>Corresponding Author : Amphayvan Homsavath
>Article Type : Mini Review Article
>Volume : 5 | Issue : 2
>Received Date : 14 August, 2025
>Accepted Date : 26 August, 2025
>Published Date : 30 August, 2025
>DOI : https://doi.org/10.54289/JDOE2500108
>Citation : Homsavath A, Eugenio BA, Vannapho K, Rajpho V, and Inthakhoun V. (2025) The Factors Effecting to Dental Service and Oral Health Status Related to Quality of Life Among Older Adults Aged 65-74 Years in Hadxayfong District, Vientiane Capital, Lao P.D.R. J Dent Oral Epidemiol 5(2): doi https://doi.org/10.54289/JDOE2500108
>Copyright : © 2025 Homsavath A, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Mini Review Article | Open Access | Full Text
1Faculty of Dentistry, University of Health Sciences, Vientiane, Lao P.D.R
2Department of Epidemiology, College of Global Public Health, New York University, New York, USA
3103 Military Hospital, Vientiane, Lao P.D.R
4Faculty of Medicine, University of Health Sciences, Vientiane, Lao P.D.R
5Faculty of Dentistry, University of Health Sciences, Vientiane, Lao P.D.R
*Corresponding author: Amphayvan Homsavath, Faculty of Dentistry, University of Health Sciences, Vientiane, Lao P.D.R.
Abstract
The objective of this study was to measure the effects of oral health status on the quality of life, and to describe utilization of dental care services among senior adults aged 65 to 74 years in Hadxaifong District, Vientiane Capital, Lao P.D.R. A cross sectional study was designed and a total of 232 older adults aged 65–74 years were selected by convenience sampling. Participants responded to questionnaire and were clinically examined for dental caries, periodontal status, and tooth loss using standard WHO criteria. The prevalence of dental caries was 78 percent with mean number of decayed, missing, and filled teeth (DMFT) score 15 4. The prevalence of periodontal pockets (1 or more teeth with 4 mm or more of probing depths) was 95 percent. Sixty-six percent of participants had more severe periodontal pockets (1 or more teeth with 6 mm or more). On average, the mean number of missing teeth was 13, and no filled teeth, suggesting that tooth extraction is the only type of dental care received by senior adults in Hadxaifong District. In agreement with these clinical findings, the most common impacts on quality of life were eating (100%), smiling (52%), and speaking (48%). Seventy-five percent of participants reported having at least one dental visit in their lifetime. The main reason for not having a dental visit was perceived absence of dental problems (41%), never live close to the dentist (30%) and followed by cost (29%). Thus, income, fear and having no time were the barriers to access of oral health care in Hadxaifong District. Oral health care planning needs to emphasize more both prevention and promotion to adults and elderly in Hadxaifong District, Vientiane Capital, Lao P.D.R.
Keywords: Dental Service, Caries, Periodontal Disease and OIDP
Abbreviations: Lao PDR: Lao People’s Democratic Republic
Background and problem statement
Lao People’s Democratic Republic (Lao PDR) is located in a landlocked area surrounded by China, Vietnam, Cambodia, Thailand and Myanmar. According to the National Statistics Center, the population is estimated at 7,062,214 [1]. Approximately 68 percent of the Lao population lives in rural areas, primarily engaged in agricultural work [1]. The elderly population in Lao PDR, aged 65-74 years, totaled 162,900 people in 2015, and this population is expected to reach 198,100 by 2020 [2].
Hadxaifong District, located in the Vientiane Capital, Lao PDR, has an area of 258 km2 and a population of approximately of 99,757 people. Within the district, there are 2,712 people aged 65-74 years (males=1297 and females=1415) [3].
The world’s population reached nearly 7.6 billion in mid-2017. The world has added one billion people since 2005 and two billion since 1993. The United Nations reports an increase in the elderly population around the world in the last century–13 percent were aged 60 years or more, and two percent were aged 80 years or more. In 2017, there were approximately 962 million people aged 60 years and older worldwide. It is estimated that by 2050, the elderly populations will have reached 2.1 billion [4].
