>Corresponding Author : Emadodin Darchini-Maragheh
>Article Type : Case Report
>Volume : 2 | Issue : 2
>Received Date : 26 June, 2022
>Accepted Date : 10 July, 2022
>Published Date : 20 July, 2022
>DOI : https://doi.org/10.54289/JCRMH2200109
>Citation : Kiafar B, Tayyebi M and Darchini-Maragheh E. (2022) A Case Report of Coronavirus (COVID-19) Infection-Induced Pseudocellulits: A Microthrombotic Related Dermatosis. J Case Rep Med Hist 2(2): doi https://doi.org/10.54289/JCRMH2200109
>Copyright : © 2022 Kiafar B, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Case Report | Open Access | Full Text
Cutaneous Leishmaniasis Research Center, Mashhad University of Medical Sciences, Mashhad, Iran
*Corresponding author: Emadodin Darchini-Maragheh, Cutaneous Leishmaniasis Research Center, Mashhad University of Medical Sciences, Mashhad, Iran
Abstract
Various skin manifestations have been reported with Corona Virus Disease 2019 (COVID-19) infection. Microthrombotic effect of the infection clarify some related dermatoses such as chilblains, acral ischemia and livedoreticularis. We describe here a case of acral erythema and edema, different from the pseudo chilblain previously described in literature, as related dermatoses of COVID-19.
Keywords: COVID-19; Skin Diseases; Diagnosis
Abbreviations: COVID-19: Corona Virus Disease 2019, WHO: World Health Organization, ARDS: Acute Respiratory Distress Syndrome, CFR: Case Fatality Rate, ICU: Intensive Care Unit, HRCT: High-Resolution Computed Tomography
Introduction
During late 2019, Clusters of unknown cause pneumonia reported from Wuhan, China, which now is named Corona Virus Disease 2019 (COVID-19) by the World Health Organization (WHO), and on 30 January, is declared as a Public Health Emergency of International Concern. On 30 January, 2020, the World Health Organization (WHO) declared it to be a Public Health Emergency of International Concern. As of 1 June 2020, more than 216 countries and territories, 5,704,736 cases of COVID-19 and 357,736 deaths have been confirmed all over the world, of which the number of confirmed patients has gradually decreased in Iran but is increasing rapidly in USA and Europe [1].
Fever, cough, and muscle soreness or fatigue were reported to be the most common symptoms, followed by dyspnea, and myalgia. Acute respiratory distress syndrome (ARDS) is the most common complication among patients. The overall estimated proportion of case fatality rate (CFR) in two recent systemic systematic reviews were reported as 3.6% and 4.3% [2,3].
Rapid spread of the disease among countries encountered the physicians with a vast array of clinical presentation, including cutaneous manifestations. There are increasing reports of various cutaneous manifestations in COVID-19 as well as rare cases of skin rashes as an early symptom of the infection.
In a recent large prospective nationwide study, dermatological manifestations of COVID-19 were described and classified in five clinical patterns including: Acral erythema and edema with some vesicles or pustules (pseudochillblain); other vesicular eruptions; Urticarial lesions; other maculopapules; Livedo or necrosis [4].
In Iran, as one of the first countries to be involved with the outbreak, lots of dermatologic consultations have been performed among COVID-19 patients until now due to probable coincidental skin lesions, as well as drug reactions and probable COVID -19 specific lesions. We describe a case of acral erythema and edema, different from the pseudo chilblain previously described in the literature, as a preliminary symptom of COVID -19.
Case presentation
A 59-year-old female was referred to emergency department of Imam Reza hospital, Mashhad, Iran due to slowly progressive lower legs erythema and edema, as well as nausea, vomiting, stomach ache, constipation, malaise and myalgia within two previous weeks. Her medical history was notable for a completely treated pulmonary tuberculosis 8 years ago. Due to deterioration of general condition and progressive dyspnea, she was admitted in COVID-19 zone of the hospital suspicious to atypical presentation of COVID -19. During the hospitalization, blood oxygen saturation level was decreased to 70% and thus, she was admitted to intensive care unit (ICU). Lung High-Resolution computed tomography (HRCT) and chest x-ray revealed bilateral lung involvement which was more severe at the right side (fig1 and 2). Laboratory data are summarized in table 1.
