>Corresponding Author : Sofia Kafki
>Article Type : Review Article
>Volume : 1 | Issue : 1
>Received Date : 21 June, 2023
>Accepted Date : 05 July, 2023
>Published Date : 19 July, 2023
>DOI : https://doi.org/10.54289/JSSS2300101
>Citation : Kafki S, Chrysikos D, Manoli A and Troupis T. (2023) Anatomical Variations of the External Branch of the Superior Laryngeal Nerve and its Correlations with the Superior Thyroid Artery and the Upper Pole of the Thyroid Gland: A Review of the Literature. J Surg Surg Spec 1(1): doi https://doi.org/10.54289/ JSSS2300101
>Copyright : © 2023 Kafki S, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Review Article | Open Access | Full Text
1Otolaryngology, Health Centre of Philadelphia, Athens, GRC
2Anatomy/Assistant Professor, Department of Anatomy, School of Medicine, National and Kapodistrian University of Athens, Athens, GRC
3Otolaryngology, Thoracic Diseases General Hospital of Athens ‘Sotiria’, Athens, GRC
4Anatomy/Professor, Department of Anatomy, School of Medicine, National and Kapodistrian University of Athens, Athens, GRC
*Corresponding author: Sofia Kafki, Otolaryngology, Health Centre of Philadelphia, Athens, GRC
Abstract
Injury to the external branch of the superior laryngeal nerve (EBSLN) following thyroid or parathyroid surgery often results in devastating voice changes especially noticed by patients who use their voice professionally. The external branch arises from the vagus nerve which provides the motor supply to the cricothyroid muscle, an exclusive tensor of the vocal cords. The course of the EBSLN is subject to great anatomic variability. Damage to the nerve occurs during improper ligation of superior thyroid vessels close to the upper pole of thyroid gland in up to 58% of patients undergoing thyroid surgery. Thus, a thorough knowledge of the anatomy of the EBSLN and its variations, is essential requirement to minimize iatrogenic complications during surgery of the neck. Additionally, nerve monitoring methods have been developed to facilitate the localisation of the nerve, decreasing the possibility of nerve injury during thyroid surgery. The aim of this study is to analyze and review the anatomical variations of the EBSLN and its correlations with the superior thyroid artery and the upper pole of the thyroid gland. The literature search was performed during the period from February 1992 through November 2021.
The position of the EBSLN was classified according to the Cernea and Kierner classification.
Based on this classification, type 2a variant of EBSLN was the commonest followed by type 1. In addition, neuromonitoring allowed a higher identification rate than the visual identification.
Keywords: Ebsln; Superior Thyroid Artery; Upper Pole; Thyroid Gland; Cernea/Kierner Classification; Intraoperative Neuromonitoring
Abbreviations: RLN: Recurrent Laryngeal Nerve, IBSLN: Internal Branch of the Superior Laryngeal Nerve, EMG: Electromyography, CMAP: Compound Muscle Action Potential, IONM: Intraoperative Nerve Monitoring, STA: Superior Thyroid Artery, CTM: Cricothyroid Muscle
Introduction
Numerous studies have emphasized the importance of preserving the recurrent laryngeal nerve (RLN) during thyroidectomy because injury of it can cause serious complications such as permanent or transient hoarseness, dysphasia and total vocal cord paralysis [1]. Due to the diversity of EBSLN, few approaches to identify and preserve the nerve during thyroid surgery have been established in the literature. The EBSLN innervates the cricothyroid muscle and its injury often results in hoarseness, inability to raise pitch, and voice fatigue mainly detected in professional singers, teachers and public speakers [2]. The EBSLN runs close to the superior thyroid artery in relation to the upper pole of thyroid gland. The injury of the nerve is possible during the sectioning of the superior thyroid vessels throughout thyroid surgery. In most circumstances, the EBSLN passes above the superior thyroid pole, but many variations have been reported in literature. The EBSLN was categorized according to the proposed classification by Cernea et al. [3] and Kierner et al. [4]. The aim of this study was to review the surgical anatomy and variations of the EBSLN and its relevance to the superior thyroid pole and assess the role of neuromonitoring in detecting the nerve during thyroid surgery. Hence, a thorough understanding of EBSLN anatomy and its possible variations, is the key to achieve a safe and effective surgery.
Surgical Anatomy
Thyroid gland
The thyroid gland develops as an endodermal downgrowth from the 1st and 2nd pharyngeal pouches [5]. The thyroid gland takes its name from the Greek words ‘thyreos’ (shield) and ‘edidos’ (form) because of its shape and position in the anterior central neck [6,7]. It weighs about 15-25 grams. It is closely associated with several vital structures such as parathyroid glands, recurrent laryngeal nerves, external laryngeal nerves and thyroid vessels [8,9]. The arterial supply of thyroid comes from the superior and inferior thyroid arteries. The superior thyroid artery is normally the 1st branch of the external carotid artery. It descends down and anteriorly to reach the superior pole of the thyroid gland. Along part of its course, the artery parallels the external branch of the superior laryngeal nerve. At the superior pole the artery divides into anterior and posterior branches. The anterior branch parallels the medial border of the lobe and anastomoses in the midline with the anterior branch of the other side. The posterior branch anastomoses with branches of the inferior thyroid artery. From the posterior branch, a small parathyroid artery passes to the superior parathyroid gland. The inferior thyroid artery usually arises from the thyrocervical trunk of the subclavian artery. It bends medially and passes posteriorly to the carotid sheath to reach the inferior pole of the thyroid either anteriorly or posteriorly to the RLN. Then, the artery divides into two branches. The superior branch anastomoses with the posterior branch of the superior thyroid artery. The inferior branch supplies the lower pole of the gland along with the inferior parathyroid glands. On the right, the inferior thyroid artery is absent in about 2% of individuals. On the left, it is absent in about 5%. The artery is occasionally double. Approximately 10% of people have small unpaired thyroid ima artery. It may arise from brachiocephalic trunk, aortic arch or right common carotid artery. It ascends on the anterior surface of the trachea and continues to the thyroid isthmus. A potential source of bleeding during tracheotomy is the presence of this artery [6]. A complex of veins form under the thyroid capsule. The superior thyroid vein which flows into the internal jugular vein accompanies the ipsilateral artery. The middle thyroid vein arises on the lateral surface of the gland at about two-thirds of its anteroposterior extent. No artery accompanies it. This vein enters either the internal jugular or the innominate vein. The inferior thyroid vein is the largest and most variable of the thyroid veins. It accompanies the thyroid ima artery (if artery is present) [10]. Lymphatic drainage parallels the venous drainage. The upper part drains into the upper deep cervical lymph nodes (from the prelaryngeal nodes; Delphian lymph node), the lower part drains into the lower deep cervical lymph nodes (from the pre-tracheal and paratracheal nodes) and the isthmus drains into the brachiocephalic lymph nodes [11]. Thyroid gland receives its innervation from the superior, middle and inferior cervical sympathetic ganglia (from the sympathetic trunk) which are vasomotor in function [12].
