>Corresponding Author : Melis Palamar
>Article Type : Mini Review Article
>Volume : 3 | Issue : 1
>Received Date : 06 Dec, 2023
>Accepted Date : 18 Dec, 2023
>Published Date : 22 Dec, 2023
>DOI : https://doi.org/10.54289/JORVC2300101
>Citation : Tas MD, Baris ME, Guven S and Palamar M. (2023) Evaluation of Self-Competence in Eye-Drop Instillation in Healthy Young Adults. J Ophthalmic Res Vis Care 3(1): doi https://doi.org/10.54289/JORVC2300101
>Copyright : © 2023 Tas MD, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Mini Review Article | Open Access | Full Text
Ege University, Department of Ophthalmology, Izmir, Türkiye
*Corresponding author: Melis Palamar, Ege University, Department of Ophthalmology, Izmir, Türkiye
Abstract
Aim: To evaluate the ability of self-instillation of eye drops in healthy adults.
Methods: Participants who are older than 18 years old with no ocular or systemic pathologies were included in the study. All subjects underwent a complete ophthalmological evaluation including best corrected visual acuity (BCVA), intraocular pressure measurement, anterior and posterior segment examinations. Participants were given a 5 ml bottle of sodium hyaluronate 0.15% (Dryex, Abdi Ibrahim, Turkiye) and were instructed to install one drop to each eye. Dominant hands of the participants were noted and eye-drop instillation was evaluated for each eye. Success was defined as putting one drop on the ocular surface, not touching the bottle tip to surrounding tissues nor to the ocular surface, and not putting more than one drop.
Results: A total of 50 participants, 27 (54%) female and 23 (46%) male were included in the study. The mean age was 28.0±8.1 (18-40) years, and the mean best corrected visual acuity (Snellen) was 1.0 (all participants had 20/20 visual acuity). The number of participants who managed to instill the eye-drop to both eyes successfully was 13 (26%). When both eyes were encountered, the rate of he successful ability to instill at least 1 drop was 62%, bottle tip touch was 39%, and more than one drop flow was 27%).
Conclusion: The success rate of self-using of eye drops is lower than expected (26%) in healthy young adults, and patient education on eye-drop instillation might be a necessity for every patient.
Keywords: Compliance; Dry Eye; Eye Drop Instillation; Glaucoma; Patient Education
Abbreviations: BCVA: Best Corrected Visual Acuity
Introduction
Topical treatment is an essential part of ophthalmology practice and most of the patients have to apply the medications by themselves. Visual and physical disabilities or lack of knowledge on how to use eye drops properly might cause inappropriate instillation, resulting with treatment failure [1,2]. Many ophthalmologists prescribe eye drops without explaining the correct instillation technique to patients under busy working conditions [3].
The correct eye drop instillation technique includes the steps of one drop into the pocket formed by gently pulling down the lower eyelid and not touching the bottle to the eye.
Missing the eye and contacting the ocular surface with the bottle are the most common mistakes [3]. These mistakes can cause treatment failure causing physicians to think that the drug is ineffective as well as various complications including epithelial problems, refractory infections, etc. Correct instillation of the eye drops is especially important in patients who require long-term topical treatment such as glaucoma and dry eye.
Instillation success rates in glaucoma patients and geriatric groups have been investigated inseveral previous studies [4]. Although instillation failure is thought to be higher in these groups due to poor visual acuity and reduced manual skills, it might also be detected in young and healthy individuals. This study aimed to evaluate the performance of self-instillation of eye drops among healthy young adults.
Materials and Methods
This prospective clinical study was conducted in Ege University Hospital, Ophthalmology Department between January and April 2023 and was approved by the Ege University Ethics Committee and by the Turkish Medicines and Medical Devices Agency. Written informed consent was obtained from all participants and the study was conducted by the principles of the Declaration of Helsinki.
Patients who applied for routine eye examination between the ages of 18-40 and did not have any ophthalmological or musculoskeletal pathologies, were not using any eye drops were included. All had a visual acuity of 1.0 in both eyes and had at least finished high school education. Physicians, nurses, health technicians, and medical school students who might previously be taught to instill eye drops were excluded. Moreover, patients with any musculoskeletal pathologies causing limitation of movement of the hands, arms, or neck, those with high refractive errors (±3 D spherical, ±1 D cylindrical), those with presbyopia, contact lens use and patients with any acute or chronic ophthalmological pathologies were excluded from the study.