The growing number of older adults has become a public health concern in many countries because an aging population places considerable demands on social and healthcare services. Oral health is essential to general health and well-being of older adults, but many elderly people face significant problems and obstacles in getting dental care, such as financial barriers [5]. Oral diseases in older adults have a negative impact on their daily quality of life. For example, tooth loss may impact the ability to chew, affect the selection of certain foods and impact on nutritional intake [6]. In a review study published in 2017, Almeida and coworkers reported on the association of sociodemographic variables and utilization among older adults of health care services. Higher income and education have been associated with the use and access to medical appointments. The same association has been observed in dental visits in all countries [7].
Different terms have been used to label those who are 65 years and older, including “third age,” “elderly,” “seniors,” “retired adults,” and more recently “older adults.” The latter will be term used in this research. This study was measuring current oral disease levels, their impact on daily living, and barriers to treatment services among older adults in Hadsaifong District. This information will be a benefit of oral health promoting the prevention strategies on oral problem among elderly and quality of life.
Materials and Methods
Study Design
The study was a cross-sectional study. The survey was conducted during the period 2021 at Hadxaifong District, Vientiane Capital, Lao P.D.R. The study population was older adults and seniors aged 65-74 years. Sample size was calculated using Confidence coefficient from the threshold for significance (1-α) = 95% and proportion of population of caries diseases 84% or 0.84 [8]. Number of population study was 229 individuals in six villages. Multistage cluster was followed. Elderly with systemic health conditions such as cancer, stroke was excluded.
Operational Definitions and Measuring Tools
Self-reported variables were collected by a face-to-face interview. The questionnaire was designed to obtain self-reported information regarding socio-geographic indicators, oral health status, access and utilization of dental services, having dentures, and oral health impacts on daily living. Most questions were derived from instruments used in other studies. The OIDP questionnaire for older adults was used to measure impacts on daily living [9]. Scores were obtained for each of performance impact by multiplying the frequency (0-5 points) and severity score (0-5 points) for each performance. The overall OIDP score was derived from the sum of all performance scores and divided by the maximum possible score (5 frequency x 5 severity scores x 10 performances) and multiplied by 100 to obtain a percentage. In addition to the OIDP score [10] and refers to the number of OIDP performances with impacts affecting a respondent’s quality of life over the past six months.
Normative Variables
All normative results were recorded in a modified WHO data entry form. Dental caries was measured at the tooth level using the decayed, missing, and filled teeth index (DMFT) following the World Health Organization detection criteria and process [11].
Periodontal status was measured using the Community Periodontal Index (CPI) following the WHO Health Organization detection criteria and process. Each tooth, except third molars, was assessed for periodontal pockets in six sites. The worst CPI value for all six sites was used to categorize the tooth.
Data Collection
Data collection was conducted with logistical support and recommendations from the head of the village, who provided input regarding a physical study location, such as at the temple or the village office. In case participants were unable to come to the survey site, the research team conducted the examination and interview in their homes. Data collection was divided into two phases: in the first phase, each participant was interviewed to complete the questionnaire. Completing the questionnaire took approximately 15 minutes. The clinical examination followed the interview and took approximately 5-10 minutes.
All clinical examinations were performed by the examiner with the help of a recorder The examiner trained the recorder to use a modified WHO recording form. For the clinical examination, participants were seated on a chair. In addition, a head lamp (flashlight) was used to help with intraoral illumination along with a flat mouth mirror and a WHO periodontal probe. After completing the examination, the examiner and recorder verified that the coding was complete. Completed forms were collected and kept in a secure place to prevent loss or damage until data entry and analyses were completed
Data analysis
All variables were analyzed at the univariate and bivariate levels. Chi-square statistics and ANOVA was used to test for statistical differences between continuous (scale) and categorical variables.
