>Corresponding Author : Eric Hu
>Article Type : Case Report
>Volume : 4 | Issue : 4
>Received Date : 07 Dec, 2024
>Accepted Date : 18 Dec, 2024
>Published Date : 21 Dec, 2024
>DOI : https://doi.org/10.54289/JDOE2400116
>Citation : Hu E, Brunstein K, Kreider JK, Yoo A, Shute W, et al. (2024) Restoring Severe Tetracycline Stained Teeth with Milled Lithium Disilicate Ceramic Veneers: A Case Report with 14-Month Recall. J Dent Oral Epidemiol 4(4): doi https://doi.org/10.54289/JDOE2400116
>Copyright : © 2024 Hu E, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Case Report | Open Access
12-Year Advanced Education in General Dentistry Residency Program, Fort Cavazos, TX
2Army Postgraduate Dental School, Uniformed Services University of the Health Sciences, JBSA-Fort Sam Houston, TX
*Corresponding author: Eric Hu, Prosthodontics Department, 2-Year AEGD Residency Program, 36014 Wratten Drive, Building 36014, Fort Cavazos, TX 76544
Abstract
Tetracycline is a broad-spectrum antibiotic commonly used to treat bacterial infections in children and adults. One of the side effects of tetracycline is the intrinsic staining of teeth which often creates an esthetic concern that can affect one’s self-esteem. The severity, color of staining and presence of banding are dependent on the type of tetracycline used, as well as the duration, timing, and concentration used during odontogenesis of primary and permanent teeth. Treatment depends on the severity of the staining and can include external bleaching, microabrasion, direct resin restoration, ceramic veneers, or full-coverage crowns. This case report discusses the treatment planning and sequence of using milled lithium disilicate veneers to achieve predictable, esthetic and life-changing results for a patient with severe tetracycline staining.
Keywords: Adhesive Dentistry, CAD/CAM, Ceramic Veneers, Esthetics, Lithium Disilicate, Prosthodontics, Tetracycline Staining
Introduction
Tetracycline is a broad-spectrum, bacteriostatic antibiotic introduced in 1948 and is used to treat common bacterial infections in children and adults [1,2]. There are many types of tetracycline, including chlortetracycline, dimethylchlortetracycline, minocycline, doxycycline and oxytetracycline. One of the side effects of tetracycline use is intrinsic staining of teeth due to the ability of the antibiotic to chelate calcium ions during the tooth development calcification process [2]. The prevalence of dental staining from tetracycline and minocycline use has been reported to be approximately 3-6% in adults when taking more than 100mg per day during long-term use [2]. For children exposed to various tetracyclines, an incidence rate of dental staining between 23-92% has been reported [3]. In a study by Ibiyemi et al. evaluating 384 adolescents in rural Nigeria, 120 participants (31.2%) had some form of anterior discoloration. Tetracycline staining and enamel hypoplasia accounted for 5.4% of teeth discoloration among all participants [4].
Although the oral side effects from tetracycline use have been well established, it continues to be used by nursing mothers in parts of the world. For example, in a prospective study by Enabulele et al., they found that among 128 nursing mothers at a hospital in Nigeria, 53.9% were unsure if tetracycline is safe for use in children and 38.3% had administered it to their children [1]. Only 19.5% of the mothers who participated in the survey knew tetracycline use in children can result in oral side effects. Interestingly, the authors of the article also stated that tetracycline can be easily accessed in Nigeria as it is sold as an over-the-counter medication [1].
The severity, color of staining and presence of banding are dependent on the type of tetracycline used, as well as the duration, timing, and concentration used during odontogenesis of primary and permanent teeth [2]. The sensitive period for tetracycline staining in the permanent first molars begins at birth while enamel completion of second molars completes at eight years of age [5]. Therefore, tetracyclines should not be prescribed to patients before age eight [6]. The color of staining usually ranges from yellow to brown to gray and can intensify from oxidation when tetracycline is exposed to light [2]. In addition to intrinsic staining of teeth and bone, these drugs can also lead to enamel hypoplasia and depression of bone growth [2,7]. Tetracycline has been known to cross the placental barrier and can affect the developing fetus, and cases have been reported on infants with breastfeeding mothers [2,8]. Other conditions that can present with gray-brown tooth staining include dentinogenesis imperfecta (Shields type II), hemosiderin staining, dental trauma, and pulp necrosis [9].
