>Corresponding Author : Hlaibi Omnia
>Article Type : Case Report
>Volume : 6 | Issue : 1
>Received Date : 25 Jan, 2026
>Accepted Date : 06 Feb, 2026
>Published Date : 11 Feb, 2026
>DOI : https://doi.org/10.54289/JCRMH2600104
>Citation : Hasnae S, Omnia H, Aicha G, Amine L, Mohammed J, et al. (2026) Ovarian Ectopic Pregnancy: A Case Study. J Case Rep Med Hist 6(1): doi https://doi.org/10.54289/JCRMH2600104
>Copyright : © 2026 Aicha G, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Case Report | Open Access | Full Text
1Departement of gynecology and obstetrics, University Hospital Center Ibn Rochd, Casablanca 20100, Morocco
2Faculty of Medicine and Pharmacy, Hassan II University of Casablanca, Casablanca, Morocco
*Corresponding author: Hlaibi Omnia, Departement of gynecology and obstetrics, University Hospital Center Ibn Rochd, Casablanca 20100, Morocco and Faculty of Medicine and Pharmacy,Hassan II University of Casablanca,Casablanca, Morocco
Abstract
Ovarian pregnancy is a rare type of ectopic pregnancy, accounting for about 3% of cases. It is characterized by implantation of the gestational sac within the ovary and differs from tubal ectopic pregnancy by the absence of typical risk factors. Its pathophysiology remains unclear, although reflux of the fertilized ovum into the ovary is the most accepted theory.
We report the case of a 28-year-old woman presenting with pelvic pain, light metrorrhagia, and 4 weeks of amenorrhea. Ultrasound showed an empty uterus and a left ovarian mass with a β-hCG level of 1650 IU/L. Surgical exploration confirmed a left ovarian pregnancy with hemoperitoneum and normal fallopian tubes. Conservative surgical treatment was performed.
Diagnosis is challenging and often made intraoperatively or by expert ultrasound. Management is mainly surgical, and prognosis is generally favorable.
Abbreviations: OP: Ovarian Pregnancy, EUP: Extrauterine Pregnancy, 3D: Three-Dimensional, MTX: Methotrexate
Introduction
Ovarian pregnancy (OP) is a type of pregnancy in which the ovary is the site of implantation [1]. It occupies a special place among ectopic pregnancies due to its rarity, which is linked on the one hand to its definition, which takes anatomical criteria into account, and on the other hand to well-codified diagnostic procedures. Unlike other types of extrauterine pregnancy (EUP), OP remains an isolated and exceptional phenomenon, independent of the usual risk factors. This is all the more so given that the exact mechanism leading to OP is still poorly understood. Compared to other EP, other forms of GO have been reported, such as GO that can progress into the second trimester or even to term [2]. The objectives of this study are to analyse the determining factors of GO and to support the aetiopathogenic, histopathological and evolutionary characteristics of this ectopic pregnancy.
Observation
Ms. I R, aged 28, G2 P1, was admitted to the LALLA MERIEM Maternity Ward for light metrorrhagia, pelvic pain and a 4-week delay in her period, with a history of using injectable progestogen contraception for 8 years.
The initial clinical examination found the patient conscious, with a pulse rate of 118, blood pressure of 09/06, profuse sweating, and marked abdominal tenderness on the left side.
Pelvic ultrasound showed an empty uterus (Figure 1) and a 6x6 cm mass on the left side of the uterus, affecting the left ovary (Figure 2), with BHCG at 1650 IU.
Surgical exploration revealed a left-sided ectopic pregnancy, profuse effusion, a slightly enlarged uterus, with no abnormalities in the left fallopian tubes or right adnexa (Figure 3).
Conservative treatment was performed (Figure 4).