EBSLN anatomy and variations
The SLN arises from the inferior ganglion of the vagus nerve.Within 1.5cm of its origin and posteromedially to the internal carotid artery, it descends antero-inferiorly to reach the thyrohyoid membrane. It bifurcates into external laryngeal branch and internal laryngeal branch at the level of the hyoid bone. The internal branch of the superior laryngeal nerve (IBSLN) pierces the thyrohyoid membrane along with superior laryngeal vessels. This nerve divides into three branches that communicate with the RLN. The IBSLN provides sensory innervation of the supraglottic larynx. Injuries to the internal branch are uncommon during thyroidectomy [13].
The EBSLN is a smaller, motor branch that travels anteriorly and inferiorly along the lateral surface of the inferior constrictor muscle and the branches of superior thyroid artery. Then it descends anteriorly and medially towards the larynx to innervate the cricothyroid muscle. The nerve bifurcates to innervate the two parts of the muscle which are the pars recta and the pars oblique. The cricothyroid muscle increases the longitudinal tension of the vocal folds and raises the pitch of the voice. Injury to the EBSLN causes paralysis of cricothyroid muscle with consequent hoarseness, vocal fatigue, changes in the pitch of the voice and volume changes on loud phonation [14]. However, it is not yet known whether SLNs provide innervation to the thyroarytenoid [15]. The relation of the nerve to the upper pole and superior thyroid artery is extremely variable. This condition increases the risk of nerve damage during thyroidectomy, parathyroidectomy, carotid endarterectomy or anterior cervical spine procedures. For that reason, the superior thyroid artery needs to be ligated and individually isolated just near the upper pole where it is not so closely related to the nerve as it is at its origin. Apart from that, visual identification of the nerve is needed before the ligature of the upper pole. Also, the use of neuromonitoring to the margin of the cricothyroid muscle has improved detection rates [16,17]. A classification of the EBSLN with respect to the upper pole and its relation to superior thyroid artery is the most important landmark the surgeons need to raise awareness during thyroid surgery. The landmark drawn by Cernea et al. [3] is the usual position of the superior pole of the thyroid, but it changes with ethnic differences and size of thyroid gland. Later Kierner et al. added a 4th type [4] (figure 1):
Type 1: Nerve crosses STA more than 1cm above the superior pole (Cernea and Kierner)
Type 2a/2: Nerve crosses STA<1cm above the superior pole (Cernea/Kierner)
Type 2b/3: Nerve crosses STA<1cm below the superior pole (Cernea/Kierner)
Type 4 (Not identified): Nerve runs dorsally to the superior thyroid pedicle (Kierner)
The Cernea et al. classification is the most widely accepted system in identification and documentation of EBSLN in relation to the superior pole and superior thyroid vessels. It has been reported 60% of type 1, 17% of type 2a, 20% of type 2b, and 3% of type Ni (Not identified) EBSLNs [3].
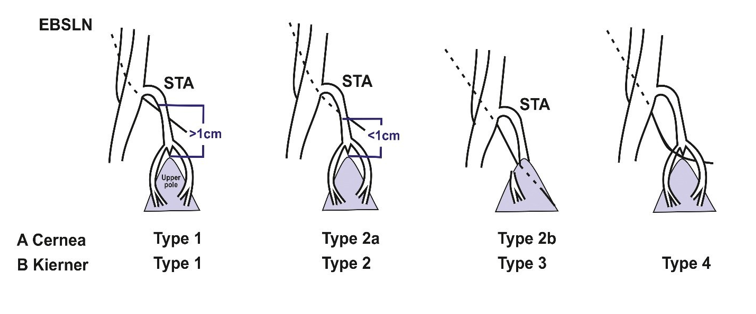
Figure 1: Cernea and Kierner classification
Kierner et al. classification is similar to Cernea. However, a 4th type was added which described 14% of cases where the EBSLN could not be identified since it descended more dorsally. It is claimed that this type may have been partly responsible for the type Ni findings of Cernea’s classification [4].
The Friedman et al. classification described the EBSLN in relation to the inferior pharyngeal constrictor muscle before its entry into cricothyroid muscle as follows [18]:
Type 1: EBSLN runs superficially to the inferior constrictor muscle, along with the superior thyroid vessels
Type 2: EBSLN penetrates the inferior constrictor muscle in the lower portion of the muscle
Type 3: EBSLN plunges into the inferior constrictor (‘buried’)
The Friedman et al. classification is based on the distal identification of the EBSLN. It was reported that in more than 85% of cases, the nerve could be identified in the junction of the inferior constrictor muscle and cricothyroid muscle. However, prevalence data for each variant was not provided [18].
