>Corresponding Author : Muntadher Abdulkareem Abdullah
>Article Type : Case Report
>Volume : 3 | Issue : 2
>Received Date : 04 Feb, 2023
>Accepted Date : 24 Feb, 2023
>Published Date : 01 Mar, 2023
>DOI : https://doi.org/10.54289/JCRMH2300109
>Citation : Abdullah MA. (2023) Prolonged Cholestasis in Patient with Acute HAV Infection (Unusual Presentation) (Role of Steroids). J Case Rep Med Hist 3(2): doi https://doi.org/10.54289/JCRMH2300109
>Copyright : © 2023 Abdullah MA. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Case Report | Open Access | Full Text
Lecturer at Basrah college of Medicine, Basrah Gastroenterology and Hepatology hospital
*Corresponding author: Muntadher Abdulkareem Abdullah, Lecturer at Basrah college of Medicine, Basrah Gastroenterology and Hepatology Hospital
Abstract
Background: Hepatitis A virus (HAV) is a virus which infects yearly more than 1.5 million persons worldwide and is usually spread through contaminated food and water. Most HAV infection in children under the six years of age are asymptomatic and they develop lifelong immunity. However, HAV infection in older children and adults often symptomatic with development of jaundice, nausea, vomiting, poor appetite, fever, fatigue, abdominal pain, etc. most of those infected patients usually fully recovering from HAV infection naturally within 2 months, it has not been a cause for major concern of public health).
With more and more patients suffering from hepatitis A, there is also increase in the number of patients suffering from unusual presentation of HAV infection also. Most hepatitis A patients tend to recover from the illness natural without any complications; however, there are occasions of serious complications among adult hepatitis A patients such as extrahepatic manifestation, acute renal failure, cholestatic hepatitis, relapsing hepatitis, prolonged course and even fulminant hepatic failure. Cholestatic hepatitis accounts for between 0.8 - 5.2% of hepatitis. Together with increasingly more cases of hepatitis A being reported, the number of patients who have cholestatic hepatitis arising from hepatitis A also has increased.
The current treatment for hepatitis A is usually symptomatic treated by sufficient nutrition, vitamin supply and sufficient rest. There are also no special treatments for cholestatic hepatitis, with conservative treatment being used. Ursodeoxycholic acid (UDCA) and cholestyramine and antihistamines are used to treat skin itching caused by cholestatic hepatitis; however, there are occasions where symptoms of cholestatic hepatitis are so severe and prolong that required the use of corticosteroids to shorten the duration of symptoms and reduce hospitalization.as to call for liver transplantation.
Aim: Is to show the effectiveness of corticosteroids in shorten the duration of severe symptoms and shorten hospitalization in patient with prolong severe cholestatic symptoms of acute hepatitis A virus infection.
Abbreviations: HAV: Hepatitis A Virus, UDCA: Ursodeoxycholic Acid, ABC: ATP-Binding-Cassette
Case Report
A 17-year-old male patient, immunocompetent, was referred to our hospital due to prolonged jaundice diagnosed as acute viral hepatitis A TWO months previously based on typical clinical symptoms of acute hepatitis support by serological investigation, at time of referral patient was complained of deep jaundice, severe itching associated with profound anorexia with significant wt. loss of about 16 kg over the last two months of starting the illness.
