by tongue and retro molar trigone area. (Table 1) The mean tumour size is 1.8 x 1.41, 3.23x2.28, 2.85x2.43 and 3.78x 3.06 in stage 1,2,3 and 4 respectively. There is significant tumour size difference in stage 1 and 4 but no significant difference between stage 1, 2 and 3. The largest lymph node measurable was 1.33x1.36 in stage 3 and 1.84x 1.38 in stage 4. The number of lymph nodes involved in stage 3 are 1.1 and 2.82 in stage 4. Both mean lymph node number and mean lymph node size were statistically significant between stage 3 and 4. (Table 2)
The mean NLR in stage 1,2,3 and 4 were 2.68, 2.72, 3.17 and 3.68 respectively. The lowest being for stage 1 and highest being stage 4. There is no significant difference between stage 1 and 2 but significant difference was found between stage 1,3 and 4. The mean PLR in stage 1, 2,3 and 4 were 106.4, 117.8, 108.2 and 182.2 respectively. The lowest being stage 1 and highest being stage 4. There was no significant difference between stage 1,2 and 3 but there was significant difference between these and stage 4. (Table 2)
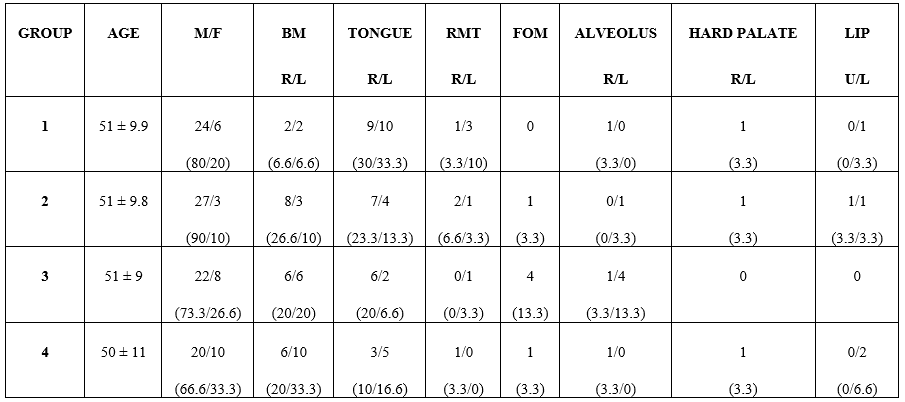
Table 1: Various parameters regarding oral cancer patients
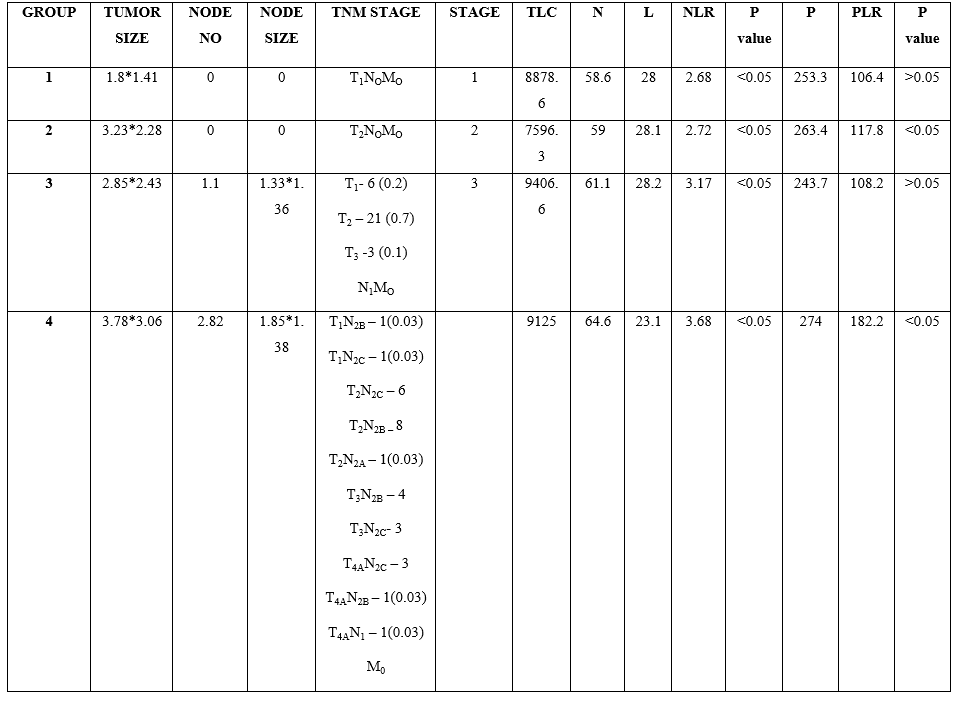
Table 2: Various parameters in different stages
Discussion
Oral cancer is a major concern in maxillofacial tertiary care institutions, with high death rates and a considerable impact on quality of life and morbidity. Previously, this was mostly a disease of the elderly with well-known epidemiological risk factors however this looks to be changing. The most acknowledged risk factor is the use of tobacco in both smokeable and chewable forms on a regular basis [5].
