>Corresponding Author : Andrew S Ryser
>Article Type : Case Report
>Volume : 4 | Issue : 3
>Received Date : 22 July, 2024
>Accepted Date : 05 Aug, 2024
>Published Date : 09 Aug, 2024
>DOI : https://doi.org/10.54289/JDOE2400114
>Citation : Ryser AS, Handel SE, Sabol JV, Phillips MB and Majure AT. (2024) Expedited Treatment of a Fractured Tooth by Rebonding: A Case Report. J Dent Oral Epidemiol 4(3): doi https://doi.org/JDOE2400114
>Copyright : © 2024 Ryser AS, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Case Report Article | Open Access | Full Text
1Resident, Department of Prosthodontics, Army Postgraduate Dental School, Postgraduate Dental College, Uniformed Services University, Fort Eisenhower, GA, USA
2Assistant Director, Department of Prosthodontics, Army Postgraduate Dental School, Postgraduate Dental College, Uniformed Services University, Fort Eisenhower, GA, USA
3Director, Department of Prosthodontics, Army Postgraduate Dental School, Postgraduate Dental College, Uniformed Services University, Fort Eisenhower, GA, USA
4Resident, Department of Endodontics, Army Postgraduate Dental School, Postgraduate Dental College, Uniformed Services University, Fort Eisenhower, GA, USA
*Corresponding author: Andrew S Ryser, Resident, Department of Prosthodontics, Army Postgraduate Dental School, Postgraduate Dental College, Uniformed Services University, Fort Eisenhower, GA, USA
Abstract
Fractured maxillary anterior are a common occurrence when a person experiences trauma to the face. A patient sought treatment at a endodontics and prosthodontics practice after experiencing trauma to his maxillary right central incisor that resulted in a complete horizontal fracture. This case report describes a novel way to restore a fractured anterior tooth with a highly esthetic outcome that can be completed relatively easily in the clinic or in an austere environment.
Keywords: Fractured Tooth; Esthetics; Anterior Crown; Austere Dentistry; Fixed Prosthodontics; Field Medicine; Field Dentistry
Introduction
A patient presented to a prosthodontics clinic with a fractured maxillary central incisor. The soldier’s tooth fractured while participating in a physical fitness training. The tooth was asymptomatic and free of caries; however, the patient required treatment to restore esthetics and protect the tooth from sensitivity due to exposed dentin. The fracture was complicated with exposure of the pulp however it could easily be re-articulated back on to the tooth with clean margins. A treatment plan to bond the fractured portion of the crown back onto the tooth was presented and accepted by the patient.
Crown fractures of anterior teeth are one of the most common reasons patients report to a dental clinic due to trauma, and account for 20% of dental hard tissue injuries [1,2]. Maxillary anterior teeth are especially prone to trauma due to their location in the dental arch and play a vital role in esthetics and function [3]. When a crown fractures it can be classified as complicated or uncomplicated depending on if the pulp is involved [1]. Uncomplicated fractures occur when only the enamel and dentin is involved and the pulp is not exposed [4]. Complicated fractures include the involvement of enamel, dentin, and the pulp [4]. 28-44% of the permanent incisor fractures are uncomplicated while 11-15% are complicated [2]. When maxillary anterior teeth are fractured the patient can experience functional, esthetic, and phonetic limitations [3].
Immediate treatment of a fractured anterior tooth is ideal to prevent pulpal or periapical pathologies from developing. When treatment planning the clinician should consider a number of things to include: the age of the patient, extent and position of the fracture, supracrestal tissue attachment, and other structures such as the alveolar bone had been damaged [5]. If the fractured segment of tooth is available, the condition of the segment, occlusion, and esthetics plays a role in what treatment plan is possible [5]. The type of fracture affects the extent of treatment required for the patient. Uncomplicated fractures can be restored with direct or indirect restorations [6]. Complicated fractures with involve additional treatment such as root canal treatment and maybe a post and core.6 In the military or austere environments traditional treatment in a clinic might not be possible and the desired treatment plan such a resin restoration or crown might not be possible. Bonding of the fragmented segment back to the tooth might be a viable and quick option that can restore the patient’s function, phonetics and provide satisfactory esthetics [7].
Patient Information, Diagnostic Assessment, And Intervention
A 22-year-old patient presented to a prosthodontic practice with an complicated fracture of a maxillary central incisor (Fig. 1). The patient was transported to the dental clinic after experiencing trauma to the maxillary anterior teeth during physical fitness training. #8 displayed a mid-crown complete horizontal fracture, the pulpal tissue was exposed, no mobility, and the patient reported a moderate amount of sharp constant pain (Fig. 2). A pulpal and periapical diagnosis of symptomatic irreversible pulpitis and normal apical tissue was made. No other injuries were noted to adjacent teeth or intraoral and extraoral tissue. The fractured segment was brought with the patient and after cleaning with sterile saline it could be easily aligned back on the tooth and the margins displayed a clean fracture (Figs. 3 and 4). The patient was esthetically demanding and required a quick and long-term solution to return back to training as he was a student at Fort Eisenhower. The patient was scheduled for an overseas mission shortly after his school ended.
The patient was given the following treatment options: endodontics treatment and a direct resin composite restoration to build the tooth back to normal shape and form, or to bond the fractured tooth segment back on to the tooth to restore after completion of endodontics therapy. The patient elected for vital pulp therapy and to rebond the fractured segment back on to the tooth to restore contours and esthetics.