On physical examination:
Patient was conscious and oriented
Stable vital signs and afebrile
Deeply jaundice
Evidence of scratch marks over the legs, arms and abdomen, No organomegaly, No LAPS
The patient was admitted to the hospital
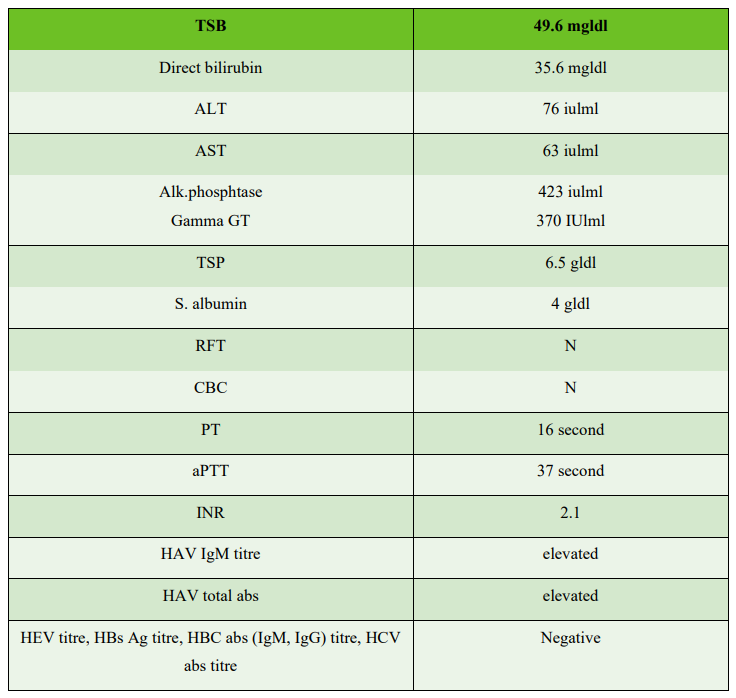
Investigation at time of admission:
Biliary obstruction had been excluded with the normal abdominal ultrasound and normal abdominal MRI, MRCP, Despite the two weeks of in hospital conservative treatment there was no satisfactory clinical and biochemical response So we decide to start oral steroid after excluding of current infections.
So, at the third week of the hospital admission prednisolone tablets at a dose of 30 mglday was started alongside with continuing the symptomatic and the supportive treatment.
After the first week of the oral steroid therapy, the pruritus significantly improved, the jaundice and the appetite profoundly improved, without significant steroid side effects.
On the 14th day of prednisolone administration, total and direct bilirubin decreased to 11.3 mg/dL and 6.1 mg/dL respectively with improvement of the patient symptoms, and he discharged home and scheduled for outpatient follow up.
After 4 weeks following the administration of prednisolone, prednisolone dose was tapered off by 10 mg at intervals of two weeks. On the 8th weeks, total bilirubin decreased to 1.1 mg/dL, no relapse of HAV infection.
Discussion
Prolonged cholestasis is one of atypical manifestations of hepatitis A infection. Appropriate diagnosis and treatment are needed because this manifestation will increase morbidity and medical cost.
Clinical presentations are more severe with increasing age, so adults are more frequently associated with prolonged jaundice compared to children. The genotype of the viral hepatitis A is also reported to affect the severity of the cholestasis [1].
Seven HAV genotypes (I–VII) have been identified [2], four of which (I, II, III, and VII) were recovered from humans with HAV infection, and three of which (IV–VI) were recovered only from a simian species that developed a hepatitis A–like illness during captivity [2,3,4].
Cholestasis happens because of some mechanism, including decreased bilirubin uptake, conjugation dysfunction, bilirubin excretion dysfunction and biliary obstruction. In hepatitis A, cholestasis happens because of inflammatory process. Endotoxin and pro inflammatory cytokines are released from liver and also as systemic response. TNF alfa and IL-1 inhibit mrp2 (multidrug-resistance associated protein 2), one of the proteins that has role in bilirubin excretion [5].
It is therefore conceivable that cholestasis associated with this inflammatory process can be improved by the administration of steroids. It is known that multidrug resistance-associated protein 2 (mrp2), a transporter protein which is involved in excretion of the bilirubin outside the hepatocytes during the steps of bilirubin metabolism, is inhibited by TNF-α and IL-1 [6].
Steroids inhibit the synthesis of TNF-α and IL-1, and thereby prevents impairment of the function of mrp2 in the canaliculi of endotoxemic rats [7]. Steroids induce the expression of mrp2 twice as much even in normal liver tissue and facilitates the metabolism of the bilirubin [8].