The severity of tetracycline staining can be classified according to its color, intensity, and banding (Table 1). Treatment depends on the severity and varies based on the degree of staining. Prolonged external bleaching, microabrasion, or direct resin are preferable treatments for first and second degree stains. Internal bleaching can be considered for endodontically treated teeth for first and second degree stains but is ineffective for third degree stains [10]. Ceramic veneers or crowns should be considered for third degree stains [7,10-12].
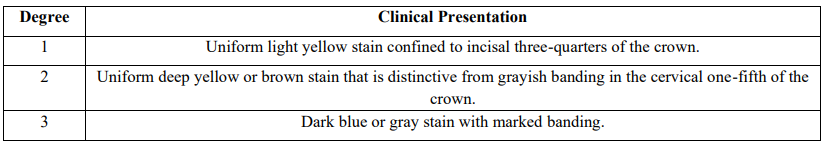
Table 1: Jordan and Boksman’s classification of tetracycline stained teeth10
When masking tetracycline-induced staining, the final indirect veneer color will depend on the ceramic type, shade, translucency, and thickness, along with the underlying dentin and cement shade. When indirect veneers are indicated, the ceramic of choice must be able to block out the underlying tetracycline stain while preserving natural esthetics and translucency. Lithium disilicate glass ceramics offer excellent esthetics, strength, predictable bonding, and have demonstrated long-term success [13,14]. Alternatively, zirconia is a high-strength polycrystalline ceramic that offers good masking ability. However, zirconia is more opaque than glass ceramics, where low translucency lithium disilicate (e.max CAD LT) was found to be significantly more translucent than 3-mol% yttria-stabilized tetragonal zirconia polycrystal (3Y-TZP), 4Y-TZP, and 5Y-TZP zirconia tested at 1mm thickness [15]. In addition, zirconia and its long-term predictability and success as a bonded facial veneer material has not been established in the literature [16]. This case report describes how monolithic lithium disilicate veneers can successfully transform a patient with severely stained teeth from tetracycline.
Case Report
A 35-year-old African American male presented with the chief complaint: “I don’t like the color of my teeth. I am depressed because a lot of people comment on the dark color of my teeth”. According to the patient, he was born in Nigeria and his mother received tetracycline while she was pregnant. The exact type of tetracycline, dosage and duration are unknown, but the dark gray-brown appearance of the patient’s teeth is consistent with chlortetracycline. The patient does not recall receiving tetracycline as a child but remembers having similar dark staining on his deciduous teeth. The pattern of this patient’s staining, which affects all of his permanent dentition, is consistent with exposure(s) to tetracycline between 30 months and 5 years of age [17].
Initial evaluation revealed generalized staining with a dark brown and gray appearance and banding in the middle and incisal third of his natural teeth, and dark yellow discoloration in the cervical third and lingual/occlusal surfaces. The extent of the patient’s staining was classified as third degree staining (Figure 1). The patient exhibited excellent oral hygiene, no known drug allergies, and denied any tobacco or coffee use. The patient presented with mutually protected occlusion with no missing dentition. All natural teeth exhibited normal pulpal response with normal apical tissues. The patient was diagnosed with obstructive sleep apnea and uses a continuous positive airway pressure machine. Esthetic evaluation revealed a low smile line, a dental midline about 1mm to the left of the patient’s facial midline, an irregular occlusal plane, irregular incisal edges, an asymmetric smile line and adequate lip support. The patient showed 0mm of maxillary incisors in repose. The patient exhibited slightly wide buccal corridors and presented with diastemata between maxillary lateral incisors, canines and first premolars. From the occlusal view, the patient exhibited an ovoid arch form with slightly retroclined maxillary incisors (Figure 2). Diagnostic impressions were made with irreversible hydrocolloid and casts were mounted on a semi-adjustable articulator with a facebow. Casts were cross-articulated in maximum intercuspation. Diagnostic wax-up was completed by lengthening maxillary incisors by approximately 0.5-1mm following curvature of the lower lip line, and adding approximately 0.5mm to the facial contours due to the slightly retroclined teeth position and dark zone of discoloration in the middle and incisal thirds.