Furthermore, increased NLR has been linked to a poor prognosis in people with oesophageal, colorectal, oral, pancreatic, prostate, hepatic, bile duct, breast, gastric, cutaneous melanocytic, thyroid medullary and lung cancer according to several studies. However, it's important to keep in mind that NLR can be elevated in a number of benign conditions [6,7]. Patients with a high platelet count are more likely to develop cancer, as well as some malignancies that have a stronger link to thrombocytosis. Previous research has found that platelet count has a predictive relevance in a range of solid tumours (oral, renal-cell, hepatocellular, lung, colorectal, gastric and gynaecological). Lymphocytes, the second component of NLR and PLR have long been recognised for their critical involvement in cancer growth and progression. Lymphocytes, the primary effectors of the anti-tumour immune response work at the tumour site as well as in the peripheral compartment. Extensive research over the last several decades has yielded crucial knowledge on the mechanisms that back and interfere with the systemic anti- immunotherapy. High NLR and PLR has been linked to worse survival in a number of solid tumours (oral, tumour immune response leading to one of the most significant discoveries in cancer history - the discovery of hepatocellular, ovarian, cervix, colorectal, bile duct, breast, lung, renal cell, gastric, prostate and oesophageal) [8,9].
The main purpose of the TNM classification system is to provide an anatomically based classification that appropriately portrays cancer prognosis. For therapy selection, diagnosis, prognosis, research design, cancer control approaches and precision in cancer staging is crucial. Clinical care, clinical trial eligibility, stratification, research, health services, cancer registry operations, cancer control and policy development all use the TNM classification. It has been widely utilised by a varied range of users since its introduction, including doctors, researchers and cancer registrars from several fields [10].
Our retrospective study's goal was to compare systemic inflammation based diagnostic scores to TNM stage in order to uncover therapeutically effective diagnostic markers for customised therapy in patients with oral cancer. There are very few studies available in literature which compares systemic inflammatory indicators and TNM staging in head and neck cancer.
A similar study was conducted by Chen Th et al.in 2017 among 1383 patients with colorectal cancer. The authors compared systemic immune inflammation index which was found by dividing the product of platelets and neutrophils by lymphocytes, NLR and PLR for predicting prognosis of colorectal cancer in according to TNM staging and found out that the NLR in stage 4 is greater than stage 3, 2 and stage 1. There was no significant difference between stage 1 and stage 2. PLR can identify the survival difference between stage 2,3 and 4 but has very little value in stage 1. The results were similar to our current study except the PLR values are not significant between stage1, 2 and 3 [11].
A study conducted by Caruntu et al, in 2021 in a study group of 111 oral squamous cell carcinoma. The authors divided the patients into two groups based on PLR value of 120. They found out that the group with PLR less than or equal to 120 has highest number of disease survivors and the group with PLR more than or equal to 120 has highest diseased individuals and found no statistically difference based on TNM staging although there was steep increase of PLR between stage 4 and stage 1. This study findings are in line with our study [12].
Ferroni et al Conducted a retrospective study in 475 women with breast cancer in 2018 to find prognosis and significance of NLR in framework of 8th edition TNM staging for breast cancer. According to them the optimal NLR cut off value was at 2:00 and 74% of patients with NLR more than 2 to developed distant metastasise. The elevated NLR value was associated with poor prognosis and poor overall survival rate. NLR cut off value can be steadily determined from stage 1 to stage 4. The NLR values are highest for stage 4 and lowest for stage 1 and results of this study were in conclusive to the current study [4].
Pan et al Conducted a study in Chinese population of 207 gastric cancer patients who underwent surgery. The authors found out PLR more than or equal to 150 and NLR more than or equal to 5 are independent markers of poor prognosis and advanced stage of disease. They also conclude that high preoperative NLR and PLR rates are found in patients with stage 4 although it is not significant in stage 1, 2 and 3 of TNM staging. The above findings are partially coinciding with our current study [13].
In a study conducted by Yang et al. in 2017 to find out clinical base line and prognostic difference of PLR and TNM staging in right and left sided colon cancer. The study sample included 1846 patients in which 744 were with right side colon cancer and 1102 with left side colon cancer. The authors concluded that the height PLR values are significantly associated with poor overall survival and elevated with TNM staging. They also concluded that PLR is a an inexpensive and readily available inflammatory marker which is significant in assessing overall survival and more commonly elevated in advanced TNM staging. This study had similar results as our study [14].