Block et al. reported the positional interrelationship of EBSLN to superior thyroid artery including variants of other classifications [19]:
Type A: The nerve travels medial to the superior thyroid artery
Type B: The nerve travels deep to the inferior pharyngeal muscle (similar to Friedman type 3)
Type C and D: The nerve travels between the branches of the superior thyroid artery (similar to Lennquist variants described below)
Type E: The nerve crosses below the apex of superior thyroid pole (similar to Cernea type 2b and Kierner type 3)
Block provides no information on prevalence [19].
According to Lennquist et al. the EBSLN was classified as [20]:
Type 1: Medial to the origin of the superior thyroid artery (most common)
Type 2: Lateral to the origin of the superior thyroid artery
In about 20% of EBSLNs were identified laterally to the superior thyroid artery and distally after inferior constrictor muscle dissection, but this would not be recommended. They mentioned that some EBSLNs run among the branches of the superior thyroid artery and no further subclassification was needed [20].
Selvan e al. used electromyography (EMG) to identify and map the nerve according to clinical variations by recording the compound muscle action potential (CMAP) [21]:
Type 1a: EBSLN can be found within 1 cm of the entry of the vessels into the gland either anterior or between the branches of the superior thyroid vessels and internally 3 cm of the cricoid cartilage
Type 1b: EBSLN can be identified posterior to the vessels but inside 1 cm from the entrance of the vessels into thyroid
Type 2: EBSLN can be appeared inwardly 1 to 3 cm from the entrance of the vessels into thyroid or deep down 3 to 5 cm from the cricoid cartilage (most frequent)
Type 3: EBSLN can be found between 3 and 5 cm of the entry of the vessels into the gland or more than 5 cm of the cricoid cartilage
It was found 9% of nerves of type 1a, 3% of type 1b, 68% of type 2 and 20% of type 3 [21].
In addition, laryngeal nerves communications have been studied between the internal and recurrent laryngeal nerves; external and recurrent laryngeal nerves as well as, internal and external laryngeal nerves. Specifically, the communication between the EBSLN and the RLN (the ‘’communicating nerve’’) occurred in the piriform fossa. After the EBSLN supplied the cricothyroid muscle, it passed through this muscle to enter the larynx, where it connected with the anterior branch of RLN to innervate one-third of the anterior part of the thyroarytenoid muscle, which is the adductor of the ipsilateral vocal cord [22]. Also, neural communications have been described between external and internal laryngeal nerves (via a thyroid foramen) and between internal and RLN [23]. These variations may help explain the variable position of the vocal folds after vocal fold paralysis.
Identification and Preservation of EBSLN
The nerve is usually found in space of Reeves which is an avascular space between the upper pole of thyroid and cricothyroid muscle. Identification and opening up is important for preservation of EBSLN especially in the type 2b cases, where the nerve is at risk of injury during ligation of the vessels close to the gland [24,25]. A medial dissection is performed at the upper pole. The ipsilateral lobe is given traction in a downward and outward direction thus opening up the sternothyroid- laryngeal triangle (Joll’s triangle). The triangle is bounded by sternothyroid muscle superiorly, upper lobe and superior thyroid vessels laterally and the inferior constrictor muscle and cricothyroid muscle medially [26]. The EBSLN is usually located medially, the superior thyroid vein on the lateral side and the superior thyroid artery in between [27] (figure 2).
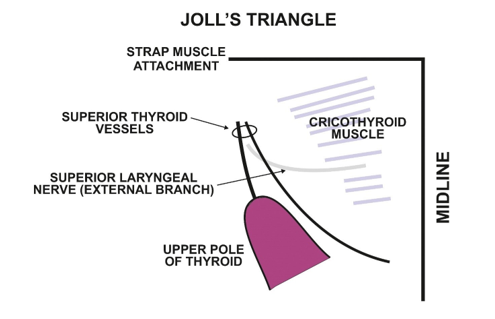
Figure 2: Joll’s triangle
Strap muscle is found superiorly, upper pole and superior thyroid vessels laterally and the cricothyroid muscle medially. The external branch of superior laryngeal nerve is usually located medially
Intraoperative nerve monitoring (IONM) of the EBSLN
Recent studies have shown that intraoperative monitoring can assist with identifying the EBSLN during superior thyroid pole surgical approach. The standard method of EBSLN monitoring is performed under general anesthesia via endotracheal tube using surface electrodes. It consists of an electromyography (EMG) that detects the adduction of the vocal folds. The monitor should be set for an appropriate event threshold at 50 μV and a stimulator probe (monopolar or bipolar) should be set on a value of 1mA. The EBSLN must be tested medially to the vascular pedicle of superior pole after the true positive stimulation with 1 mA (EMG response via cricothyroid muscle twitch). IONM contributes to voice preservation following thyroidectomy since its positive neural signal is useful for the declaration of the neural function and for identification of the EBSLN [28].
Materials and Methods
Eligible studies were identified by search of the PubMed/Medline, Medscape, Embase and Google Scholar bibliographical databases from February 1992 up to November 2021. The search included the following keywords: “external branch of superior laryngeal nerve AND superior thyroid vessels AND superior pole of thyroid gland AND Cernea/Kierner classification AND intraoperative neuromonitoring”.
Study selection criteria
The search was limited to studies published in English, French or German. Two investigators (SK and DC), working independently, reviewed the literature and cited data from each eligible study. All prospective and retrospective studies, were acceptable for this review. Articles that did not disclose the names of the authors were not evaluated. All references from the manuscripts were searched for further information.