Figure 1: Frontal view of patient presentation at initial evaluation

Figure 2: Occlusal view of patient presentation at initial evaluation
At the subsequent appointment, an intra-oral mockup was completed using bis-acryl (Luxatemp, DMG America) and a silicone putty matrix made from the diagnostic wax-up (Figure 3). Esthetics, phonetics, and occlusion were evaluated. The treatment plan was presented to the patient to include one round of in-office external bleaching and lithium disilicate veneers from teeth #4-13. The patient understood the rationale for staying conservative and did not wish to prep any mandibular teeth as they were not an esthetic concern. The patient accepted the treatment plan and was excited to move forward with treatment.
The patient returned at the following appointment where external bleaching was completed using 37.5% hydrogen peroxide gel (pola office+, SDI) following the manufacturer’s instructions. No noticeable color change was observed 2 weeks later at the veneer preparation appointment. At this appointment, the final shade (C1) for the veneers was discussed and agreed upon with the patient. Incisal edges were reduced by 1.5mm through the bisacryl mock-up. The mock-up was then removed, and a 0.5mm depth cutting diamond (LVS1, Brassler) was used for the facial reduction. A fine round-end taper diamond bur (8856.31.016FG, Brassler) was used to complete the veneer preparation to reach approximately 0.7mm total facial reduction in the middle and incisal third, and a 0.5mm reduction in the cervical third of the teeth. Facial reduction extended only halfway through interproximal contacts to improve esthetics where needed and to preserve enamel. Medium and fine-grit finishing discs (Sof-Lex, 3M) were used to refine the surface and create smooth contours. Size 000 retraction cords (Ultrapak, Ultradent) were placed along the gingival margin and preparation margins were kept equal-gingival. All preparation surfaces and margins remained in enamel and the opposing occlusion was at least 1.5mm from the veneer margin. Stumpf shade was selected (ND-8/9, IPS Natural Die Material Shade Guide, Ivoclar) at this time (Figure 4). A full arch definitive impression was made using extra-light and medium-bodied polyvinyl siloxane (Aquasil Ultra+, Dentsply Sirona). For provisionalization, all prepared teeth were spot etched in the center with 38% phosphoric acid for 15 seconds, then carefully suctioned, rinsed and air dried. A self-cured bisacryl provisional material (Luxatemp) was injected into the silicone matrix and seated on the teeth until bisacryl was fully set. After the silicone matrix was removed, the margins were trimmed, and the veneers were polished. Provisional veneers were kept splinted and a fine needle mosquito diamond bur (8392.31.016 FG, Brassler) was used to open gingival embrasures to allow threading of floss in order to maintain optimal gingival health.

Figure 3: Intra-oral mock up from diagnostic wax up

Figure 4: Veneer preparations and stumpf shade selection
In the dental laboratory, the definitive impression was poured in type IV stone (ResinRock, Whip Mix) and articulated to the existing mandibular cast on the articulator. Casts were then scanned and veneers were designed with computer-aided design software (inLab, Dentsply Sirona) using the diagnostic wax-up as a reference (Figure 5). Low translucency lithium disilicate ceramic veneers (e.max CAD LT C1, Ivoclar) were milled using a 4-axis mill (MCXL, Dentsply Sirona).