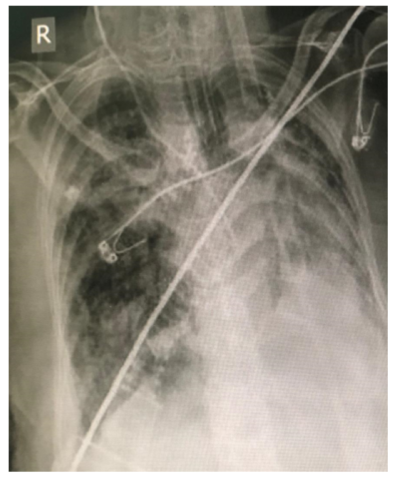
Figure 1: Chest radiography of COVID-19 patient with pseudocellulitis lesions in legs (AP technique). Reticular pattern and linear atelectasis bands in right lung field and consolidation in lower lobe of left lung is visible
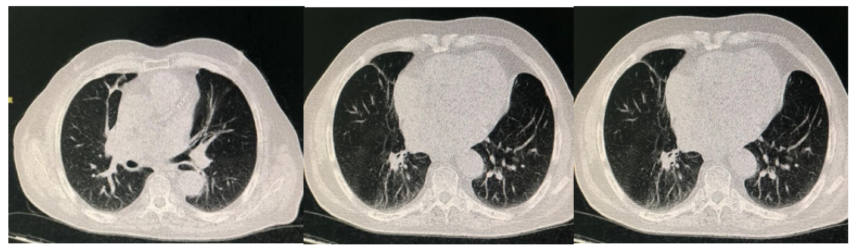
Figure 2: Lung High-resolution computed tomography (HRCT) in a COVID-19 patient and pseudocellulitis lesions in legs. Fibrotic lesions and cavitation in right lung are due to old tuberculosis.
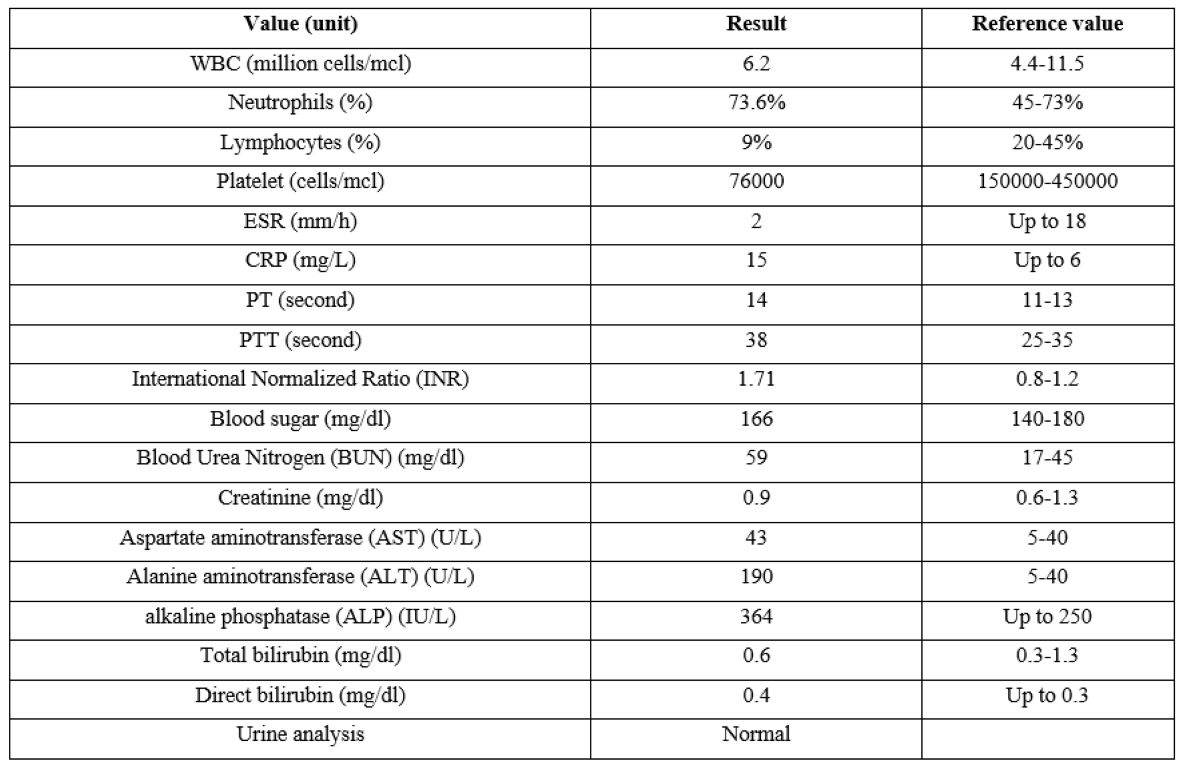
Table 1: Laboratory data of COVID-19 patient admitted with pseudo cellulitis lesions in lower legs
Dermatologic examination revealed symmetrical erythema and 2+ pitting edema of lower legs. The lesion was slightly colder than the normal adjacent skin, and rather tender. Dorsalis pedis and tibilais posterior artery pulses were symmetrically detected, however, were slightly weak, probably due to skin edema. Any signs of venous insufficiency including pain, varicose veins, hemosiderin deposition, pruritus, scaling, eczematous pattern and weeping were absent. Lesions in each leg had well defined border suggested clinical presentation of psedocellulitis (fig 3).

Figure 3: Patient with COVID-19 infection and bilateral pseudocellulitis in lower limbs (before treatment).
The only pathologic report of Doppler ultrasound study of legs was mild edema and increased echogenicity of subcutaneous tissue. Abdominal sonography was normal.