The search strategy retrieved 3559 articles. Additional records identified through other sources (n=45). Following the removal of duplicates (n=342) and primary screening (n=3021), 241 of these were considered as eligible. The other studies were excluded (n=192) by applying exclusion criteria involved previous neck irradiation, full text articles not available, studies investigating RLN, postoperative injury assessment rather than identification of the EBSLN, incomplete data, conference abstracts and reviews. Finally, 49 of them were included in this literature review. Inclusion criteria comprised total lobectomy, subtotal thyroidectomy or hemithyroidectomy, primary or secondary procedure, with or without thyroid lesions.
Results
Cernea et al. [3] in 1992 proposed a classification system in identification of EBSLN in relation to the superior pole and superior thyroid vessels. 15 cadavers were used in this study, with 30 slightly enlarged thyroid poles being dissected. It has been reported 18 (60%) of type 1, 5 (17%) of type 2a, 6 (20%) of type 2b and 1(3%) of type Ni. The rate of direct visual classification was 100%. In 1998, Kierner et al. [4] dissected 52 hemilarynges from 31 cadavers. In type 1, 23 nerves (42%) were found, in type 2, 15 (30%), in type 3, 7 (14%) and in type 4, 7 (14%). In agreement with Cernea et al., type 1 was the most common. In 1995, Cernea et al. [29] studied 9 patients and analyzed 12 EBSLNs. The average weight of the specmens was 431 grams. Three (23%) were type 1, two (15%) type 2a, seven (54%) type 2b and one (8%) type Ni. It was claimed that the incidence of the type 2b EBSLN was higher among the population of large goiters. Aina and Hisham [30] reported 392 dissections in 317 patients in 2001. They presented 199 nerves (50.8%) in type 2a and they revealed that the identification rate of the EBSLN using IONM was 95%. Bellantone et al. [31] published 215 upper pole dissection in 215 patients in the same year. They saw 126 nerves (58%) in type 1 and 25 (11.6%) in type 4/Ni. The reported visual identification for the 190 EBSLNs was 88.4%. In 2002, Hurtado-Lopez et al., [32] reproduced 73 superior poles ligations in 73 patients. 39.7% of the 29 EBSLNs was related to type 2a and 5.8% of the 4 nerves to type 4/Ni. 100% of the nerves could be identified visually. Furlan et al., [33] performed 72 dissections in 36 cadavers and 34 (47%) type 1 nerves were found predominantly. In 2005, Hurtado -Lopez et al., [34] carried out 49 dissections in 29 patients and found equal number of 16 nerves (32.5%) in type 1 and 2a. 11 nerves (22.7%) of type 4/Ni could not be identified. They documented an identification rate of 97% under IONM. According to Ozlugdik et al. [35] among the 40 dissections in 20 cadavers, the prevalence of the nerve type 2a was as high as 60%. Pagedar et al. [36] showed that 48.3% of nerve type 2b was the most common in 112 patients that underwent 178 upper pole dissections while three (1.7%) nerves were type 4/Ni. They found an identification rate of 98.3% without neural stimulation. Chuang et al. [37] prescribed 86 dissections in 43 cadavers and 39.5% of the nerves were found in type 2a although 5 nerves (5.8%) were estimated in type 4/Ni. Whitfield et al. [38] reported that no type 2b nerves were seen while the prevalence of type 1 nerves was as high as 80% and 2 nerves (13%) were type 4/Ni. Hwang et al. [39] determined that the use of IONM in the intraoperative dissection of 92 upper poles in 50 patients recognized 100% of the nerves. Fiftytwo nerves (56.5%) were classified as type 2a. Pradeep et al. [40] analyzed 584 EBSLNs intraoperatively in 404 patients and found 71.4% nerves of type 1 and 8.9% of type 4/Ni. Barczynski M et al. [41] reported 210 thyroidectomies and 248 nerves visualized with IONM in 83.8%. 126 nerves (50.8%) type 1 showed prevalence. A retrospective evaluation of 456 patients (849 nerves) was addressed by Ravikumar et al. [42] The incidence of type 2a (522) EBSLN was higher in 57.2% of cases while 63 nerves (6.92%) were not identified (type 4/Ni). Dionigi et al. [43] studied 400 nerves among 206 patients and found that the presence of type 2b nerves (56.7%) were more prevalent as compared to the other types. Uludag M et al. [44] included the data of 221 patients and a total of 374 nerves (95.2%) were identified with IONM. In a randomized prospective clinical trial of Uludag et al. [45], a total of 133 patients who underwent thyroidectomy, assigned to 2 groups. In group 1 (65 patients, 105 nerves) there was no effort to visualize the EBSLN. In group 2 (68 patients, 106 nerves), IONM identified 65.1% of EBSLNs. In group 2, 72 nerves (67.9%) type 2a were mostly found. Gavid et al. [46] showed type 1 (8 nerves) in 62.5% of 4 cadavers dissection. Joshi et al. [47] reported 94 EBSLNs in 79 patients with type 2a (46.8%) predominance. Menon et al. [24] in 2017 and Aygun et al. [48] in 2020, evaluated 191 and 200 EBSLNs intraoperatively in 100 and 126 patients respectively and reported a type 2a nerve prevalence rate of 61% and 68% subsequently. On the contrary, Ahmad et al. [49] and Iwata et al. [50] showed a type 1 nerve prevalence rate of 53.2% and 50.8% in 50 and 80 patients during thyroidectomies. Devaraja et al. [51] conducted a cadaveric study and included 12 nerves from 8 cadavers. The prevalence of type 2a nerves was higher. In the study by Del Rio et al. [52], the prevalence of type 1 EBSLN among 88 patients of 176 nerves examined, was 43.3%. Dubey et al. [53], reported a type 1 EBSLN prevalence rate of 61.1% in 50 patients while 59 EBSLNs were detected. Jonas et al. [54] determined that 37.9% of EBSLNs were identified by IONM. Page et al. [55] identified 20% of nerves by IONM. Mustafa et al. [56] documented visual identification only in 75.2% of nerves. Loch-Wilkinson et al. [57], Inabnet et al. [58], Lifante et al. [59], Masuoka et al. [60], Darr et al. [61], Kandil et al. [62], Hodnett et a. [63], Glover et al. [64], Lee et al. [65], Hurtado-Lopez et al./2016 [66], Aygun et al./2017 [67], Wang et al. [68] and Aleksova et al. [69] found that IONM recognized 87%, 53.3%, 65.7%, 89.2%, 100%, 54.2%, 67%, 97.2%, 98.5%, 97.5%, 65.6%, 98.5% and 96.8% of the EBSLNs, respectively. Gurleyik E&Gurleyik G/2017 et al. [70] reported only visual identification in 66.9% of nerves. Zhang et al. [71] recognized 94.4% (group 1) and 83.1% (group 2) of EBSLN, respectively by IONM. Gurleyik E&Gurleyik G/2021 et al. [72] documented only visual identification in 64.3% of EBSLNs.