Additional contouring, polishing, glazing and crystallization were completed by a dental laboratory technician following the manufacturer’s instructions (Figure 6).
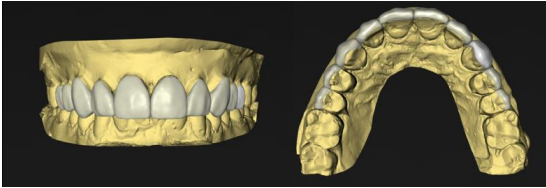
Figure 5: Computer aided-design of ceramic veneers

Figure 6: Milled lithium disilicate veneers prior to delivery
At the delivery appointment, provisional veneers were still intact. Provisional veneers were removed and all teeth preparations were cleaned with flour pumice. Veneers were then tried in with a water-soluble, glycerol-based try-in paste (Panavia V5 Try-in Paste, shade A-2, Kuraray) to assess proximal contacts, marginal integrity, occlusion and esthetics. After final adjustments and patient approval, the intaglio surface of the veneers were etched using 5% hydrofluoric acid (IPS Ceramic Etching Gel, Ivoclar) for 20 seconds, steam cleaned and then silanated with a ceramic primer (Clearfil Ceramic Primer Plus, Kuraray). Tooth preparation surfaces were total-etched with 38% phosphoric acid (Etch-Rite, Pulpdent) for 15 seconds, then rinsed and dried. A self-etching adhesive (Panavia V5 Tooth Primer, Kuraray) containing a proprietary polymerization activator was applied for 20 seconds with a microbrush before air drying. Veneers were cemented, starting with the central incisors, with a light-cured, amine-free, low-viscosity resin cement (Panavia Veneer LC, shade A2, Kuraray) under isolation. After bonding, a #12 blade was used to remove excess cement and the margins were polished. Periapical radiographs were taken to confirm sealed margins and cement removal. Post-operative intra-oral and extra-oral photographs were taken 2 weeks after delivery (Figures 7,8,9). One month after delivery, the patient stated “I am much happier now and I sleep much better at night. Thank you.” At the 14-month re-call examination, the patient was still very satisfied with the result. All ceramic veneers were in excellent condition with gingival health. No signs of fracture, marginal deterioration, staining, or color change were observed (Figure 10).

Figure 7: Intra-oral photo taken 2 weeks after delivery of ceramic veneers

Figure 8: Patient’s initial presentation and after delivery of ceramic veneers in repose

Figure 9: Patient’s initial presentation and after delivery of definitve veneers in full animation

Figure 10: Intra-oral photo taken at the 14-month re-call examination
Discussion
The final result described in this case report achieved satisfactory esthetics and was able to completely block out the underlying discoloration. Although some translucency was lost in the process, this case report demonstrated that monolithic lithium disilicate can be used on patients with severe tetracycline staining to create an esthetic result. Compromising on translucency to ensure the necessary block-out of the underlying shade is a decision backed by previous studies. In a study by Juntavee et al. which evaluated the masking properties of ceramic veneers on various underlying structures, the authors found that tetracycline-stained dentin was the most difficult to mask compared to natural dentin, zirconia or cast metal alloy [18]. The authors tested two zirconia-reinforced lithium silicate ceramics, where Vita Suprinity required 1.2mm thickness and Celtra Duo required 1.6mm to perfectly mask the tetracycline-stained dentine [18]. The greater thickness for Celtra Duo can be attributed to its slightly larger crystal structure compared with Vita Suprinity, which allows greater light transmission and a more translucent appearance. Similarly, Duraes et al. found that 1.2mm low translucent (LT) and medium opacity (MO) lithium disilicate ceramics offered the best masking ability over discolored teeth compared to thinner and more translucent lithium disilicate materials [19].
