>Corresponding Author : Bahlioui Fatima Ezzahra
>Article Type : Case Report
>Volume : 5 | Issue : 12
>Received Date : 26 Oct, 2025
>Accepted Date : 06 Nov, 2025
>Published Date : 03 Dec, 2025
>DOI : https://doi.org/10.54289/JCRMH2500159
>Citation : Ezzahra BF, Zahra CF, Benchrifi Y, Mustapha B, Mohamed E, et al. (2025) Metaplastic Breast Carcinoma: 1 Case Report and Review of the Literature. J Case Rep Med Hist 5(12): doi https://doi.org/10.54289/JCRMH2500159
>Copyright : © 2025 Ezzahra BF, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Case Report | Open Access | Full Text
1Resident Physician, Department of Gynecology and Obstetrics at the Ibn Rochd University Hospital, Casablanca, Morocco
2Professor in the Department of Gynecology and Obstetrics at the Ibn Rochd University of Hospital in Casablanca Morocco
*Corresponding author: Bahlioui Fatima Ezzahra, 1Resident Physician, Department of Gynecology and Obstetrics, at Ibno Rochd University Hospital, Casablanca, Morocco
Abstract
Metaplastic breast carcinoma is a rare and hetero geneous form of breast cancer characterized by the coexistence of epithelial and mesenchymal components. Accounting for less than 1% of malignant breast tumors, it is distinguished by its aggressiveness, relative resistance to conventional treatments, and frequent association with the triple-negative phenotype. The Diagnosis is based on histopathology and immunohistochemistry, while management relies primarily on surgery, supplemented in some cases by chemotherapy and/or radiotherapy. The prognosis remains poor compared to other types of invasive breast carcinomas, hence the importance of early diagnosis and an appropriate therapeutic approach.
Keywords: Metaplastic Carcinoma, Breast, Triple Negative, Histopathology, Prognosis
Abbreviations: MBC: Metaplastic Breast Carcinoma
Introduction
Metaplastic breast carcinoma (MBC) is a rare entity representing approximately 0.2 to 1% of all invasive breast cancers [1]. It is characterized by the transformation of malignant epithelial cells into non-glandular or mesenchymal elements, resulting in a wide variety of morphologies [2]. This type of tumor, often associated with a triple-negative profile, has a more unfavorable clinical course than classic invasive ductal carcinoma [3].
Case report
This is a 66-year-old female patient, mother of three children born vaginally, menopausal for 15 years, with no particular medical history, presenting for follow-up care for metaplastic carcinoma of the left breast.
Her history of the disease dates back five months, when she felt a lump in her left breast during a self-examination. The initial clinical examination revealed a 5 cm mass at the junction of the lower left quadrants, which was mobile in both planes.
Initial echo-mammography: Suspicious lesion measuring 47x32 mm at the junction of the lower quadrants of the left breast + Left axillary lymphadenopathy, some of which have a thickened cortex, the largest measuring 11x7 mm: Examination classified as ACR5 on the left (Figure 1).
-Tru-cut biopsy: Atypical myxoid spindle cell proliferation.
-A left lumpectomy was performed, with pathological examination confirming metaplastic carcinoma with the presence of vascular emboli.-IHC: PR: 30%, ER: negative, HER2 negative.
Two months after the lumpectomy, the patient presented with a 3 cm mass at the junction of the inner quadrants of the left breast, with no signs of inflammation or nipple discharge, and a clean lumpectomyscar.
Breast ultrasound: Formation of a hypoechoic, multilobulate doval structure measuring 22.7 x 15.4 mm in the lower inner quadrant + bilateral axillary lymphnodes with preserved architecture.
A left mastectomy with left axillary lymphnode dissection was performed, with pathological examination revealing an un differentiated malignant tumor measuring 3.5 cm in diameter, consistent with known metaplastic carcinoma (SBRIII). Significant necrotic hemorrhagic changes were present in the center of the tumor. Deep dermal infiltration without epidermal involvement or ulceration. No in situ component, vascularemboli, or nerve sheathing. The resection margins were clear. Else where, sclerosing mastopathy, hemorrhagic changes, cyto-steatonecrosis, and resorptive giant cell granulomas. No lymphnode metastasis (0N+/10N).