Results
The total sample size was 232. By design, an equal number of males and females were selected. The sample included 114 individuals (49%) aged 65 to 69 years and 118 individuals (51%) aged 70 to 74 years (Table 1). The overall mean age was 68.9 years. The mean age for males was 68.9 (sd=3.1) and for females it was 69.0 (sd=3.1). Fifty-five percent of all participants reported being married, most participants (75%) completed primary and secondary school and 15 percent completed secondary school. Twenty-four percent never attended school, only 1% of elderly completed University. 57% unemployed, 22% was farmer. Most participants (52%) reported a monthly family income of 1.000.001-3.000.000 Kip, with little variation by age group. Monthly family incomes less than 1.000.000 per month were more common in the oldest than in the youngest age groups (42% and 23%, respectively). Only two percent had a monthly family income greater than 5.000.000 Kip.
Access dental service
Most participants reported at least one lifetime visit to a dentist (75%). A significantly higher percentage of participants in the 70-74 years age group (82%) than in the 65-69 years age group (67%) reported at least one lifetime visit. Participants who reported no lifetime dental visit said they never had dental problems (41%). Other reasons for never visiting a dentist included never living close to a dentist (30%), seeing a traditional healer instead (24%) and going to the emergency room for dental problems (5%). The distribution of reasons for never having a dental visit by age group was statistically significant (chi-square=8.143, df=3, p=0.043).