The key to enabling the utilization of the most conservative ceramic veneers possible involved planning with the end in mind. The end goal for this case was to achieve 1.0mm ceramic thickness in the cervical third and 1.2mm thickness in the middle and incisal third to completely block out the discoloration. This case was treatment planned to follow a traditional veneer preparation to reduce 1.5mm incisally with a butt-joint incisal edge design, 0.5mm facial reduction in the cervical third, 0.7mm facial reduction in the middle and incisal third while maintaining interproximal contacts to maximize enamel for bonding. Preparation margins were kept equigingival as it was esthetically acceptable, preserved enamel, maintained gingival health and cleansibility, and simplified veneer delivery. It is worth noting that for other cases with severely stained teeth, breaking through interproximal contacts and subgingival margins may be necessary to meet esthetic demands [20]. Low translucency lithium disilicate (e.max CAD LT) was selected in this case due to its better masking properties compared to predominately glass and high translucency lithium disilicate materials [16,19].Low translucency e.max CAD contains smaller crystals (0.8 x 0.2mm) compared to high translucency lithium disilicate (e.max CAD HT) (1.5 x 0.8mm), and has nanocrystals of lithium phosphate and lithium zinc silicate added to reflect light [16,21].The decision was also made with the patient to keep the veneers monolithic to minimize any potential complications related to fracture of veneered porcelain. Survival rates of 94% for glass-ceramic veneers and 87% for feldspathic veneers with a median follow-up period of 9 years have been reported in literature [22]. Fracture/chipping of veneers was the most common complication reported (4%), followed by debonding (2%), severe marginal discoloration (2%), endodontic problems (2%) and secondary caries (1%) [22].
Unfortunately, while childhood tetracycline use remains high in places like Nigeria, medication-induced staining will continue to present as a primary esthetic concern that dentists must be comfortable managing. If untreated, anterior tooth discoloration can have a tremendous effect on adolescent psychosocial development and may be associated with anxiety, depression, and timidity [4]. It is imperative dentists understand the treatment modalities to consider for each degree of tetracycline-induced staining, including techniques to utilize ceramic coverage for severe staining. This case report documents a suggested treatment flow to manage severe staining which other restorative dentists can leverage to improve patient’s self-confidence and mental wellness.
Conclusion
For tetracycline-stained teeth, the severity and location of staining must be considered when planning the preparation design, amount of tooth removal, and the type, translucency, and thickness of the ceramic. The final veneer shade is determined by the type of ceramic material, material thickness, and color of the underlying dentin and cement. This case report demonstrated that monolithic lithium disilicate veneers can completely cover underlying discoloration in a patient with severe tetracycline staining while achieving predictable, esthetic, and life-changing results.
Acknowledgments
A special thank you to Mrs. Andrea Bates, dental laboratory technician for design and fabrication of the ceramic restorations.
The authors declare that there are no conflicts of interest in this case report.
Disclaimer: The identification of specific products, scientific instrumentation, or organization is considered an integral part of the scientific endeavor and does not constitute endorsement or implied endorsement on the part of the author(s), Department of Defense, or any component agency. The views expressed in this article are those of the author(s) and do not reflect the official policy or position of the Department of the Army, Uniformed Services University of the Health Sciences, Defense Health Agency, Department of Defense, or the United States Government.
References
- Enabulele JE., Chukwumah NM., Enabulele O. Tetracycline use in children and knowledge of its oral implications among nursing mothers. Pediatr Dent J. 2020;30(3):224-30. [Ref.]
- Sánchez AR., Rogers RS., and Sheridan PJ. Tetracycline and other tetracycline-derivative staining of the teeth and oral cavity. Int J Dermatol. 2004;43:709-715. [PubMed.]
- Wang J., Zou D., Li Y., Liu P and Guo C. Drug-induced tooth discoloration: An analysis of the US food and drug administration adverse event reporting system. Front Pharmacol. 2023;14:1161728. [PubMed.]
- Ibiyemi O., Taiwo JO. Psychosocial aspect of anterior tooth discoloration among adolescents in igbo-ora. southwestern Nigeria. Ann Ib Postgrad Med. 2011;9(2):94-9. [PubMed.]