Physiologically, the normal flow of bile through the biliary tract this is maintained by a set of hepatocanalicular proteins transporting major biliary lipids from hepatocytes into the bile canaliculi [9], these ATP-binding-cassette (ABC) proteins, namely ABCB4, ABCB11 and ABCG5/8, transport phosphatidylcholine, bile salts and sterols respectively and subjected to genetic pleomorphism.
Several common and rare variants within these transporters have been identified as genetic risk factors for cholestasis [10].
In Summary
The risk of Prolonged cholestasis in the setting of acute hepatitis A infection can be increased due to:
• Increasing age of the patient
• Infection with HAV genotypes Ia and Ib
• Pleomorphism in the host bilirubin transporting protein genes
Persistent cholestasis can still be managed symptomatically, but this frequently lengthens hospital stay and causes higher medical expenses and social economic loss.
The decision to begin steroids was based on the often-debilitating symptoms associated prolonged cholestasis. Prednisone or corticosteroid generally resulted in symptomatic relief and rapid initial drop in serum bilirubin levels [11].
It was reported that cholestasis spontaneously resolves although corticosteroids may hasten the resolution, but it may predispose the patient to develop a relapse of the hepatitis.
Also need to search for hidden infections before starting steroids in patient with complicated HAV infection.
References
- Coppola N, Genovese D, Pisaturo M, Taffon S, Argentini C, et al. (2007) Acute hepatitis with severe cholestasis and prolonged clinical course due to hepatitis A virus Ia and Ib coinfection. Clin Infect Dis. 44: e73-77. [Ref.]
- Robertson BH, Jansen B, Khanna RW, et al. (1992) Genetic relatedness of hepatitis A virus strains recovered from different geographic regions. J Gen Virol. 73: 1365-1377. [PubMed.]
- Tsarev SA, Emerson SU, Balayan MS, Ticehurst J, Purcell RH. (1991) Simian hepatitis A virus (HAV) strain AGM-27: comparison of genome structure and growth in cell culture with other HAV strains. J Gen Virol. 72: 1677-1683. [PubMed.]
- de Paula VS, Baptista ML, Lampe E, Niel C, Gaspar AMC. (2002) Characterization of hepatitis A virus isolates from subgenotypes Ia and Ib in Rio de Janeiro, Brazil. J Med Virol. 66: 22-27. [PubMed.]
- Trauner M, Fickert P, Stauber RE. (1999) Inflammation-induced cholestasis. J Gastroenterol Hepatol. 14: 946-959. [PubMed.]
- Wolkoff AW. (2008) The Hyperbilirubinemias. In: Fauci AS, Braunwald E, Kasper DL, Hauser SL, Longo DL, Jameson HL, eds. Harrison’s principles of internal medicine. Mc Graw Hill. 2(17edition): 1927-1931. [Ref.]
- Roelofsen H, Schoemaker B, Bakker C, Ottenhoff R, Jansen PL, et al. (1995) Impaired hepatocanalicular organic anion transport in endotoxemic rats. Am J Physiol. 269: G427-434. [PubMed.]
- Demeule M, Jodoin J, Beaulieu E, Brossard M, Beliveau R. (1999) Dexamethasone modulation of multidrug transporters in normal tissues. FEBS Lett. 442: 208-214. [Ref.]
- Stapelbroek JM, van Erpecum KJ, Klomp LW, Houwen RH. Liver disease associated with canalicular transport defects: current and future therapies. J Hepatol 52: 258-71 [PubMed.]
- Stapelbroek JM, Erpecum KJV, Klomp LW, Houwen RH. (2010) Liver disease associated with canalicular transport defects: current and future therapies. J Hepatol. 52(2): 258-271. [PubMed.]
- Yoon EL, Yim HJ, Kim SY, Kim JH, Lee JH, et al. (2010) Clinical courses after administration of oral corticosteroids in patients with severely cholestatic acute hepatitis A) three cases. Korean J Hepatol. 16: 329-333. [PubMed.]