Discussion
The external branch of superior laryngeal nerve (EBSLN) is closely related to the superior thyroid artery (STA) and upper pole of thyroid. This topographic relationship represents a key point of EBSLN identification during thyroid surgery. The EBSLN arises together with internal branch from the superior laryngeal nerve, which is a branch of the vagus nerve. It travels inferiorly, passing superficially to the inferior constrictor muscle and finally it terminates and innervates the cricothyroid muscle (CTM) which tenses the vocal cord [13]. In addition, the nerve is identified in the Joll’s triangle (sternothyroid laryngeal triangle) which is bounded laterally by upper pole of thyroid gland and the vessels, superiorly the attachment of the strap muscles and medially by the midline. The floor is formed by the CTM. The EBSLN lies within this triangle [26,27]. The techniques used for the identification of the EBSLN mentioned in literature include the use of nerve monitoring, the inspection of the distal part of the inferior constrictor muscle and individual ligation of the superior thyroid vessels [31].
Common symptoms associated with damage of the EBSLN are loss of pitch of the voice, diminished vocal frequency and easy fatigability of voice which may result in decreased quality of life, particularly for those voice professionals [14]. Therefore, preservation of this nerve is one of the critical steps of thyroid surgery. The EBSLN passes under sternothyroid deep to superior thyroid vessels. As a result, there is a risk of nerve damage approximately in 58% of cases during the dissection of the upper pole [73]. The literature describes various classification systems of the EBSLN in relation to these anatomic structures. In the present study, the identification rate of EBSLN was considered by evaluating the relationship between the superior thyroid artery and EBSLN based on Cernea’s and Kierner’s classification [3,4]. In most studies, Cernea type 2a nerves were found to be the most prevalent type followed by type 1 nerves [2,24,30,32,35,37,39,42,44,45,47,51,53,67]. In cadaveric studies, type 1 nerves were most common followed by type 2a nerves and type 2b nerves [3,4,33,38,46,51]. The incidence of type 2a nerves in intraoperative studies was higher compared to type 1 and type 2b nerves [2,24,30,39,42,44,45,47,53,67]. In some studies, the EBSLN descended more dorsally than one would expect and its identification was more difficult. It has been stated by Kierner’s et al. that type 4 may be partially responsible for the type Ni findings of Cernea’s classification [3,4,29,31,32,34], [36-38], [40,42,47,49].
The use of IONM significantly improves EBSLN identification rates during thyroid surgery. The research of Hwang et al. [39] and Darr et al. [61] recognized 100% of the EBSLN by IONM. Aina&Hisham et al. [30], Hurtado-Lopez et al. [34.66], Glover et al. [64], Lee et al. [65], Uludag M.et al. [44], Wang et al. [68] and Aleksova et al. [69] identified more than 95% of the EBSLNs with intraoperative neuromonitoring. Darr et al. [61] could identify all the EBSLNs and observe significant EMG responses in 100% of cases. Barcynski et al. [41], Dionigi et al. [43], Loch-Wilkinson et al. [57], Masuoka et al. [60], Zhang et al. [71] compared visualization with IONM and found increased identification rate of EBSLN about 90% of cases. The metanalysis of Cheruiyot et al. [73] demonstrated that the identification rates of EBSLNs were 95.90% (95% CI 94.30-97.25) in studies that used intraoperative neuromonitoring techniques (IONM) versus to 76.56% (95% CI 69.34-83.08) in studies using only visual identification. However, the accuracy of IONM is dependent to the technical experience of the surgeons, such as setting up the IONM equipment and interpreting the results correctly, as well as, the comprehensive cooperation between surgeons and anesthesiologists [27]. The most technical problems are incorrect positioning of the surface electrodes on the endotracheal tube relative to the vocal cords but occur less frequently compared to RLN intraoperative neuromonitoring [44].
Conclusion
The present study aims to review published literature for anatomical variations of external branch of the superior laryngeal nerve in relation to the superior thyroid artery and superior pole considering Cernea and Kierner classification and the application of intraoperative neural monitoring. Based on this classification, type 2a variant of EBSLN was the commonest followed by type 1. In addition, neuromonitoring allowed a higher identification rate than the visual identification. The key point for identifying and preserving the nerve during surgery of the neck is attention to anatomic detail and vascular configuration associated with knowledge of the course of the EBSLN and anatomical variations as described by Cernea et al. and Kierner et al. classification. Additionally, the contribution of intraoperative neuromonitoring is obvious helpful in identifying EBSLN and ensuring motor function of the larynx especially in professional singers and speakers.