Most participants reported that they had needed dental treatment because of pain or another problem (64%). Among those participants who reported having tooth or mouth pain in the previous 12 months, most participants took medicine from a pharmacy (41%), 45% among those in the 70-74 years age group and 37% in the 65-69 years age group. Thirty-three percent of participants went to a dentist’s office; 35% among those 65-69 years old and 32% among those 70-74 years old. Twenty-one percent of those reporting dental pain in the previous 12 months did not take any action.
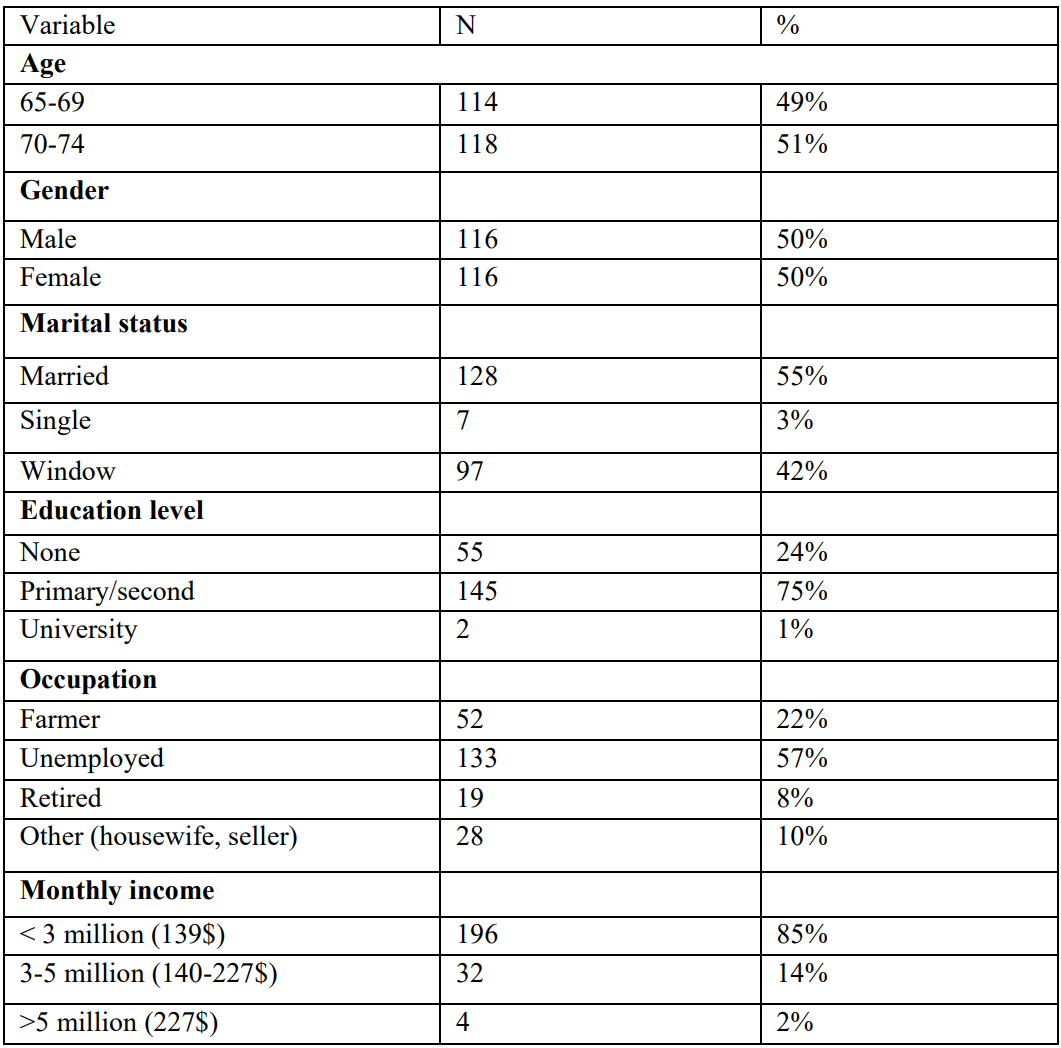
Table 1: General information of elderly in Hadxayfong District, Vientiane Capital

Table 2: history of Access dental service distribution by age group among elderly
Oral Health Status
Twelve participants (5%) had 28 teeth present at examination regardless of disease status, while nine (4%) were edentulous. The prevalence of dental caries (DMFT>0) was 100%. The overall prevalence of untreated decay (DT>0) was 78%, 56% in the 65-69 age group and 44% in the 70-74 years age group. The prevalence of untreated decay was 74% in males and 81% in females. The mean DMFT was 15.35 teeth and includes 12.68 missing, and 2.63 decayed teeth. The mean number of filled teeth was only 0.056.
Regarding clinical measures, those who ever had a dental visit had fewer number of teeth, greater number of missing teeth, higher prevalence of periodontal pockets and bleeding on probing, and higher proportion of tooth pain than those never having a dental visit (Table 3).