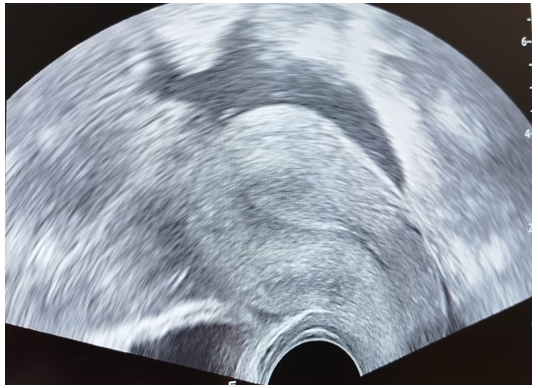
Figure 1. Radiological image of uterine emptiness
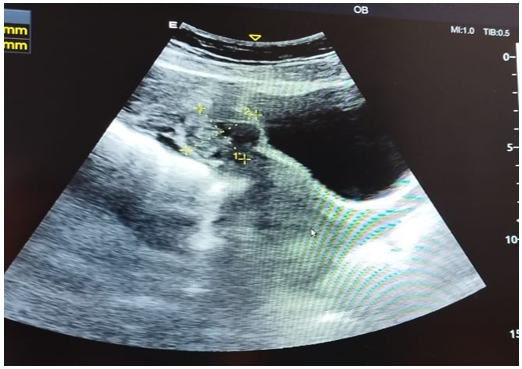
Figure 2. Radiological image of the ovarian ectopic pregnancy mass
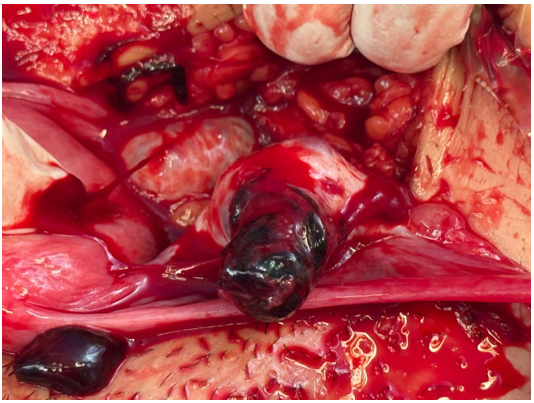
Figure 3: Intraoperative ovarian ectopic pregnancy
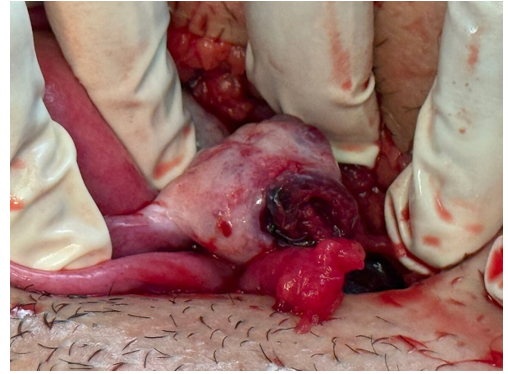
Figure 4: Conservative treatment
Discussion
Ovarian pregnancy (OP) accounts for 3% of ectopic pregnancies [3]. Its pathophysiology is poorly understood, but it appears to be secondary to reflux of the fertilised egg back into the ovary [3]. Cases of OP following in vitro fertilisation reported in the literature support the reflux theory [4]. The pregnancy implants preferentially on the scar of the original follicular ostium, which is rich in fibrin and new capillaries [5]. This theory corresponds to the intra-follicular and juxtapositional forms. More rarely, this Implantation will occur away from the corpus luteum or even on the contralateral ovary, corresponding to the juxtacortical and interstitial forms, the pathophysiology of which remains unclear. More rarely, ectopic pregnancy may be bilateral or part of a heterotopic pregnancy [6]. In our series, all pregnancies were single and implanted on the side of the corpus luteum. Unlike tubal ectopic pregnancies, tubal pathology and surgery do not appear to increase the risk of GO. However, there is no consensus among authors on the role of inflammatory pelvic pathologies in the genesis of GO [7]. Furthermore, contraception using an intrauterine device appears to be particularly associated with ovarian pregnancies [8]. Indeed, several authors studying series of 7 to 26 OPs [9] noted that between 57% and 90% of patients had an intrauterine device. Clinically, painful abdominal and pelvic symptoms precede the onset of the condition. These pains correspond to the rupture of the ovarian capsule due to pregnancy and the formation of haemoperitoneum [10]. Patients are most often seen in an emergency setting, in a state of shock [11]. In our patients, abdominal and pelvic pain was indeed the primary symptom, and one patient was in haemorrhagic shock. The diagnosis of ovarian pregnancy can be made by ultrasound by a skilled operator. A gestational sac adjacent to the ovary can be seen, or, as some have described, a double hyperechoic ring within a hypoechoic lateral uterine mass with or without an embryo [12]. In fact, depending on the age of the pregnancy, several ultrasound images have been described in the literature [13]. Certain ultrasound criteria are highly suggestive of an ovarian pregnancy: the presence of a round anechoic image with a hyperechoic crown on the surface of the ovary, the presence of ovarian parenchyma such as a corpus luteum or follicle surrounding the mass, and a higher echogenicity of the mass than that of the ovary [14]. The differential diagnosis often involves a corpus luteum cyst or a haemorrhagic cyst. In this case, three-dimensional (3D) ultrasound seems to be able to make the distinction thanks to the cross-sectional planes [15]. Energy Doppler does not appear to be useful for diagnosis [16]. Pulsed Doppler appears to be more useful. Several surgical techniques have been described: wedge resection of the ovary removing the GO, enucleation of the GO, cystectomy of the corpus luteum removing the trophoblast, curettage of the trophoblast with coagulation or haemostatic suturing of the GO bed with total preservation of the ovary [17]. In rare cases, due to the advanced stage of pregnancy, oophorectomy or even adnexectomy may be necessary [13]. This was the case with our patient. Indeed, GO is often diagnosed at a stage where complications prevent the use of first-line medical treatment [12]. The addition of methotrexate (MTX) may be considered as a follow-up to insufficient surgical treatment. We did not use MTX. In terms of prognosis, GO does not constitute a risk factor for a new ECT, due to the absence of tubal involvement. Only one case of GO recurrence has been described in the literature, involving the contralateral ovary [11]. Pathological examination is of paramount importance, as it is the only way to confirm the diagnosis of GO. Its purpose is to eliminate primitive abdominal pregnancies, those implanted on the ovary but originating from a tubo-abdominal abortion, and those where the ovary is not the exclusive site of implantation, according to Spielberg's anatomical criteria of 1878 [14] the fallopian tube on the affected side, including the fimbriated end, must be free of any lesions; the ovular sac must occupy the usual anatomical position of the ovary; the ovary and gestational sac must be connected to the uterus by the utero-ovarian ligament; there must be ovarian tissue within the ovular sac, which implies histological confirmation of the presence of chorionic villi within the ovarian tissue. Based on the anatomical criteria defined by certain authors [15,16], several classifications of GO have been proposed.