The patient underwent ICU care and administered oral hydroxychloroquine (200 mg twice daily), oral azithromycin (250 mg daily) and acetaminophen for one week. As her general condition, blood oxygen saturation and underline disease improved during hospitalization, dermatological manifestation of bilateral pseudocellulitis was subsequently improved and skin lesions were remarkably ameliorated (fig 4).

Figure 4: Patient with COVID-19 infection and bilateral pseudocellulitis in lower limbs (after treatment of underlying disease).
Discussion:
During the COVID-19 pandemia, histological findings of fibrin thrombi within the pulmonary vasculature. Additional reports were compatible with thrombi in pulmonary, bronchial, and small lung veins of postmortem COVID-19 infected lung autopsies. These reports suggested a prothrombotic effect of the COVID-19 [5]. Multiple organ thrombosis, associated with microcirculation disturbance and polyangiitis was also reported in an autopsy in a COVID-19 patient [6].
Previous reports on skin manifestation of COVID-19 were in accordance with microthrombotic effect of the infection and hyperthrombotic state. Lesions have not been similar to other respiratory viral infection skin manifestation.
Increasing reports of chilblain like lesions were noted among dermatologic consultations. The manifestation was during the warmer springtime and occurred in patient with no history of other cold induced dermatoses and connective tissue diseases, suggested a COVID-19 related dermatosis. Although most of the first reported cases were asymptomatic, further reports strengthened the association. Sparse histopathological studies of the lesions were similar to chilblain lupus, including an interface dermatitis with superficial and deep lymphoplasmacytic infiltration and lack of significant dermal edema [7].