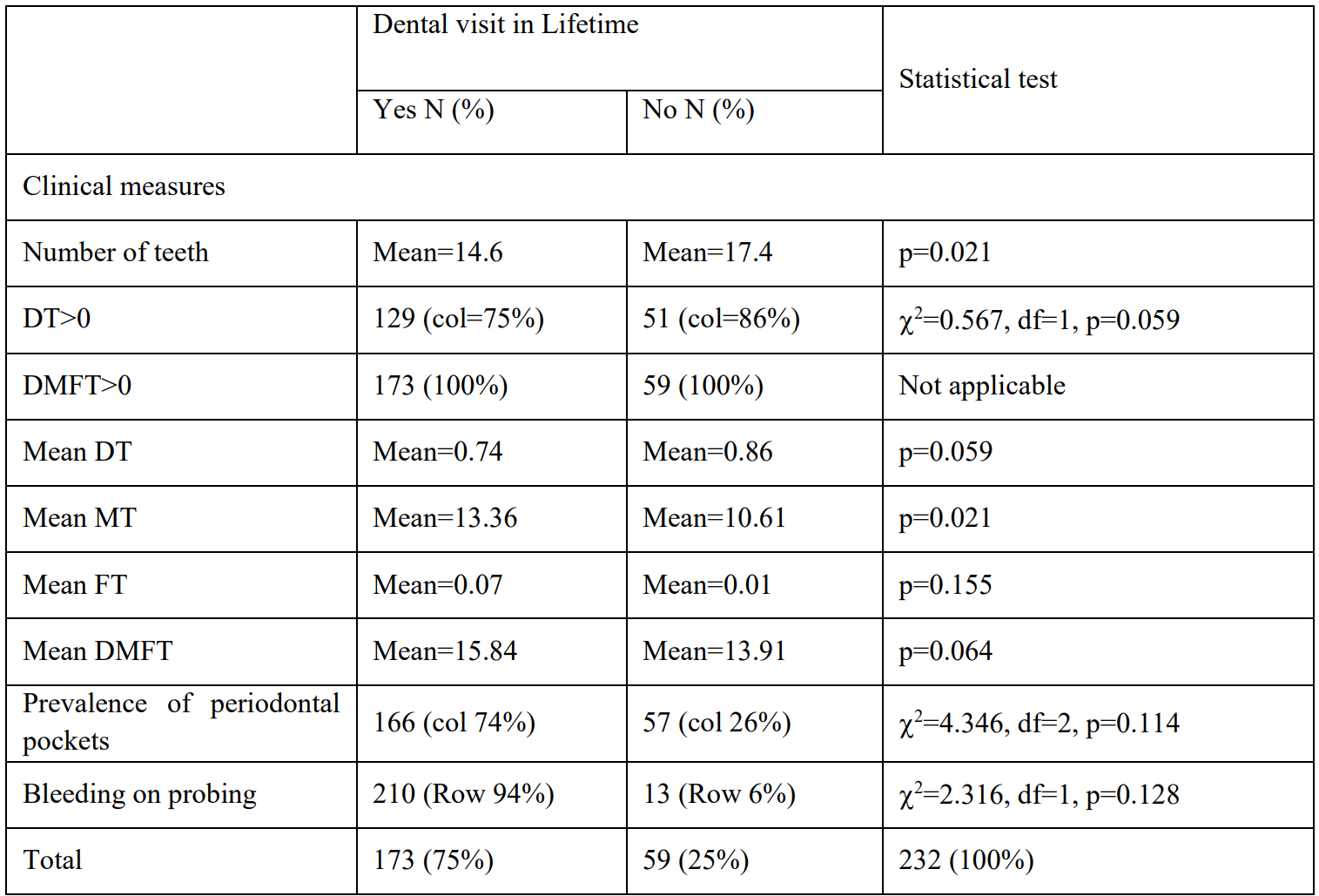
Table 3: Clinical measures of dental caries and periodontal status, comparing those with and without a lifetime dental visit
OIDP (Oral Impact in Daily Performance
Among the 155 participants reporting at least one impact in daily activity, the most common impacts were eating (100%), followed by smiling (52%), and speaking (48%). Less frequent impacts included doing work and enjoying social contact (25%). None of the participants had impacts on cleaning teeth, home activities, sleeping or relaxing. One participant reported impacts on emotions. The overall mean OIDP score was 9.76 (Table 4). The mean OIDP score was statistically higher in the older age group (p=0.004). There were no statistically significant differences by sex in the overall OIDP score. The higher OIDP score among older participants was an effect of statistically higher scores for speaking and doing work.
Discussion
Dental caries the mean DMFT score in the present study was 15.36 (DT=2.63, MT=12.67, FT=0.06). These values were very similar to those reported by Ploysangnam [12] DMFT was 16.9 (DT=2.6, MT=13.2, FT=1.0) in a Thai population. In both studies, the greatest contributor to the DMFT was missing teeth. A survey of 140 older adults, aged 60 years and older, in Luanprabang province Lao P.D.R, [13] reported a similar result (mean DMFT =15.1 teeth, DT=5.0, MT=10.1, FT=0.0). However, a study in Vientiane [8] on 252 older adults, aged 60 years and older reported lower DMFT scores (7.7 teeth, DT=3.1, MT=4.5, FT=0.0).