All participants underwent a complete ophthalmologic examination including best corrected visual acuity (Snellen), measurement of intraocular pressure (Goldmann applanation tonometry), slit-lamp examination of the anterior segment and posterior segments with a 90 D lens. Afterwards, their performance of instillation of eye drops to their own eyes was evaluated.
Without any instruction or training by the researchers, the participants were given a 5 ml bottle containing sterile 0.15% sodium hyaluronate (Dryex, Abdi Ibrahim, Turkiye) and were instructed to instill one drop to each eye using their dominant hands while sitting in an up right chair. The entry of the drop into the eye (ocular surface and/or conjunctival fornix), the contact of the bottle with the eyelids, eyelashes, and ocular surface, and the number of drops instilled were recorded. Observations were made by two researchers (MDT, MEB). If the participants were not satisfied with their first attempt, they were allowed to try once more. It was accepted as complete success, if the drop hits the ocular surface/fornix, the tip of the bottle does not contact anywhere, and a single drop drips in each try.
Statistical analysis was performed using IBM SPSS Statistics Software (IBM, Illinois, USA). The chi-square test was used when examining the relationship between categorical variables. The significance level was 0.05 while interpreting the results. It was stated that there was a significant difference in the case of p<0.05.
Results
A total of 50 participants, 27 (54%) female, and 23 (46%) male were included in the study. The mean age was 28.0±8.1 (18-40) years, and the mean best corrected visual acuity (Snellen) was 1.0 (all participants had 20/20 visual acuity). None of the patients had any systemic diseases. The dominant hand was right in 46 (92%) and the left in 4 (8%) participants.
The eye drop instillation rates of the participants and the faults that were made are shown in Table 1. When the right and left eyes were both evaluated, the rate of successful ability to instill at least 1 drop was 62%, the rate of contacting the bottle to the ocular surface or the eyelashes was 39%, and the rate of pouring more than one drop was 27%. The ability to instill at least 1 drop on the right and left ocular surfaces of the right-handed participants was 30/46 (65.2%) and 28/46 (60.8%), respectively, and there was no significant difference between the two eyes (p= 0.6). The ability to instill at least 1 drop on the right and left ocular surfaces of the4 participants whose left hands were dominant were 2/4 (50%) on the right and 2/4 (50%) on the left, respectively.
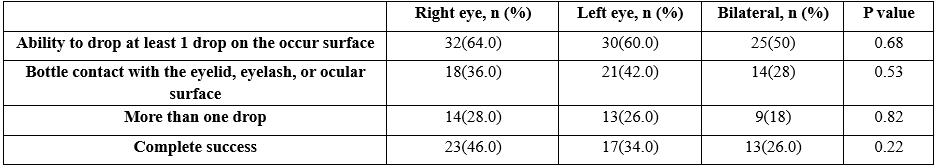
Table 1: The abilities of the participants eye drops instillation in the right and left eyes.
The number of participants who managed to instill the eye-drop to both eyes successfully according to our complete success criteria was 13 (26%). While the rate of completely successful instillation in the right eye was 23 (46%), the rate of completely successful instillation in the left eye was 17 (34%), and there was no statistical difference (p=0.2).
While the rate of completely successful instillation in the right eye of the right-handed participants was 22 (47.8%), the complete success rate in the left eye of these participants was 17 (36.9%), and there was no statistically significant difference (p=0.2). In 4 left-handed participants, the rate of successful instillation of drops in both to the right and left eyes were 25%.
Discussion
In this study, the success rates of instillation of eye drops in both eyes was found to be 26% in participants without any ophthalmological or skeletal system pathologies. In a study by Tatham et al. conducted on glaucoma patients, the number of patients who could successfully instill a drop and did not have bottle contact was found to be 29.4% [2]. In the study by Henessy et al., the success rate of instillation in glaucoma patients was reported as 39% [5].
In a study evaluating real-life data, it was found that the rates of successful drop instillation were low even in patients who had been using eye drops for at least 1 month, and the most common mistake was bottle contact with the ocular surface or eyelids (40.7%) [6]. In another study, it was shown in patients with different ophthalmological pathologies that in the supine position, patients were able to instill drops more accurately [7]. While applying eye drops, patients use the bottle with their dominant hands and manipulate the eyelids with the other hands. In a study evaluating hand dominance when eye drops hit the eye, it was found that dominance was not significantly related succes of eye drop instillation [8]. Herein, hand dominance was also not a significant factor for success.