Conclusion
Ovarian pregnancy is a rare condition that presents certain semiological characteristics compared to other ectopic pregnancies. It is difficult to diagnose. Treatment remains surgical. Although rare, ovarian pregnancy remains an obstetric emergency with specific semiology depending on complications at different stages of pregnancy. Its diagnosis remains difficult and is often made intraoperatively, through ultrasound by an experienced practitioner, given the limited possibilities presented by the semiology, and is also based on intraoperative findings. Management is surgical despite advances in medical treatment. Informed consent for the publication of their clinical details and/or clinical images has been obtained from the patient.
Conflict of interest
The authors declare no conflict of interest.
References
- Chahtane A., Dehaymi M., Rhrab B., Kharbach A., El Armani S., Chaoui A. Ovarian pregnancy. Four cases with review of the literature. Revue Française de Gynecologie obstetrique. 1993;88(1):35–38. [PubMed.]
- Shahabuddin A., Chowdhury S. Primary term ovarian pregnancy superimposed by intrauterine pregnancy: a case report. J Obstet Gynaecol Res. 1998;24(2):109–114. [PubMed.]
- Sergent F., Mauger-Tinlot F., Gravier A., Versycke E., Marpeau L. Grossesses ovariennes: reevaluation des criteres diagnostiques. J Gynecol Obstet Biol Reprod (Paris). 2002;31(8):741–6. [PubMed.]
- Kraemer B., Elizabeth K., Ersin G., Juhasz-Boess I., Erich-Franz S., Diethelm W., et al. Ovarian ectopic pregnancy: diagnosis, treatment, correlation to carnegie stage 16 and review based on a clinical case. Fertil and Steril. 2009;92:392. [PubMed.]
- Molinaro TA., Barnhart KT. Ectopic pregnancies in unusual locations. Semin Reprod Med. 2007;25:123–30. [PubMed.]
- Comstock C., Huston K., Lee W. The ultrasonographic appearance of ovarian ectopic pregnancies. Obstet Gynecol. 2005;105(1):42-5. [PubMed.]
- Ghi T., Banfi A., Marconi R., Iaco PD., Pilu G., Aloysio DD., et al. Three dimensional sonographic diagnosis of ovarian pregnancy. Ultrasound Obstet Gynecol. 2005;26(1):102–4. [PubMed.]
- Jourdain O., Fontangged M., Schiano A., Rauch F., Gonnet JM. Prise en charge des autres ectopies annexielles (cornuale, interstitielle, angulaire, ovarienne). J Gynecol Obstet Biol Reprod (Paris). 2003;32(7 Suppl): S93–100. [Ref.]
- Pan H., Huang L., Lee J., Hwang J., Chang J. Ovarian pregnancy torsion. Arch Gynecol Obstet. 2004;270(2): 119–121. [PubMed.]
- Sergent F., Mauger F., Gravier A., Verspyxk E., Marpeau L. Ovarian pregnancies: revaluation of diagnostic criteria. J Gynecol Obstet Biol Reprod. 2002;31(8):741–746. [PubMed.]
- Chahtane A., Dehaymi M., Rhrab B., Kharbach A., El Armani S., Chaoui A. La grossesse ovarienne: a propos de 14 observations avec revue de la litterature. Revue Française de Gynecologie obstetrique. 1993;88(1): 35–38. [Ref.]
- Renaud R., Voury-Heyler C., Leissner P., Chesnet Y., Sangaret M., Serres JJ., et al. Les grossesses abdominales apres le 6e mois, revue de la litterature: a propos de 8 cas. Gynecol Obstet. 1969;68(3):297–318. [PubMed.]
- García-Ferreyra J., Roly H., Duenas J. Ectopic ovarian pregnancy after intracytoplasmic sperm injection with testicular spermatozoa –a case report. JBRA Assist Reprod. 2017;21(2):135–136. [PubMed.]
- Andrea T., Gernot H., Antonio M., Raffaele T. Laparoscopic management of ovarian pregnancy. JSLS. 2008;12(2):169–72. [PubMed.]
- Sangeeta J., Kate B., Asif Q., Arshad I. Ovarian ectopic pregnancy. BMJ Case Rep. 2011;2011:bcr0820103250. [PubMed.]
- Comstock C., Huston K., Lee W. The ultrasonographic appearance of ovarian ectopic pregnancies. Obstet Gynecol. 2005;105:42–5. [PubMed.]
- Tabassum M., Atmuri K. The unexpected ovarian pregnancy at laparoscopy: a review of management. Case Rep Obstet Gynecol. 2017;2017:9856802. [PubMed.]