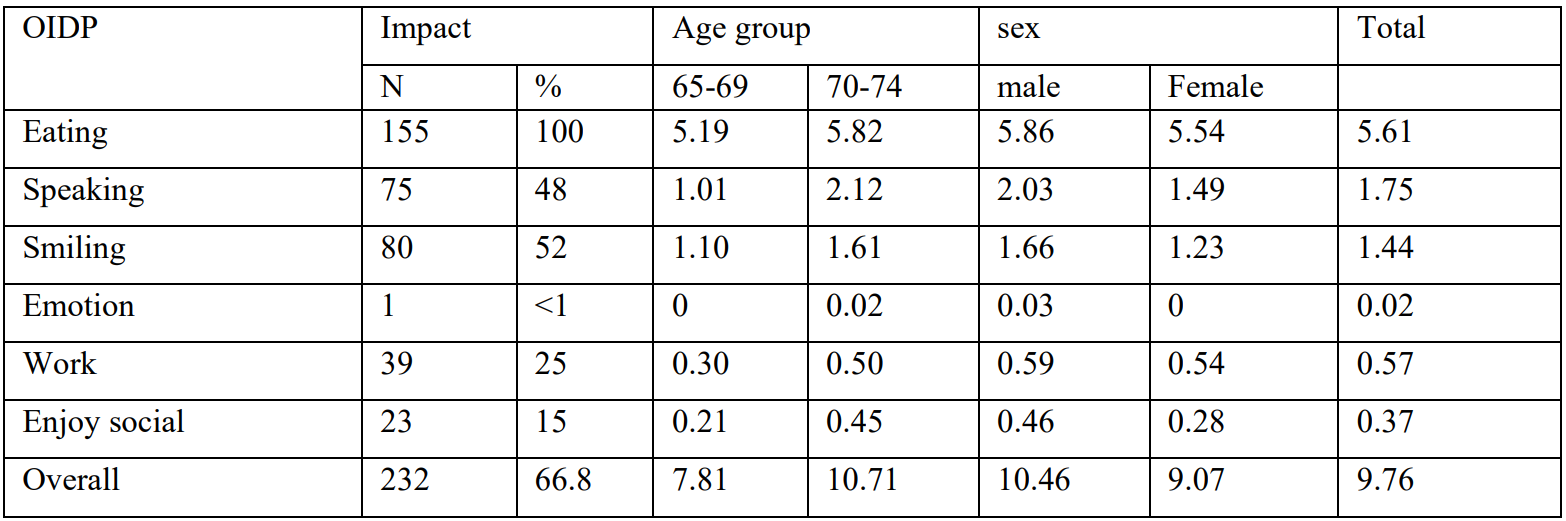
Table 4: the frequency and mean score of Oral Impact in Daily Performance among elderly distribution by age and sex.
*Represents t-test with p-values less than 0.05.
Missing teeth the average person in the study had 13 missing teeth and extraction is the only type of care received, Also, periodontal diseases lead to tooth loss, missing teeth affects the quality of life of the elderly especially in terms of chewing, pronunciation and smiling. When a lot of teeth are lost, the quality of life is poor compared to studies in Thailand had 13.2 missing teeth [12] and in Laos had 10.1 missing teeth [13]. There is still a lot of tooth loss. Consistent to São Paulo, Brazil the two main risk factors for tooth loss are dental caries and seeking dental service by pain [14]. As it is the case for dental caries, periodontal diseases have strong social determinants; thus, people with lower income, lesser education, or inadequate access to care are more likely to loss teeth [15].
In the present study was 86% of participants with a previous dental visit received only extraction for treatment. Edentulism is when all teeth have been extracted. In some countries tooth extraction and dentures becomes a treatment of choice for low-income individuals because they are cheaper alternatives than other dental treatment [16].
When dental caries remains untreated can lead to pain, infection and eventually tooth loss. Therefore, tooth loss increases with age affecting older adults around the world [17]. Caries remains a major oral health problem among the elderly for various reasons: the increase in treatment and maintenance of teeth rather than their extraction (Gil-Montoya et al, 2015).
Periodontal status in the present study was 95% of participants had at least one periodontal pocket of 4 mm or more and 66% of participants had at least one periodontal pocket of 6 mm or more. These results are similar to the study in Luangprabang (Somsanith, 2009) where 94% of those studies had CPI>0. And in 2008, Chanthamalinh reported almost 90 percent (CPI>0) among 252 older adults aged 60 years and older living in Vientiane [18].