The most common mistakes made by patients include contacting the bottle with the ocular surface or eyelids and instilling more than one drop [5,9]. The contact of the bottle tip with the surface increases the risk of contamination. In the study of Teuchner et al. among glaucoma patients, bottle contact was observed at a rate of 24% [10]. Geyer et al. reported a 40% contamination rate 8 weeks or more after the bottle was opened [11]. It is also known that bottle contact may cause corneal epithelial defects, and related complications such as keratitis and recurrent epithelial defects.
Tatham et al. reported that 42.4% contacted the bottle with the ocular surface in a study of 85 patients [2]. Gupta et al. reported that the contact of the bottle to the ocular surface was 75% in a study involving 70 glaucoma patients [12]. In a study by Gomes et al., the rate of bottle contact with the ocular surface was 62%, while the rate of multiple drops was 27% [13]. In a study evaluating the success of instillation in patients with and without glaucoma, the contact of the bottle to the ocular surface was 15.3% in the group without glaucoma, while the rate of instillation of more than one drop was 8.2% in this group [14]. In the present study, the rate of contacting the tip of the bottle with at least one eye in healthy young adults was 50%, and the rate of instilling more than one drop was 36%.
Instilling more than one drop may result inadequacy of the drug during the treatment period among patients who are using social health insurance support. It is especially important for patients who need to regularly use this drug for a certain period of time. Previous studies have generally been conducted in glaucoma patients, and multiple instillation rates have been reported at rates ranging from 3 to 40% [15]. Another disadvantage of instilling multiple drops is the possibility of facing more common systemic adverse events such as cardiovascular or bronchio-alveolar problems. In addition, it increases the possibility of local dermatological side effects such as periocular skin hyperpigmentation etc [13,14].
In order to increase the success, methods such as mirror-assisted droppers, attaching a funnel to the dropper tip, designing the bottles to cover the eye and surrounding structures, or darktipped dropper methods were used [15,16]. Actually, probably the best option to increase success in patients is to educate them about how to instill eye drops [17,18].
It has been shown that patient education for using eye drops significantly increases performance [13,19]. In the study of Kan et al., the rate of instillation of eye drops in 138 glaucoma patients after training increased significantly [4]. Al Busaidi et al., however, reported no significant difference in performance between the groups that participated and did not participate in the training program in patients using glaucoma drops [20]. Patient education can also be provided with videos or educational programs showing drop instillation.
Eye drop instillation has generally been evaluated in patients with glaucoma. There are limited publications evaluating patients without ophthalmologic pathology. In a study examining the success of eye drop instillation in glaucoma patients and healthy people without glaucoma, it was reported that the success rate in the healthy group was 64.9% in participants younger than 65 years of age, while it was 39.3% in those older than 65 years. In that study, the success rate of eye drop instillation was found to be significantly lower in glaucoma patients than those without glaucoma [14]. Evaluation of non-adherence to treatment in elderly and sick individuals has been studied in previous studies in detail, however this subject is not often considered in young and healthy individuals. The correct use of eye drops is not as easy as it seems, and if it is not done correctly, it might cause problems such as increased cost and side effects, resulting with the discontinuity of treatment or ocular surface problems and eventually treatment failure.
The present study revealed that the success rate of self-using of eye drops is lower than expected in healthy young adults. Since treatment adherence directly affects the success of treatment in many ophthalmological diseases that frequently affect young people, including conjunctivitis, keratitis, dry eye, and uveitis, it is of great importance that ophthalmologists should educate all patients about how to instill the eye drops. Considering the overcrowding patients in most of the ophthalmology clinics, an education unit to direct these patients to learn how to use their medications might be beneficial.
Statements and Declarations
Financial disclosure: None
Conflict of interest: None
References
- Lampert A, Bruckner T, Haefeli WE, Seidling HM. (2019) Improving eye-drop administration skills of patients - A multicenter parallel-group cluster-randomized controlled trial. PloS One. 14(2): e0212007. [PubMed.]
- Tatham AJ, Sarodia U, Gatrad F, Awan A. (2013) Eye drop instillation technique in patients with glaucoma. Eye Lond Engl. 27(11): 1293-1298. [PubMed.]
