>Corresponding Author : Lim Chee Min
>Article Type : Case Report
>Volume : 2 | Issue : 1
>Received Date : 13 March, 2022
>Accepted Date : 27 March, 2022
>Published Date : 30 March, 2022
>DOI : https://doi.org/10.54289/JORVC2200103
>Citation : Min LC, Ariffin N, Hong HS, Vendargon FM. (2022) Paediatric Supraorbital Mass: A Case of Langerhans Cell Histiocytosis. J Ophthalmic Res Vis Care 2(1): doi https://doi.org/10.54289/JORVC2200103
>Copyright : © 2022 Min LC, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Case Report Article | Open Access | Full Text
Department of Ophthalmology, Hospital Sultanah Aminah Johor Bahru, Johor
*Corresponding author: Lim Chee Min, Department of Ophthalmology, Hospital Sultanah Aminah Johor Bahru, Johor
Abstract
This is a case of 2-year-old boy who presented with painless right supraorbital swelling for 2 weeks. He had history of left humerus fracture and multiple scalp swelling. Examination revealed a hard, non-tender mass over right upper eye lid with downward placement of eye globe and limitation of extraocular muscle movement upon upward gaze. Systemic examination was unremarkable. MRI brain and orbit showed avid enhancing mass arising from right orbital roof. Histopathological examination of left humerus trucut biopsy revealed focal aggregation of histiocytes with scattered eosinophils. The diagnosis of LCH was further confirmed by positive CD1a and S100 protein staining on immunohistochemical studies. He was referred to oncology department for initiation of chemotherapy. Significant improvement was seen after the first cycle of chemotherapy.
Keywords: Langerhans cell histiocytosis, supraorbital swelling
Introduction
Langerhans Cell Histiocytosis (LCH) is a spectrum of disorders characterized by an accumulation of histiocytes in various tissues [1]. Any organ or system of the human body can be affected, but those more frequently involved are the skeleton (80% of cases), the skin (33%), and the pituitary (25%) [2]. They may manifest as unisystem (Unifocal or multifocal) or multisystem disease, predominantly in children [3,4].
Objective: To report a case of LCH presented with orbital manifestation.
Case description:
A two-year-old boy presented with acute painless right eye swelling of 2 weeks duration. He had no fever and was active. 3 months earlier, he had left humerus fracture requiring bone biopsy in view of persistent swelling at the fracture site. The bone biopsy was negative for cancer and his left humerus swelling gradually resolved. In the same year, he also had history of multiple scalp swellings which were spontaneously resolved.
On examination, there was a firm, well-defined, non-tender right supraorbital mass measuring 3×2cm causing downward displacement of the globe and up gaze limitation (Figure 1). The overlying skin was not inflamed and there was no eyelid infiltration. Visual acuity and other ocular findings were normal. Systemic examination was unremarkable. There was no mass on the scalp or left humerus. Patient was initially treated as right preseptal cellulitis by paediatric team. However, there was no improvement after receiving intravenous antibiotic for 1 week.
Full blood counts were normal and full blood picture showed no blast cell. MRI brain and orbit showed an enhancing mass arising from right orbital roof (Figure 3 & 4) with differential diagnoses of Langerhans Cell Histiocytosis (LCH), lymphoma and rhabdomyosarcoma. We manage to revise the histopathological examination (HPE) of previous left humerus trucut bone biopsy in which focal aggregation of histiocytes with scattered eosinophils was seen. Possibility of LCH was further tested on the same sample by using CD1a and S100 protein staining on immunohistochemical studies and the results were positives for both.
Both radiological and HPE results confirmed the diagnosis of LCH. He was referred to Oncology Department for initiation of chemotherapy. Significant improvement was seen even after the first cycle of chemotherapy (Figure 2).
Discussion:
The clinical differential diagnoses that need to be considered in this type of case includes orbital cellulitis, acute dacryocystitis, ruptured dermoid cyst, hematoma, inflammatory pseudotumor, pilomatrixoma, leukaemia, sarcoma, metastatic neuroblastoma, and rhabdomyosarcoma [4].
Langerhans cell histiocytosis (LCH) is a heterogeneous disease. It is characterized by accumulation of dendritic cells with features similar to epidermal Langerhans cells in various organs [2]. Orbital involvement is found in 20% of LCH patients [1]. Orbital involvement of LCH is characterised by osteolytic lesions with sclerotic margins, commonly involving the zygomatico-frontal suture, [3] as seen in our patient.