Pseudo chilblain has been more commonly noticed in younger patients, associated with milder disease course, and occurred in late course of the disease. It has been described clinically as asymmetrical acral areas of erythema and edema with vesicles and/or pustules and sometimes purpuric areas [8]. In contrast, our presented case had symmetrical uniform erythema and edema and also was characterized as severely infected patient who admitted in ICU ward.
Acral ischemia with finger – toe cyanosis as well as livedoreticularis have also been reported among more severe COVID-19 patients as microthrombotic related dermatoses [9]. There has been no previous report of psedocellulitis pattern as microthrombotic, and/or inflammatory related dermatosis of COVID-19 infection.
Occlusion of skin microvascular system due to micro thrombosis reduces cutaneous blood flow and in known as the main pathogenesis. Histopathological evidences of both skin and lung biopsies of COVID-19 patients suggest activation of the alternative and lectin based complement [10]. We believe that the mentioned presentation in our patient is also different from acrocyanosis and other previous microthrombotic related dermatoses of COVID-19. The lesion was erythematous and edematous with a clear cut off from normal skin.
Since further histopathological studies were not possible, we cannot shed light on particular pathogenesis of the opinion. Nevertheless, with regard to the patient’s abnormal coagulation tests, we therefore hypothesize that bilateral pseudocellulitis presentation of the patient could be a manifestation of microthrombotic related dermatoses of COVID-19. Treatment of underlying disease would be helpful in reducing cutaneous COVID-19 dermatoses. Besides, it was previously suggested antithrombotic therapy in severe patients to reduce thrombotic and microthrombotic complications.
Since the spectrum of dermatological presentations of COVID-19 rapidly widens, it is advised to dermatologists to be updated and vigilant in dermatology clinics, in order to hasten the diagnosis and take safety precautions.
References
- WHO main website. 2020. [Ref.]
- Fu L, Wang B, Yuan T, et al. (2020) Clinical Characteristics of Coronavirus Disease 2019 (COVID-19) in China: A Systematic Review and Meta-Analysis. J Infect Jun. 80(6): 656-665. [PubMed.]
- Sun P, Qie S, Liu Z, et al. (2020) Clinical characteristics of 50466 hospitalized patients with 2019-nCoV infection. [Ref.]
- Casas CG, Català A, Hernández GC, et al. (2020) Classification of the cutaneous manifestations of COVID‐19: a rapid prospective nationwide consensus study in Spain with 375 cases. British Journal of Dermatology. 183(1): 71-77. [PubMed.]
- Giannis D, Ziogas IA, Gianni P. (2020) Coagulation disorders in coronavirus infected patients: COVID-19, SARS-CoV-1, MERS-CoV and lessons from the past. J Clin Virol. 127: 104362. [Ref.]
- Xiang-hua Y, Le-min W, Ai-bin L, et al. (2010) Severe Acute Respiratory Syndrome and Venous Thromboembolism in Multiple Organs, Am. J Respir Crit Care Med. 182: 436-437. [PubMed.]
- Kolivras A, Dehavay F, Delplace D, et al. (2020) Coronavirus (COVID-19) infection-induced chilblains: A case report with histopathologic findings. JAAD Case Rep. 6(6): 489-492. [PubMed.]
- Alramthan A, Aldaraji W. (2020) Two Cases of COVID-19 Presenting with a Clinical Picture Resembling Chilblains: First report from the Middle East. Clin Exp Dermatol. [PubMed.]
- Zhang Y, Cao W, Xiao M, et al. (2020) Clinical and coagulation characteristics of 7 patients with critical COVID-2019 pneumonia and acro-ischemia. Zhonghua xue ye xue za zhi= Zhonghua xueyexue zazhi. 28: 41: E006. [PubMed.]
- Magro C, Mulvey JJ, Berlin D, et al. (2020) Complement associated microvascular injury and thrombosis in the pathogenesis of severe COVID-19 infection: A report of five cases. ransl Res. 220: 1-13. [PubMed.]