Periodontal status in the present study CPI>0 was 95% measure each tooth. Study in Luangprabang CPI>0 was 94% and in Vientiane CPI>0 was 90% they are measure by sextant.In this study Forty-six participants (20%) reported having dentures (either partial or total prostheses). Of these, 17 (7%) were for upper teeth, seven (3%) for lower teeth, and 22 (10%) for both.
The Oral Impact on Daily Performance (OIDP) is one of the most commonly used oral health related quality of life instruments globally. It measures the impact and extent to which the ability to perform regular physical, psychological and social activities is compromised due to poor oral health [19]. In this study the most common impacts were eating (100%), followed by smiling (52%) and speaking (48%). The oral impact on daily performances problem was severe when compared to the survey in 2017 study investigated oral health status and OIDP among an institutionalized older adult (aged 60-86 years) in seven provinces in the Northeastern Region of Thailand with reported impacts affecting eating (52%), speaking (51%). [20] and Korean study using the Oral Impact on Daily Performances (OIDP) instrument among 687 older adults 65 years and older with reported impacts affecting eating (48 %), speaking (25 %) [21].
Barriers in the present study, cost, fear, and having no time were major barriers for the utilization of dental services. In addition, 95% of participants reported paying out-of-pocket or used family funds to pay for treatment. Regarding the treatment received extraction was the most common treatment, consistent the Bommireddy report in India. Self-reported barriers for not seeking dental treatment included fear, no time, no access, expensive, lack of awareness and lack of importance of dental care [22] and Data from the U.S. National Health Interview Survey indicated that in 2010, of those over the age of 65 had a dental visit in the past year. The major perceived barriers to dental care were cost/lack of dental insurance, fear/mistrust of the dentist, and transportation problems [23].
Barriers also affect access to preventive interventions by these barriers because is a less common practice in the rural areas and among older people. In particular, this practice is less frequent in low-income countries; in contrast, traditional oral self-care is prevalent in several countries of Africa and Asia. While fluoridated toothpaste is widely used in developed countries, it is extremely infrequent in most developing countries. Oral health services are available in developed countries; however, the use of such services is low among the older people. Lack of financial support from government and/or lack of third-party payment systems render oral health services unaffordable to them [17]. It has been widely accepted that dental care utilization is low among older people, particularly among the socio-economically disadvantaged population [15].
Difficulties, Strengths, and Limitations
The main limitation of this study is that participants were recruited from one geographical location of Lao so findings may not be representative of the entire Lao elderly. In addition, despite using some random selection in each step, the sample should be considered a convenient sample of senior adults in Hadxaifong.
The major strength of this study is that it is the first to document potential drivers of dental care utilization among elders. Each country has varied healthcare policy system and needs of older adults are heterogeneous; hence it is not easy to compare findings with other countries. However, the findings of this study will serve as a baseline for future studies in Laos.
Conclusion
The findings of the present study indicate that elders in Hadxaifong have limited access to dental care and the type or dental care received is limited almost exclusively to dental extractions. As consequence, tooth loss and edentulism are followed, which limited the quality of life of this population. The barriers and facilitators as well as the health and social effects are accrued over the life course and represent the type and quality of services offered to this population. Potential solutions are not only providing some level of optimal care for senior adults but in preventing future cohorts reaching the same level of sequelae. Senior adults need adequate information about the resources available in the community and reducing barriers to receive appropriate care, including maintaining and replacing dentures. Decision makers should design effective and affordable oral health strategies integrated into general health programmes for better oral health of the elders and the oral health care planning older adults in Hadxaifong District Vientiane Capital Lao P.D.R need to emphasize more both prevalence and promotion more. Tooth loss amongst the elderly in Hadxaifong District should be a concern in the situation where the elderly has a trend to live longer. To manage tooth loss problems, prevention and treatment of dental caries and periodontal disease were needed. Effective oral health education and regular dental checkups should be emphasized. They are not going for prevention. That is a public health challenge in hadxaifong district for education in elderly to prevention or early intervention.
References
- UNDP-United Nations Development Programme. 2019. [Ref.]
- Bounpheng S. The health care for elderly population in Lao PDR. 2007. [PubMed.]