Figure 1: Initial presentation of patient.

Figure 2: Close up of fractured maxillary central incisor.

Figure 3: Fractured segment after cleaning with sterile saline.

Figure 4: Re-articulation of fractured segment back on to tooth.
The fractured maxillary central was anesthetized, and vital pulp therapy was completed with a rubber dam for isolation. Hemostasis was achieved and NeoMTA was placed over the exposed pulpal tissue. Vitrebond was then placed over the MTA. The fractured segment and the tooth were etched with 37% phosphoric acid and rinsed, bonding agent (Clearfill Primer and Bond) was applied to both segments, air dried, and light cured (Figs. 5 and 6). Flowable resin composite was then placed on both segments, the fractured segment was placed back on the tooth in proper position, and the resin was light cured (Fig. 7). Excess resin was removed and the area was polished (Fig. 8). Occlusion was adjusted to have the maxillary right central incisor in very light occlusion. A post-operative periapical radiograph was taken and the patient was able to return to training in a timely manner (Fig. 9). The patient returned at 1week and 1 month for follow up with stable tooth and pulpal/ periapical sensibility testing was normal, an athletic mouthguard was made for the patient and no further treatment was necessary. The patient was thrilled to be able to have his tooth back to “normal” and to retain the esthetics of his natural tooth.

Figure 5: Etching of tooth after vital pulp therapy was completed.

Figure 6: Etching of tooth fragment In preparation for bonding.
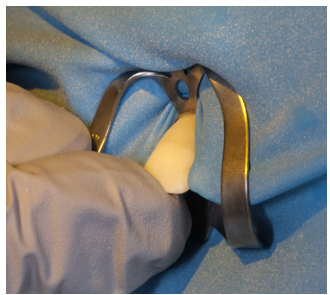
Figure 7: Bonding the fractured segment back onto the tooth using flowable resin.

Figure 8: Finished endodontic treatment and rebounded tooth segment.