- Sayner R, Carpenter DM, Robin AL, et al. (2016) How glaucoma patient characteristics, selfefficacy, and patient-provider communication are associated with eye drop technique. Int J Pharm Pract. 24(2): 78-85. [PubMed.]
- Kan YM, Kho BP, Kong L, Chong QX, Tiong MNJ, et al. (2022) Eye drop instillation technique among patients with glaucoma and evaluation of pharmacists’ roles in improving their technique: an exploratory study. Int J Pharm Pract. 30(6): 520-525. [PubMed.]
- Hennessy AL, Katz J, Covert D, et al. (2011) A video study of drop instillation in both glaucoma and retina patients with visual impairment. Am J Ophthalmol. 152(6): 982-988. [PubMed.]
- Mehuys E, Delaey C, Christiaens T, et al. (2020) Eye drop technique and patient-reported problems in a realworld population of eye drop users. Eye Lond Engl. 34(8): 1392-1398. [PubMed.]
- Naito T, Yoshikawa K, Namiguchi K, et al. (2018) Comparison of success rates in eye drop instillation between a sitting position and supine position. PloS One. 13(9): e0204363. [Ref.]
- Kayıkçıoğlu Ö, Erakgün T, Eğrilmez S, Akkın C. (2000) The Relationship of Hand Dominance With Eyedrop Administration. Turk J Ophthalmol 30: 645-648. [Ref.]
- Ramalho CM, Ribeiro LN, Olivieri LS, Silva JA da, Vale TC, et al. (2007) [Socioeconomic profile of individuals presenting with glaucoma in the service of ophthalmology of the University Hospital of the Federal University of Juiz de Fora - Minas Gerais - Brazil]. Arq Bras Oftalmol. 70(5): 809-813. [PubMed.]
- Teuchner B, Wagner J, Bechrakis NE, Orth-Höller D, Nagl M. (2015) Microbial contamination of glaucoma eyedrops used by patients compared with ocular medications used in the hospital. Medicine (Baltimore). 94(8): e583. [Ref.]
- Geyer O, Bottone EJ, Podos SM, Schumer RA, Asbell PA. (1995) Microbial contamination of medications used to treat glaucoma. Br J Ophthalmol. 79(4): 376-379. [PubMed.]
- Gupta R, Patil B, Shah BM, Bali SJ, Mishra SK, et al. (2012) Evaluating eye drop instillation technique in glaucoma patients. J Glaucoma. 21(3): 189-192. [PubMed.]
- Gomes BF, Paredes AF, Madeira N, Moraes HV, Santhiago MR. (2017) Assessment of eye drop instillation technique in glaucoma patients. Arq Bras Oftalmol. 80(4): 238-241. [PubMed.]
- Naito T, Namiguchi K, Yoshikawa K, et al. (2017) Factors affecting eye drop instillation in glaucoma patients with visual field defect. PloS One. 12(10): e0185874. [Ref.]
- Strungaru MH, Peck J, Compeau EC, Trope GE, Buys YM. (2014) Mirror-hat device as a drop delivery aid: a pilot study. Can J Ophthalmol J Can Ophtalmol. 49(4): 333-338. [PubMed.]
- Brand G, Hecht I, Burgansky-Eliash Z, et al. (2021) Comparison of the Usability of Eye Drop Aids and the Conventional Bottle. J Clin Med. 10(23): 56-58. [PubMed.]
- Salyani A, Birt C. (2005) Evaluation of an eye drop guide to aid self-administration by patients experienced with topical use of glaucoma medication. Can J Ophthalmol J Can Ophtalmol. 40(2): 170-174. [PubMed.]
- Carpenter DM, Sayner R, Blalock SJ, et al. (2016) The Effect of Eye Drop Technique Education in Patients With Glaucoma. Health Commun. 31(8): 1036-1042. [Ref.]
- Liu Y, Murdoch A, Bassett K, Dharamsi S. (2013) Proficiency of eye drop instillation in postoperative cataract patients in Ghana. Clin Ophthalmol Auckl NZ. 7: 2099-2105. [PubMed.]
- Al-Busaidi A, Samek DA, Kasner O. (2016) Eye drop administration in patients attending and not attending a glaucoma education center. Oman J Ophthalmol. 9(1): 11-16. [PubMed.]