Additional Information Disclosures
Conflicts of interest: All authors declare the following:
Payment/services info: All authors have declared that no financial support was received from any organization for the submitted work.
Financial relationships: All authors have declared that they have no financial relationships at present or within the previous years with any organizations that might have an interest in the submitted work.
Other relationships: All authors have declared that there are no other relationships or activities that could appear to have influenced the submitted work.
References
- Monfared A, Gorti G, Kim D. (2002) Microsurgical anatomy of the laryngeal nerves as related to thyroid surgery. The Laryngoscope. 112: 386. [PubMed.]
- Athavale PK, Bokare BD, Ekhar VR. (2013) Identification and preservation of external branch of superior laryngeal nerve in thyroidectomy. Int J Phonosurg Laryngol. 3(2): 39-41. [Ref.]
- Cernea C, Ferraz AR, Nishio S, et al. (1992) Surgical anatomy of the external branch of the superior laryngeal nerve. Head Neck. 14: 380-383. [PubMed.]
- Kierner AC, Aigner M, Burian M. (1998) The external branch of the superior laryngeal nerve. its topographical anatomy as related to surgery of the neck. Arch Otolaryngol Head Neck Surg. 124(3). 301-303. [PubMed.]
- Stewart WB, Rizzolo L. (2012) Embryology and surgical anatomy of the thyroid and parathyroid glands. Surgery of the thyroid and parathyroid glands. 2: 17-21. [PubMed.]
- Skandalakis LJ, Skandalakis JE, Skandalakis PN. (2009) Surgical anatomy and technique. Springer Science and Business Media LLC. 2. 32-41. [Ref.]
- Mizrachi A, Swartzwelder CE, Sheha AR. (2015) Proposal for anatomical classification of the superior pole in thyroid surgery. J Surg Oncol. 112(1): 15-17. [Ref.]
- Rghurajsai M. Thyroid Surgery. (2022) Surgical anatomy. Journal of Universal Surgery. 10(9): 65. [Ref.]
- Mohebati A, Shaha AR. (2012) Anatomy of thyroid and parathyroid glands and neurovascular relations. Clin Anat. 25(1): 19-31. [PubMed.]
- Singh R. (2020) Surgical anatomy of thyroid gland- A comprehensive review. Basic Sciences of Medicine. 9(1). 10-14. [Ref.]
- Khatawkar AV, Awati SM. (2015) Thyroid gland - Historical aspects, Embryology, Anatomy and Physiology. IAIM. 2(9). 165-171. [Ref.]
- Bliss R, Gauger P, Leigh W, Delbridge L. (2000) Surgeon’s Approach to the Thyroid Gland. Surgical Anatomy and the Importance of Technique. World J. Surg. 24: 891-897. [PubMed.]
- Dekhou AS, Morrisson RJ, Gemechu JM. (2021) The superior laryngeal nerve and its vulnerability in surgeries of the neck. Diadnostics. 11. [Ref.]
- Kochilas X, Bibas A, Xenellis J. (2008) Surgical anatomy of the external Branch of the superior laryngeal nerve and its clinical significance in head and neck surgery. Clin. Anat. 21: 99-105. [PubMed.]
- Michael O, Dinesh C. (2014) Superior laryngeal nerve injury effects, clinical findings, prognosis, and management options. Current Opinion in Otolaryngology and Head and Neck Surgery. 22(6): 439-443. [Ref.]
- Yalcin B, Develi S, Tubbs RS. (2013) A detailed study of the relationship between the external laryngeal nerve and superior thyroid artery, including its glandular branches. Clinical Anatomy. 26: 814-822. [PubMed.]
- Potenza AS, Filho VJFA, Cernea CR. (2017) Injury of the external branch of the superior laryngeal nerve in thyroid surgery. Gland Surgery. 6(5): 552-562. [PubMed.]
- Friedman M, Savio PL, Ibrahim H. (2002) Superior laryngeal nerve identification and preservation in thyroidectomy. Arch Otolaryngol Head Neck Surg. 128(3): 296-303. [PubMed.]
- Block MA. (1999) Surgical therapy of thyroid tumours. Comprehensive Management of Head and Neck Tumours. Thawley S (ed), W.B. Saunders, Philadelphia, PA. 1721-1751. [Ref.]
- Lennquist S, Cahlin C, Smeds S. (1987) The superior laryngeal nerve in thyroid surgery. Surgery. (107): 999-1008. [PubMed.]
- Selvan B, Srinivasa B, Deepak A, et al. (2009) Mapping the compound muscle action potentials of cricothyroid muscle using electromyography in thyroid operations. Ann Surg. 250. 293-300. [PubMed.]
- Uludag M, Tanal M, Isgor A. (2018) A review of methods for the preservation of laryngeal nerves during thyroidectomy. Med Bull Sisli Etfal Hosp. 52(2): 79-91. [PubMed.]
- Naidu N, Lazarus L, Partab P, et al. (2014) Laryngeal nerve anastomoses. Folia Morphol. 73(1): 30-36. [PubMed.]
- Menon RR, Murali S, Nair CG, et al. (2017) Correlation between the Cernea classification of external branch of superior laryngeal nerve in relation to the ultrasound-based volume of thyroid gland. Indian Journal of Endocrinology and Metabolism. 21(6): 845-847. [Ref.]
- Babu RD, Paul D. (2022) Laryngeal nerves and voice change in thyroid surgery. Indian Journal of Surgical Oncology. 13(1): 99-108. [Ref.]
- Chintamani. (2017) A tale of two nerves in thyroid surgery. Indian J Surg. 79(5): 375-377. [Ref.]
- Zhao Y, Zhao Z, Zhang D, et al. (2021) Improving classification of the external branch of the superior laryngeal nerve with neural monitoring. a research appraisal and narrative review. Gland Surg. 10(9): 2847-2860. [Ref.]