- National Statistics Center, Planning and investment Committee. Report on the population survey in Hadxaifong District. 2015. [PubMed.]
- United Nations World Population Prospects. 2017. [PubMed.]
- Dolan TA., Atchison K., Huynh TN. Access to Dental Care Among Older Adults in the United States. J Dent Educ. 2005;69(9):961–974. [PubMed.]
- Griffin SO., Jones JA., Brunson D., Griffin PM., Bailey WD. Burden of oral disease among older adults and implications for public health priorities. Am J Public Health. 2012;102(3):411–418. [PubMed] [PubMed.]
- Almeida APSC., Nunes BP., Duro SMS., Facchini LA. Socioeconomic determinants of access to health services among older adults. a systematic review. Rev Saude Publica. 2017;51:50. [PubMed.]
- Chanthamalinh V., Duangjai Lexomboon. The oral health of elderly in Vientiane Capital, Lao PDR. 2008. [Ref.]
- Eric J., Stancic I., Tihacek L. Validity and reliability of the Oral Impacts on Daily Performance (OIDP) scale in the elderly population of Bosnia and Herzevina. Gerodontology. 2012;29(2):e902–8. [PubMed.]
- World Health Organization. Oral Health Surveys Basic Method. 5th edition. Geneva, World Health Organization. 2013. [Ref.]
- Ploysangngam P., Subhakorn S., Pongnarisorn N., Jaturanon S., Chaisupamongkollarp S. Oral health status in the elderly priests in Bangkok. J Med Assoc Thai. 2008;91:Suppl 1:S30-6. [PubMed.]
- Somsanith N. The oral health status of elderly population in Luangprabang Provice, Lao PDR. 2009. [Ref.]
- Manoelito Ferreira Silva Junior., Marília Jesus Batista., Maria da Luz Rosário de Sousa. Risk factors for tooth loss in adults: A population-based prospective cohort study. Plos One. 2019;22;14(7):e 0219240. [PubMed.]
- Petersen PE., Yamamoto T. Improving the oral health of older people: the approach of the WHO global oral health Programme. Community Dent Oral Epidemiol. 2005;33(2):81–92. [PubMed.]
- Slade GD., Akinkugbe AA., Sander AE. Projections of U S. edentulism prevalence following 5 decades of decline. J Dent Res. 2014;93(10):959–965. [PubMed.]
- Petersen PE., Kandelman D., Arpin S., Ogawa H. Global oral health of older people--call for public health action. Community Dent Health. 2010;27(Suppl 2):257–267. [PubMed.]
- Gil-Montoya JA., de Mello AL., Barrios R., Gonzalez-Moles MA., Bravo M. Oral health in the elderly patient and its impact on general well-being: a nonsystematic review. Clin Interv Aging. 2015;10:461–467. [PubMed.]
- Uttara Amilani., Prasanna Jayasekara., Irosha R. Perera., Hannah E. Carter., Sameera Senanayake & Sanjeewa Kularatna. Oral impact on daily performance (OIDP) scale for use in Sri Lankan adolescents: a cross-sectional modification and validation study. BMC Oral Health. 2020;16(20). [PubMed.]
- Sombateyotha K., Mahaweerawat U. Oral health status and oral impact on daily performance in elderly in northeastern region Thailand. European Journal of Sustainable Development. 2017;6(2):240–244. [PubMed.]
- Jung SH., Ryu JI., Tsakos G., Sheiham A. A Korean version of the Oral Impacts on Daily Performances (OIDP) scale in elderly populations: validity, reliability and prevalence. Health Qual Life Outcomes. 2008;6:17. [PubMed.]
- Bommireddy VS., Koka KM., Pachava S., Sanikommu S., Ravoori S., Chandu VC. Dental service utilization: patterns and barriers among rural elderly in Guntur District., Andhra Pradesh. J Clin Diagn Res. 2016;10(3):ZC43–ZC47. [PubMed.]
- Davis DL., Reisine S., Barriers to dental care for older minority adults. Spec Care Dentist. 2015;35(4): 182–189. [PubMed.]