>Corresponding Author : Andrew S Ryser
>Article Type : Research Article
>Volume : 5 | Issue : 2
>Received Date : 06 August, 2025
>Accepted Date : 18 August, 2025
>Published Date : 22 August, 2025
>DOI : https://doi.org/10.54289/JDOE2500107
>Citation : Handel SE, Ryser AS, Sabol JV, and Gandarilla N. (2025) 3D Printed Tool for Total Occlusal Convergence Analysis. J Dent Oral Epidemiol 5(2): doi https://doi.org/10.54289/JDOE2500107
>Copyright : © 2025 Handel SE, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Research Article | Open Access | Full Text
1Assistant Program Director, Department of Prosthodontics, Army Postgraduate Dental School, Postgraduate Dental College, Uniformed Services University, Fort Eisenhower, GA, USA
2Chief of Prosthodontics, Comprehensive Dentsitry Residency, Army Postgraduate Dental School, Postgraduate Dental College, Uniformed Services University, Fort Bragg, NC, USA
3Program Director, Department of Prosthodontics, Army Postgraduate Dental School, Postgraduate Dental College, Uniformed Services University, Fort Eisenhower, GA, USA
4Staff Prosthodontist, Fort Bliss, Texas, USA
*Corresponding author: Andrew S Ryser, Prosthodontist, Comprehensive Dentsitry Residency, Army Postgraduate Dental School, Postgraduate Dental College, Uniformed Services University, Smoke Bomb Dental Clinic, 3817 Gruber Rd, Fort Bragg 28310, USA
Abstract
Fixed dental prostheses are crucial in returning damaged teeth to proper form and function. Retention and resistance play a crucial role in the long-term success of fixed dental prostheses. Determining taper and TOC of a tooth preparation for a fixed dental prosthesis can help determine its long-term prognosis and inform the provider if alterations to the preparation are necessary to increase retention and resistance form, or if adhesive cementation is necessary. This article describes a 3D printed tool that allows the provider to critically assess a tooth preparation to ensure success of a well-fitting retentive restoration.
Keywords: Digital Dentistry; Fixed Dental Prostheses; Crown; Resistance; Retention
Abbreviations: TOC: Total Occlusal Convergence
Introduction
Fixed dental prostheses return damaged or decayed teeth to function and ideal esthetics. The principles of tooth preparation for fixed dental prostheses can be broken down into three board categories which include: biological considerations, esthetic considerations, and mechanical considerations [1]. Biological considerations include margin placement that ensure the supracrestal tissue attachment is not violated and remains healthy, occlusion, conservation of tooth structure, pulpal considerations, removal of biological and protection of adjacent teeth. Esthetic considerations include minimum display of metal when desired, thickness of the ceramic, reduction of tooth to allow for porcelain stacking if necessary, and margin placement [1].
Mechanical factors for tooth preparation include retention and resistance form. Retention form is defined by the Glossary of Prosthodontic terms (10th ed.) as the quality inherent in the prosthesis acting to resist the forces of dislodgement along the path of placement [2]. Retention is is affected by several factors to include magnitude of the dislodging forces, geometry of the tooth preparation (circular vs square), roughness of the restoration, film thickness of the luting agent, and retention grooves or boxes. The glossary of prosthodontic terms defines resistance as the feature of a tooth preparation that enhances the stability of restoration and resists dislodgment along and axis other than the path of placement [2]. The factors that influence resistance form include tooth preparation length, tooth width, and taper.
Jorgensen in 1955 was the first to demonstrate the relationship between taper and retention of crowns [3]. The relationship proved to be hyperbolic, with retention rapidly becoming less as taper increases [3]. Taper is defined as the angle, measured in degrees as viewed in a given plane, formed between an external wall and the path of placement of a tooth preparation or machine surfaces on a metal or ceramic material when prepared for a fixed dental prosthesis [2]. Jorgensen tested taper and found that maximum retention occurred when taper was 5 degrees, and that retention was cut in half when taper was increased to 10 degrees [3].
Total occlusal convergence (TOC) is defined as the total angle of convergence, measured in degrees as viewed in a given plane, formed by opposing axial walls when a tooth or machined surfaces of a metal or ceramic material is prepared for a fixed dental prosthesis [2]. Total occlusal convergence is the combined taper of two opposing walls of a prepared tooth. Goodacre et al. in recommended total occlusal convergence to be 10-20 degrees, while Shillingburg at al. In 1997 recommended TOC to be 12 degrees for maximum retention [1,4]. Determining taper and TOC of a tooth preparation for a fixed dental prosthesis can help determine its long-term prognosis and inform the provider if alterations to the preparation are necessary to increase retention and resistance form, or if adhesive cementation is necessary. This article describes a 3D printed tool that allows the provider to critically assess a tooth preparation to ensure success of a well-fitting retentive restoration.
Materials and Methods
Shillingburg’s of 12 degrees of total occlusal convergence was used to design the tool in order to maximize retention of fixed dental prostheses (Fig. 1).