This current study has few drawbacks, including a small sample size, a single-center study, and a retrospective analysis. To corroborate the findings, larger-scale, multicenter and prospective research are required.
Clinical Relevance
Scientific rationale for study: Increased pre operative inflammation scores have been identified in a vast variety of cancer. The aim of this study is to evaluate the preoperative.
Principal findings: High neutrophil lymphocyte ratio and platelet lymphocyte counts are associated with advanced inflammatory scores and their correlation with TNM staging.
stages of oral cancer
Practical implications: The pre operative inflammatory score can be used along with TNM staging for assessing the stage and treatment outcomes.
Conclusion
The current study found that NLR and PLR are independent predictors of overall advanced tumour stage. Furthermore, NLR and PLR values broadly correlate with TNM staging for oral cavity SCC. The current study suggests that pre-operative NLR, PLR levels and TNM stage may be utilised in combination before surgery to offer more accurate survival prediction and more reliable treatment choice information for patients with oral cancer.
Conflict Of Interest: None.
Author Contribution: All the authors participated in concept and study design, participated in collection of data and wrote the manuscript. All authors read and approved manuscript.
Ethical Approval: Accepted.
Data Availability Statement: Data sharing not applicable—no new data generated, or the article describes entirely theoretical research.
References
- Bray F., Ferlay J., Soerjomataram I., Siegel RL., Torre LA., et al. Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. 2018; 68(6): 394-424. [PubMed.]
- Coelho KR. Challenges of the oral cancer burden in India. J Cancer Epidemiol. 2012. [Ref.]
- Kreppel M., Nazarli P., Grandoch A., Safi AF., Zirk M., et al. Clinical and histopathological staging in oral squamous cell carcinoma - Comparison of the prognostic significance. Oral Oncol. 2016; 60: 68-73. [PubMed.]
- Ferroni P., Riondino S., Formica V., Cereda V., Tosetto L., et al. Venous thromboembolism risk prediction in ambulatory cancer patients: clinical significance of neutrophil/lymphocyte ratio and platelet/lymphocyte ratio. Int J Cancer. 2015; 136(5): 1234-1240. [PubMed.]
- Rooban T., Joshua E., Rao UK., Ranganathan K. Prevalence and correlates of tobacco use among urban adult men in India: A comparison of slum dwellers vs. non-slum dwellers. Indian J Dental Res. 2012; 23: 31-38. [Ref.]
- Turkmen K., Erdur FM., Ozcicek F., Ozcicek A., Akbas EM., et al. Platelet-to-lymphocyte ratio better predicts inflammation than neutrophil-to-lymphocyte ratio in end-stage renal disease patients. Hemodialysis Int. 2013; 17: 391-396. [PubMed.]
- Shah N., Parikh V., Patel N., Patel N., Badheka A., et al. Neutrophil lymphocyte ratio significantly improves the Framingham risk score in prediction of coronary heart disease mortality: Insights from the National Health and Nutrition Examination Survey-III. Int. J. Cardiol. 2014; 171: 390-397. [PubMed.]
- Nash GF. Turner LF., Scully MF., Kakkar AK. Platelets and cancer. Lancet Oncol. 2002; 3: 425-430. [PubMed.]
- Bailey SER., Ukoumunne OC., Shephard E., Hamilton W. How useful is thrombocytosis in predicting an underlying cancer in primary care? a systematic review. Fam. Pract. 2017; 34: 4-10. [PubMed.]
- Huang SH., O’Sullivan B. Overview of the 8th Edition TNM Classification for Head and Neck Cancer. Curr. Treat. Options in Oncol. 2017; 18: 40. [PubMed.]
- Chen JH., Zhai ET., Yuan YJ., Wu KM., Xu JB., et al. Systemic immune-inflammation index for predicting prognosis of colorectal cancer. World J Gastroenterol. 2017; 23(34): 6261. [PubMed.]
- Caruntu A., Moraru L., Lupu M., Taubner L., Caruntu C., et al. The hidden treasures of preoperative blood assessment in oral cancer: a potential source of biomarkers. Cancers. 2021; 13(17): 4475. [PubMed.]
- Pan QX., Su ZJ., Zhang JH., Wang CR., Ke SY. A comparison of the prognostic value of preoperative inflammation-based scores and TNM stage in patients with gastric cancer. Onco Targets and therapy. 2015; 8: 1375. [Ref.]
- Yang L., He W., Kong P., Jiang C., Yang Q., et al. Clinical baseline and prognostic difference of platelet lymphocyte ratio PLR; in right-sided and let-sided colon cancers. BMC cancer. 2017; 17(1): 1-1. [Ref.]