- McDonald RE., Avery DR., Dean JA. Dentistry for the Child and Adolescent. 9th ed. Mosby. 2010. [Ref.]
- Tredwin CJ., Scully C., Bagan-Sebastian JV. Drug-induced disorders of teeth. J Dent Res. 2005;84(7):596-602. [PubMed.]
- Al-Rawas MZ., Hin BY., Johari Y., Ab-Ghani Z., Husein A., et al. Minimum Intervention in Managing Two Cases of Tetracycline Staining of Different Severity. Cureus. 2022;14(1):e21289. [PubMed.]
- Vennila V., Madhu V., Rajesh R., Ealla KK., Velidandla SR., et al. Tetracycline-induced discoloration of deciduous teeth: case series. J Int Oral Health. 2014;6(3):115-119. [PubMed.]
- Watts A., Addy M. Tooth discolouration and staining: a review of the literature. Br Dent J. 2001;190(6):309-316. [PubMed.]
- Jordan RE., Boksman L. Conservative vital bleaching treatment of discolored dentition. Compend Contin Educ Dent (Lawrenceville). 1984;5(10):803-5, 807. [PubMed.]
- Bassett J., Patrick B. Restoring tetracycline-stained teeth with a conservative preparation for porcelain veneers: case presentation. Pract Proced Aesthet Dent. 2004;16(7):481-86. [PubMed.]
- Haywood VB., Pohjala R. Bleaching and esthetic bonding of tetracycline-stained teeth. Cont Esthet Rest Dent Prac. 2004;7:16-23. [Ref.]
- Malament KA., Margvelashvili-Malament M., Natto ZS., Thompson V., Rekow D., et al. Comparison of 16.9-year survival of pressed acid etched e. max lithium disilicate glass-ceramic complete and partial coverage restorations in posterior teeth: Performance and outcomes as a function of tooth position, age, sex, and thickness of ceramic material. J Prosthet Dent. 2021;126(4):533-45. [Ref.]
- Mazzetti T., Collares K., Rodolfo B., da Rosa Rodolpho PA., van de Sande FH., Cenci MS. 10-year practice-based evaluation of ceramic and direct composite veneers. Dent Mater. 2022;38(5):898-906. [PubMed.]
- Harada K., Raigrodski AJ., Chung KH., Flinn BD., Dogan S., Mancl LA. A comparative evaluation of the translucency of zirconias and lithium disilicate for monolithic restorations. J Prosthet Dent. 2016;116(2):257-263. [PubMed.]
- Skyllouriotis AL., Yamamoto HL., Nathanson D. Masking properties of ceramics for veneer restorations. J Prosthet Dent. 2017;118(4):517-23. [PubMed.]
- Logan WHG., Kronfeld R. Development of the human jaws and surrounding structures from birth to the age of fifteen years. J Am Dent Assoc. 1933;20(3):379-427. [Ref.]
- Juntavee N., Juntavee A., Phetpanompond S. Masking ability of different ceramics upon various underlying structures. J Esthet Restor Dent. 2022;34(2):430-9. [PubMed.]
- Durães I., A Cavalcanti and P Mathias. The thickness and opacity of aesthetic materials influence the restoration of discolored teeth. Oper Dent. 2021;46(5):559-65. [PubMed.]
- Rouse JS. Full veneer versus traditional veneer preparation: a discussion of interproximal extension. J Prosthet Dent. 1997;78(6):545-49. [PubMed.]
- Willard A., Gabriel Chu TM. The science and application of IPS e.Max dental ceramic. Kaohsiung J Med Sci. 2018;34(4):238-242. [PubMed.]
- Morimoto S., Albanesi RB., Sesma N., Agra CM., Braga MM. Main Clinical Outcomes of Feldspathic Porcelain and Glass-Ceramic Laminate Veneers: A Systematic Review and Meta-Analysis of Survival and Complication Rates. Int J Prosthodont. 2016;29(1):38-48. [PubMed.]