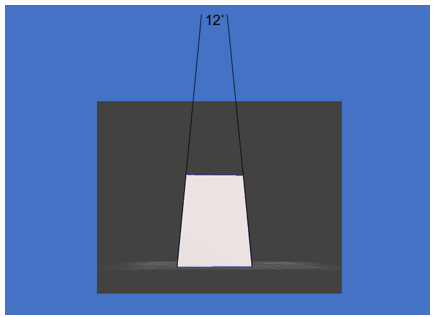
Figure 1: 12 Degrees Total Occlusal Convergence
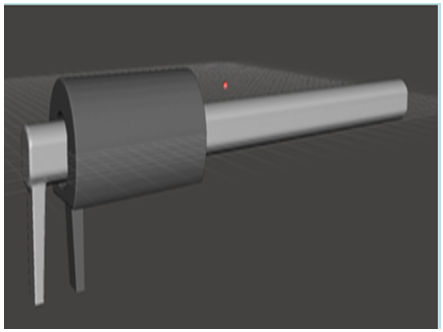
Figure 2: Digitally Designed Assessment Tool.
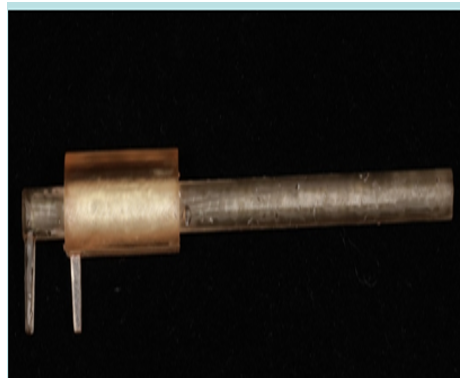
Figure 3: Printed Assessment Tool.
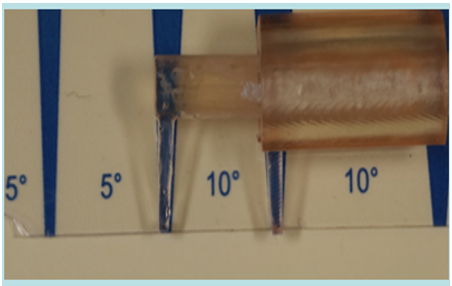
Figure 4: TOC Reference
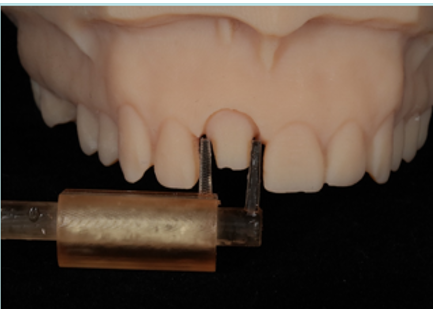
Figure 5: Assessment Tool Demonstrating TOC Greater Than 12 Degrees on Tooth Preparation
1. Using Meshmixer (Autodesk Inc. San Francisco, CA) a 12-degree TOC assessment tool prototype was designed (Fig. 2). Dimensions of tool: rod 80 mm in length, 6 mm in diameter. TOC tool has a piece that slides on the rod to allow for assessment of teeth with different widths mesial-distal, and facial-lingual.
2. The STL file was exported, and 3D printed in sterilizable surgical guide resin (Form labs Inc, Somerville, MA) (Fig. 3).
3. The Printed tool was polished and used as a guide to assess the convergence angle in the mesial-distal and buccal-lingual directions of a prepared model tooth (Figs. 4 and 5).
Discussion
Critically assessing a tooth preparation is essential to the success of a well-fitting, retentive restoration. The recommended convergence angle of 12 degrees allows for the fabrication of a restoration that will be retentive, reduces the chance of undercuts and facilitates seating of the restoration. Ohm and Silness in 1978 examined 190 stone dies that were prepared for single fixed dental prostheses, and they found that the mean convergence angle of the prepped teeth ranged from 12-37 degrees [5]. In 2004 Al-Omari et al evaluated 157 tooth preparations of dental students to assess total occlusal convergence. The authors found that the mean convergence angle faciolingually was 22.4 degrees, while the mean convergence angle mesiodistally was 25.3 degrees [6]. In the study molars showed a significantly different mean value compared to premolars and anterior teeth, [6] Abdulla et al. in 2018 analyzed the convergence angle of 206 crown preparations in private practice, they found that bucco-lingual and mesio-distal convergence angles significantly exceeded the clinically acceptable convergence angle of between 10 and 22, [7]. A comparative study in 2021 revealed the differences in the ability to obtain a clinically acceptable TOC between dental specialists and dental students. The study indicated that overall, 47% of the specialist observations achieved the recommended TOC angle, while 29.25% were obtained by the students [8].