Figure 1: Photograph showing right supraorbital swelling with downward displacement of globe

Figure 2: Photograph showing reduction of right supraorbital swelling after first cycle chemotherapy
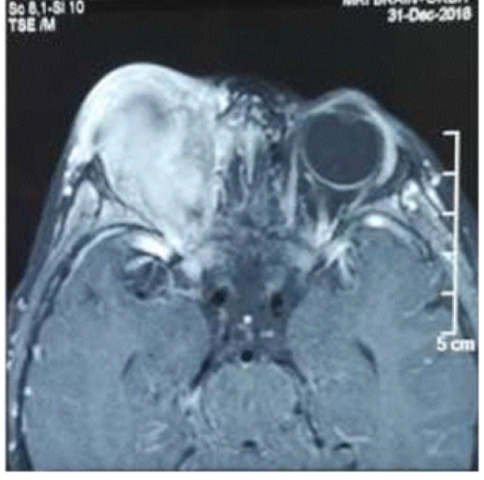
Figure 3: Axial view of MRI orbit showing enhancing mass from right orbital roof
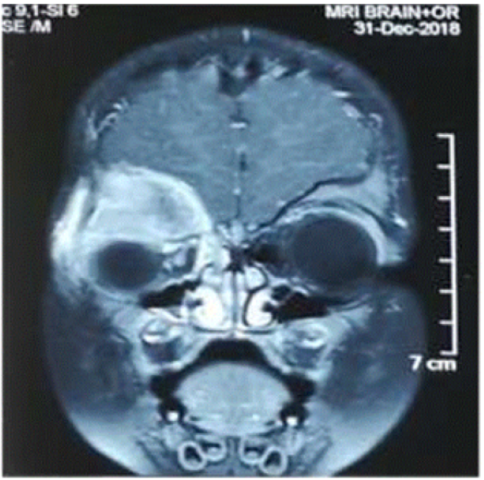
Figure 4: Coronal view of MRI orbit showing enhancing mass from right orbital roof with adjacent bony erosion
There are three clinico-pathological entities in LCH: i) acute disseminated LCH, ii) unifocal and multifocal unisystem LCH and iii) multisystem LCH [3]. Systemic evaluation is essential in ruling out multisystem disease [3]. The distinction between single and multisystem disease is very important as management and prognosis differs.3 Our patient fell into multifocal unisystem LCH in view of involvement of skull, orbit and humerus.
The treatment of LCH can be close observations, surgical curettage, local injection of corticosteroids, chemotherapy, bone marrow transplantation and antibody therapy [3]. The choice of therapeutic regime depends ultimately on disease severity and number of systems involved [1].
According to Histiocytosis Society guidance (2009) a combination of prednisolone and vinblastine has been proven to be effective, therefore becomes the standard initial therapy for all patients who receive systemic therapy [5]. Indications for systemic therapy in LCH are i) single system LCH with central nervous system risk lesions ii) single system LCH with multiple bone lesions iii) single system LCH with special site lesions (vertebral lesions with soft tissue extension) iv) multisystem LCH5. Our patient received combination of prednisolone and vinblastine in view of multiple bony lesions involved.
Conclusion:
LCH is a rare multisystemic disorder in which patient can present with isolated orbital manifestation. A high index of suspicion is required to establish a diagnosis of LCH when the disease is focal. Histopathological study is important in confirming diagnosis of LCH. Early diagnosis of LCH is possible with careful clinical assessment and radiologic imaging to aid for early treatment.
References
- Das JK, Soibam R, Tiwary BK, Magdalene D, Paul SB, et al. (2009) Orbital manifestations of Langerhans. Cell Histiocytosis: A report of three cases. Oman J Ophthalmol. 2(3): 137-140. [PubMed.]
- Haupt R, Minkov M, Astigarraga I, et al. (2013) Euro Histio Network. Langerhans Cell Histiocytosis (LCH): Guidelines for Diagnosis.Clinical Work-Up and Treatment for Patients till the Age of 18 Years. Pediatric Blood Cancer. 60(2): 175-184. [PubMed.]
- Shetty SB, Mehta C. (2001) Langerhans cell histiocytosis of the orbit. Indian J Ophthalmol. 49:(4) 267. [Ref.]
- Rajendran P, Kok WK, Hussein A, Subramaniam S, Musa AT, et al. (2017) Orbital Manifestation of Langerhans Cell Histiocytosis in a Child -A Diagnostic Dilemma. AperitoJ Ophthalmol. 3: 1. [Ref.]
- Munir A, Leech N, Windebank KP, et al. (2012) Langerhans cell histiocytosis: a multisystem disorder. R Coll Physicians Edinb 42: 311-313. [Ref.]