- Barczyński M, Randolph GW, Cernea CR, et al. (2013) External branch of the superior laryngeal nerve monitoring during thyroid and parathyroid surgery. International Neural Monitoring Study Group standards guideline statement. Laryngoscope. 123 Suppl 4: 1-14. [PubMed.]
- Cernea CR, Nishia S, Hojaij FC. (1995) Identification of the External Branch of the Superior Laryngeal Nerve (EBSLN) in Large Goiters. American Journal of Otolaryngology. 16 (5): 307-311. [PubMed.]
- Aina EN, Hisham AN. (2001) External laryngeal nerve in thyroid surgery. is the nerve stimulator necessary? Eur J Surg. 167(9): 662- 665. [PubMed.]
- Bellantone R, Boscherini M, Lombardi CP, et al. (2001) Is the identification of the external branch of the superior laryngeal nerve mandatory in thyroid operation? Results of a prospective randomized study. Surgery. 130(6): 1055-1059. [Ref.]
- Hurtado-Lopez LM, Zaldivar-Ramírez FR. (2002) Risk of injury to the external branch of the superior laryngeal nerve in thyroidectomy. Laryngoscope. 112(4): 626-629. [PubMed.]
- Furlan JC, Cordeiro AC, Branda LG. (2003) Intrinsic risk factors that can enhance an iatrogenic injury of the external branch of the superior laryngeal nerve. Otolaryngol Head Neck Surg. 128: 396-400. [PubMed.]
- Hurtado-Lopez LM, Pacheco-Alvarez MI, Montes-Castillo MD, Zaldivar-Ramirez FR. (2009) Importance of the Intraoperative identification of the external branch of the Superior is and its clinical applications. Head Neck. 32(1): 53-57. [Ref.]
- Ozlugdik S, Acar UI, Apaydin N, Tekdemir I, Elhan A, et al. (2007) Surgical anatomy of the external branch of the superior laryngeal nerve. Clin Anat. 20: 387-391. [PubMed.]
- Pagedar NA, Freeman JL. (2009) Identification of the external branch of the superior laryngeal nerve during thyroidectomy. Arch Otolaryngol Head Neck Surg. 135: 360-362. [PubMed.]
- Chuang FJ, Chen JY, Shyu JF, et al. (2009) Surgical anatomy of the external branch of the superior laryngeal nerve in Chinese adults and its clinical applications. Head Neck. 32: 53-57. [PubMed.]
- Whitfield P, Morton RP, Al-Ali S. (2010) Surgical anatomy of the external branch of the superior laryngeal nerve. ANZ J Surg. 80(11): 813-816. [PubMed.]
- Hwang SB, Lee HY, Kim WY, Woo SU, Lee JB, et al. (2012) The anatomy of the external branch of the superior laryngeal nerve in Koreans. Asian J Surg. 36(1): 13-19. [PubMed.]
- Pradeep PV, Jayashree B, Harshita SS. (2012) A closer look at laryngeal nerves during thyroid surgery. a descriptive study of 584 nerves. Anat Res Int. 1-6. [PubMed.]
- Barczynski M, Konturek A, Stopa M, Honowska A, Nowak W. (2012) Randomized controlled trial of visualization versus neuromonitoring of the external branch of the superior laryngeal nerve during thyroidectomy. World J Surg. 36(6): 1340-1347. [PubMed.]
- Ravikumar K, Sadacharan D, Muthukumar S, Mohanpriya G, Hussain Z, et al. (2016) EBSLN and factors influencing its identification and its safety in patients undergoing total thyroidectomy. a study of 456 cases. World J Surg. 40(3): 545-550. [PubMed.]
- Dionigi G, Kim HY, Randolph GW, Wu CW, Sun H, et al. (2015) Prospective validation study of Cernea classification for predicting EMG alterations of the external branch of the superior laryngeal nerve. Surg Today. 46(7): 785-791. [PubMed.]
- Uludag M, Aygun N, Kartal K, Besler E, Isgor A. (2016) Is intraoperative neural monitoring necessary for exploration of the superior laryngeal nerve? Surgery. 161(4): 1129-1138. [PubMed.]
- Uludag M, Aygun N, Kartal K, Citgez B, Besler E, et al. (2016) Contribution of intraoperative neural monitoring to reservation of the external branch of the superior laryngeal nerve. a randomized prospective clinical trial. Langenbeck's Arch Surg. 402(6): 965-976. [PubMed.]
- Gavid M, Dubois MD, Larivé E, Prades JM. (2017) Superior laryngeal nerve in thyroid surgery. anatomical identification and monitoring. Eur Arch Otorhinolaryngol. 274(9): 3519- 3526. [PubMed.]
- Joshi RR, Rijal AS, Shrestha KK, et al. (2017) Identification and preservation of external branch of the superior laryngeal nerve during thyroid surgeries at NMCTH. J Coll Med SciNepal. 13(3): 306-310. [Ref.]
- Aygun N, Demircioglu AS, Demircioglou ZG, et al. (2020) Factors influencing the relationship of the external branch of the superior laryngeal nerve with the superior pole vessels of the thyroid gland. Med Bull Sisli Etfal Hosp. 54(4): 469-474. [Ref.]
- Ahmad R, Saraf A, Kishore K, et al. (2020) Relation superior laryngeal nerve and superior thyroid artery with superior pole of thyroid during thyroid surgery. Indian Journal of Otolaryngol Head Neck Surg. 74: 2095-2098. [PubMed.]
- Iwata AJ, Liddy W, Barczynski M, et al. (2021) Superior laryngeal nerve signal attenuation influences voice outcomes in thyroid surgery. Laryngoscope. 131: 1436-1442. [PubMed.]