Literature has shown that obtaining the ideal total occlusal convergence can be challenging. As previously mentioned, Goodacre states that a clinically acceptable range for total occlusal convergence is 10-20%, [4]. However, idealistic preparations with no undercuts are not always achievable, patient and provider factors play a significant role in the outcome of tooth preparation. Techniques to evaluate TOC have been described and include: photocopy machines, CAD/ CAM technology, and overhead projectors, however with the exception of CAD/ CAM technology these techniques are not available in the clinical setting [9-11]. Techniques to evaluate TOC intraorally include direct visualization from the buccal, lingual, mesial, distal, and occlusal using intraoral mirrors as the tooth is prepped. It has been suggested that using magnifying loupes would help improve access, vision, and efficiency while prepping teeth [12]. A study by Almaki et al. in 2019 looked at the effects of dental loupes magnification on TOC and concluded that low power magnification did not show significant difference in teeth prepared with dental loupes and without dental loupes [13]. Murbay et al. in 2023 concluded that the use of magnification did not improve the quality of tooth preparation and that total occlusal convergence was increased compared to the ideal values [14].
Multiple tools exist to aid in idealizing a tooth preparation, such as reduction guides and depth cutting burs. Taper of the preparation is typically assessed via direct or mirrored visualization, but this may be challenging for posterior teeth and studies show that providers tend to underestimate the TOC through direct visualization. Alternative methods such as using an intraoral scanner or impressing the tooth and evaluating the poured cast may be effective but can increase chair time. This article demonstrates a tool that is easy to use and can quickly analyze the tooth preparation to determine if there is ideal retention and resistance form. The adjustable component allows for analysis of teeth of different widths, and the handle allows for easy access to posterior dentition. The instrument can easily be printed utilizing a 3D printer and the tool can be sterilized if an appropriate resin is used or single use.
Summary
This article describes a technique that allows for the evaluation of TOC utilizing a 3D printed 12-degree assessment tool to efficiently check preparation design. The technique can help reduce errors in over or under tapering and improve retention and resistance form of the final restoration.
Disclaimer: The views expressed in this manuscript are those of the authors and do not necessarily reflect the official policy of the United States Government, the Department of Defense, the Defense Health Agency, the Department of the Army, the United States Army Medical Department, or Uniformed Services University.
Acknowledgements: This research did not receive any specific grant from funding agencies in the public, commercial, or non-profit sectors. The authors report no conflicts of interest.
References
- Shillingburg HT., Hobo S., Whitsett LD., et al. Principles of tooth preparation. In: Fundamentals of fixed prosthodontics, 3rd ed Chicago: Quintessence. 1997;119–137. [Ref.]
- The Glossary of Prosthodontic Terms 2023. J Prosthet Dent. 2023;130:e7–126. [PubMed.]
- Jorgensen KD. The relationship between retention and convergence angle in cemented veneer crowns. Acta Odontol Scand. 1955;13(1):35–40. [PubMed.]
- Goodacre CJ., Campagni WV., Aquilino SA. Tooth preparations for complete crowns: an art form based on scientific principles. J Prosthet Dent. 2001;85(4):363–376. [PubMed.]
- Ohm E., J Silness. The convergence angle in teeth prepared for artificial crowns. Journal of Oral Rehabilitation. 1978;5(4):371–5. [PubMed.]
- Al-Omari WM., Al-Wahadni AM. Convergence angle, occlusal reduction, and finish line depth of full-crown preparations made by dental students. 2004;35(4):287–93. [PubMed.]
- Abdulla F., Khamis H., Milosevic A., Abuzayda M. Convergence angles of all-ceramic full crown preparations performed in Dubai private practice. J Clin Exp Dent. 2018;10(12):e1192-e1197. [PubMed.]
- Al-Aali KA., AlHelal AA., Hejazi RY., Abuhaimed HM. Assessment of total occlusal Convergence for Crown Preparation: A Comparative Study. World Journal of Dentistry. 2020;11(1):61–4. [Ref.]
- Kirov D., Kazakova S., Krastev D. Convergence angle of prepared Typodont teeth for full veneer crowns achieved by dental students. Int J Sci Res. 2014;3:401–403. [Ref.]
- Ghasemi S., Mireskandari P., Ghanizdah M., et al. Comparison of the convergence angle in full-crown abutment teeth prepared by the pre-clinical and senior students in Faculty of Dentistry Tabriz University. World J Dent. 2017;8:77–80. [Ref.]
- Makker R., Choukse V., Upadhyay M., et al. Assesment and comparison of convergence angle of tooth preparations for full-veneer crowns among practitioners with different levels of experience. Int J Prevent Clin Dent Res. 2014;1:7–10. [Ref.]
- Maggio MP., Villegas H., Blatz MB. The effect of magnification loupes on the performance of preclinical dental students. Quintessence Int. 2011;42(1):45–55. [PubMed.]
- Almalki A., Almalki S., Bahgat T. Effect of Low Power Magnification on Total Occlusal Convergence Angles in Crown Preparation. International Journal of Prosthodontics and Restorative Dentistry. 2019;9:13–7. [Ref.]
- Murbay S., Neelakantan P., Li KY., Pow EHN. Effect of magnifying loupes on tooth preparation of complete coverage crown: A quantitative assessment using a digital approach. European Journal of Dental Education. 2023;27(4):1053–9. [PubMed.]