Figure 9: Final post operative radiograph.
Discussion
Dental trauma affects around 5% of the global population annually, with the prevalence highly variable based on geographic location [8]. The risk of suffering trauma to the dentition varies based on age, location, profession, and culture with an increase in incidence when physical activities such as sports are participated in [8]. The maxillary centrals and laterals are the most common teeth to sustain an injury, and when trauma does occur most of the time a single tooth is affected [9]. In the military dental trauma incidence is high due to the nature of training and challenges of working in a war zone or other austere environments [10]. In a retrospective study by Becker and Ashkenazi in 2009 the authors found that the incidence of dental trauma in basic trainees was 1.1% during 8 months of training [10]. They also found that the maxillary central incisors were the most commonly traumatized tooth [10].
The rebonding of the fractured segment of a tooth can provide efficient treatment that results in a highly esthetic outcome that is a very conservative treatment option [11]. This procedure has several advantages to include: re-establishing function and esthetics, contours, natural translucency, shine, surface anatomy and texture, and original alignment of the tooth [12]. The use of the natural tooth segment to restore a fracture minimizes the problems associated with restorative materials to include: degradation of the restoration as it ages, discoloration of the restoration, and the challenges reproducing natural translucencies, textures, and contours [11]. Modern dentistry adhesive have allowed dentists performing this procedure to not only restore esthetics and function but to also preserve and strengthen the remaining tooth structure [11]. Rebonding of a fractured tooth segment can be considered an acceptable treatment plan when the segment is retrieved following the trauma, the fractured segment is relatively intact and in good shape, and it adapts well to the remaining tooth intraorally [13]. In the military rebonding of a fractured tooth segment not only restores function and esthetics, the procedure is quick, and requires very minimal supplies when compared to a direct resin restoration or an indirect restoration such as a veneer or crown. Military dentists could perform this procedure in a timely manner in a clinic or in an austere environment with nothing more than an etch, a bonding agent, a curing light, and a flowable resin or resin cement.
Conclusion
This case report demonstrates a relatively easy and quick technique to restore a complete horizontal fracture of a anterior tooth to restore function and esthetics in a clinic or when the provider is in an austere environment with limited resources. The patient who received this care had esthetics restored to a high degree of high satisfaction with no post operative complications allowing the soldier to complete his schooling and get ready for a deployment overseas. Rebonding a fractured segment back onto the tooth after endodontics treatment has proven to be a viable option when the fractured segment is in good condition, providing this treatment can restore the tooth close to pre-trauma esthetics and restore function and phonetics in a timely manner for the patient. This technique is easy to perform than a direct restoration such a resin composite and requires less time and resources than a indirect restoration such as a crown. In the military providers can quickly perform this treatment in less than ideal conditions to include field exercises, war zones, and humanitarian missions where supplies, time, and options are limited. Techniques such as the one described in this case report allow dentists to provide swift, quality care in a clinic or in an austere environment.
Declarations: none
Acknowledgments: Not applicable.
Prior Presentation: Not applicable.
Funding Sources: Not applicable.
Clinical Trial Registration: Not applicable.
Institutional Review Board (Human Subjects): Not applicable.
Institutional Animal Care and Use Committee (IACUC): Not applicable.
Competing Interests: Not applicable.
Data Availability Statement: The data that support the findings of this study are available on request from the corresponding author. All data is freely accessible.
Disclaimer: The views expressed in this manuscript are those of the authors and do not necessarily reflect the official policy of the United States Government, the Department of Defense, the Defense Health Agency, the Department of the Army, the United States Army Medical Department, or Uniformed Services University.
Institutional Clearance: Does not apply.
References
- Lakshmaiah D, Sr V, Ilango S, Sakthi N, Ps S. Management of Complex Crown Fractures: A Case Series. Cureus. 2023;15:e37907. [PubMed.]
- Divakar HD, Nayak M, Shetty R. Changing concepts in fracture reattachment of teeth—a case series. Endodontology. 2009;21:48-54. [Ref.]
- Andreasen JO. Etiology and pathogenesis of traumatic dental injuries. A clinical study of 1,298 cases. Scand J Dent Res. 1970;78:329-342. [PubMed.]
- Taguchi CM, Bernardon JK, Zimmermann G, Baratieri LN. Tooth fragment reattachment: a case report. Oper Dent. 2015;40:227-234. [PubMed.]
- Olsburgh S, Jacoby T, Krejci I. Crown fractures in the permanent dentition: pulpal and restorative considerations. Dent Traumatol. 2002;18:103-115. [PubMed.]
- Garcia FCP, Poubel DLN, Almeida JCF, Toledo IP, Poi WR, Guerra ENS, Rezende LVML. Tooth fragment reattachment techniques-A systematic review. Dent Traumatol. 2018. 34:135-143. [PubMed.]
- Diangelis AJ, Andreasen JO, Ebeleseder KA, Kenny DJ, Trope M, Sigurdsson A, et al. International Association of Dental Traumatology guidelines for the management of traumatic dental injuries: 1. Fractures and luxations of permanent teeth. Dent Traumatol. 2012;28:02-12. [PubMed.]
- Glendor U. Aetiology and risk factors related to traumatic dental injuries—A review of the literature. Dent. Traumatol. 2009:25:19-31. [PubMed.]
- Zaleckienė V, Peciuliene V, Brukiene V, Drukteinis S. Traumatic dental injuries: Etiology, prevalence and possible outcomes. Stomatologija 2014;16:7-14. [PubMed.]
- Becker T, Ashkenazi M. Incidence of reported dental trauma among soldiers during basic training. Military medicine. 2009;1:174(2):190-2. [PubMed.]
- Chu FC, Yim TM, Wei SH. Clinical considerations for reattachment of tooth fragments. Quintessence Int. 2000;31:385-91. [PubMed.]
- Martos J, Zanotto S, Cocco AR, Lund RG, Baldissera RA. Natural Crown Bonding of Anterior Fractured Teeth at Different Levels of Complexity: A 14-Month Follow-up. Contemp Clin Dent. 2018;9:S160-S163. [PubMed.]
- Macedo GV, Ritter AV. Essentials of rebonding tooth fragments for the best functional and esthetic outcomes. PubMed. 2009;31:110-6. [Ref.]