- Devaraja K, Punja R, Kalthur SG, et al. (2021) Unmapped landmarks around branches of the superior laryngeal nerve. An exploratory cadaveric study. Journal of Taibah U Med Sc. 16(3): 328-335. [PubMed.]
- Rio PD, Bonati E, Loderer T, et al. (2021) Can we routinely identify the external branch of the superior laryngeal nerves with neural monitoring? A prospective report on 176 consecutive nerves at risk. Updates in Surgery. 73: 2275-2281. [Ref.]
- Dubey T, Sigdal B, Nepali R, et al. (2021) Cernea’s classification of the External Branch of the Superior Laryngeal Nerve during Microscopic Thyroidectomy at Gandaki Medical College, Pokhara. JGMC Nepal. 14(2): 133-136. [Ref.]
- Jonas J, Bahr R, et al. (2000) Neuromonitoring of the external branch of the superior laryngeal nerve during thyroid surgery. Am J Surg. 179(3): 234-236. [PubMed.]
- Page C, Laude M, Legars D, et al. (2004) The external laryngeal nerve. surgical and anatomical considerations. Surg Radiol Anat. 26: 182-185. [PubMed.]
- Mustafa A, Bokare B. (2006) Surgical anatomy of external branch of superior laryngeal nerve (EBSLN) in thyroid surgery. Int J Biomed Adv Res. 7(10): 493-496. [Ref.]
- Loch-Wilkinson TJ, Stalberg PLH, Sidhu S, et al. (2007) Nerve stimulation in thyroid surgery. is it really useful? Anz J.Surgery. 77: 377-380. [PubMed.]
- Inabnet WB, Murry T, Dhiman S, Aviv J, Lifante JC. (2009) Neuromonitoring of the external branch of the superior laryngeal nerve during minimally invasive thyroid surgery under local anesthesia. a prospective study of 10 patients. Laryngoscope. 119(3): 597-601. [PubMed.]
- Lifante JC, McGill J, Murry T, et al. (2009) A prospective, randomized trial of nerve monitoring of the external branch of the superior laryngeal nerve during thyroidectomy under local/regional anesthesia an IV sedation. Surgery. 146: 1167-1173. [PubMed.]
- Masuoka H, Miyauchi A, Higashiyama T, Yabuta T, Fukushima M, et al. (2014) Prospective randomized study on injury of the external branch of the superior laryngeal nerve during thyroidectomy comparing intraoperative nerve monitoring and a conventional technique. Head Neck. 37(10): 1456-1460. [PubMed.]
- Darr EA, Tufano RP, Ozdemin S, et al. (2014) Superior laryngeal nerve quantitative intraoperative monitoring is possible in all thyroid surgeries. Laryngoscope. 124: 1035-1041. [PubMed.]
- Kandil E, Mohamed SE, Deniwar A, et al. (2015) Electrophysiologic identification and monitoring of the external branch of superior laryngeal nerve during thyroidectomy. The laryngoscope. 125(8): 1996-2000. [PubMed.]
- Hodnett BL, Schmitt NC, Clayburgh DR, Burkowsky A, Balzer J, et al. (2015) Superior laryngeal nerve monitoring using laryngeal surface electrodes and intraoperative neurophysiological monitoring during thyroidectomy. Clin Anat. 28(4): 460-466. [PubMed.]
- Glover AR, Norlén O, Gundara JS, Morris M, Sidhu SB. (2015) Use of the nerve integrity monitor during thyroid surgery aids identification of the external branch of the superior laryngeal nerve. Ann Surg Oncol. 22(6): 1768-1773. [PubMed.]
- Lee J, Fraser S, Glover A, Sidhu S. (2017) Prospective evaluation of the utility of routine neuromonitoring for an established thyroid surgical practice. ANZ J Surg. 87(10): E138-E142. [PubMed.]
- Hurtado-Lopez LM, Díaz-Hernández PI, Basurto-Kuba E, Zaldívar-Ramírez FR, PulidoCejudo A. (2016) Efficacy of intraoperative neuro-monitoring to localize the external branch of the superior laryngeal nerve. Thyroid. 26(1): 174-178. [PubMed.]
- Aygün N, Uludağ M, İşgör A. (2017) Contribution of intraoperative neuromonitoring to the identification of the external branch of superior laryngeal nerve. Turk J Surg. 33(3): 169-174. [Ref.]
- Wang K, Cai H, Kong, et al. (2017) The identification, preservation and classification of the external branch of the superior laryngeal nerve in thyroidectomy. World J Surg. 41(10): 2521-2529. [PubMed.]
- Aleksova L, Ali MM, Chakarov DI, Yozgyur ZM. (2017) Identification of the external branch of the superior laryngeal nerve during thyroid surgery. Folia Med. 60(1): 154-157. [PubMed.]
- Gurleyik E, Gurleyik G. (2017) Intraoperative monitoring of external branch of the superior laryngeal nerve. functional identification, motor integrity, and its role on vocal cord function. Journal of Inv Surg. 31(6): 509-514. [PubMed.]
- Zhang GL, Zhang GL, Ym L, et al. (2021) Endoscopic thyroidectomy versus traditional open thyroidectomy for identification of the external branch of the superior laryngeal nerve. Surgical Endoscopy. 35: 2831-2837. [PubMed.]
- Gurleyik E, Gurleyik G. (2021) Improving classification of the external branch of the superior laryngeal nerve with neural monitoring. a research appraisal and narrative review. Acta Chirurgica Belgica. 122(3). [Ref.]
- Cheruiyot I, et al. (2018) Surgical anatomy of the external branch of the superior laryngeal nerve. a systematic review and meta-analysis. Langenbeck’s Archives of Surgery. 403: 811-823. [PubMed.]