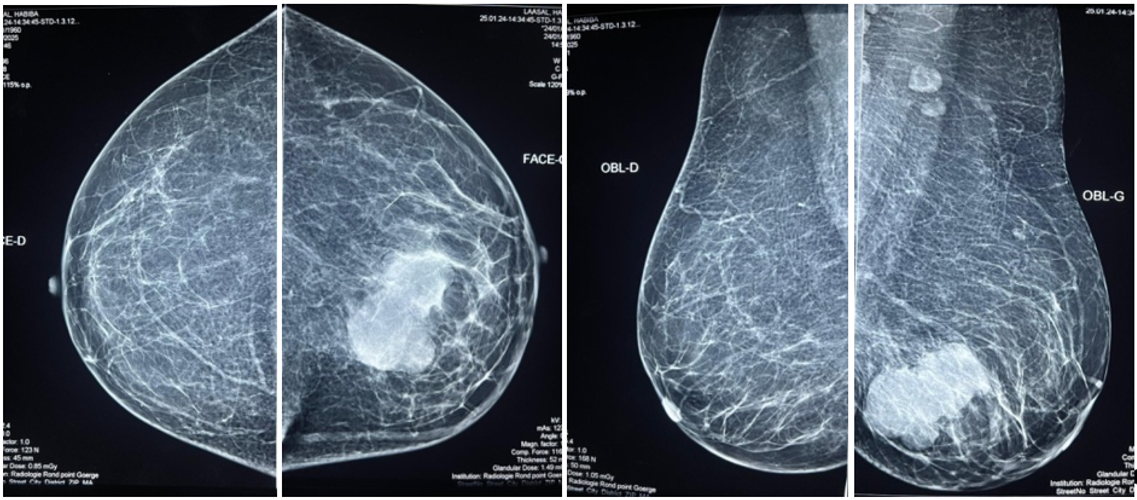
Figure 1: Initial mammo showing a lesion at the junction of the lower quadrants
Discussion
Metaplastic breast carcinoma mainly affects middle-aged to older women, with peak incidence around the sixth decade of life [4]. Clinically, it most often presents as a palpable, firm, sometimes painful, and rapidly growing mass [5]. Imaging tests, such as mammography and ultrasound, may show masses with irregular contours, but do not allow it to be specifically distinguished from other malignant breast lesions [6]. MRI may be useful in assessing local extension.
The definitive diagnosisis based on histological examination, which reveals the coexistence of carcinomatous components and metaplastic areas of sarcomatoid, squamous, or chondro-osseous appearance [7]. Immuno histo chemistry is essential to confirm the epithelial nature of the cells, with the expression of cytokeratins and often the absence of hormone receptors and HER2 [8].
From a therapeutic stand point, surgery is the corner stone of treatment, generally in the form of mastectomy or wide local excision combined with lymphnode dissection or sentinel lymphnode biopsy [9]. Adjuvant chemotherapy is offered, although CMS is generally less sensitive to chemotherapy the another triple-negative breast cancers [10]. Radiotherapy is indicated depending on local risk factors.
The prognosis for CMS is generally less favorable than for invasive ductal carcinomas of the same stage [11]. The rates of local recurrence and distant metastases, particularly to the lungs and bones, are higher. Five-year overall survival varies between 49% and 68% depending on the series [12]. Therapeutic prospects include the exploration of new moleculartar gets and the use of immuno therapies, with encouraging preliminary results [13].
Conclusion
Metaplastic breast carcinoma is a rare and aggressive tumor, the diagnosis of which relies on rigorous histo pathological analysis. Its management requires a multidisciplinary approach, and on going research aims to improve prognosis through innovative therapeutic strategies. Knowledge of its clinical and biological characteristicsis essential for optimizing management.
References
- Tse GM., et al. Metaplastic carcinoma of the breast: a clinic opathological review. J Clin Pathol. 2006;59(10):1079‒1083. [PubMed.]
- Reis‒Filho JS., et al. Metaplastic breast carcinoma: a special type of triple‒negative breast cancer. Breast. 2006;15(1):14‒21. [Ref.]
- Rayson D., et al. Metaplastic breast cancer: prognosis and response to systemic therapy. Ann Oncol. 1999;10(4):413‒419. [PubMed.]
- Luini A., et al. Metaplastic carcinoma of the breast, an unusual disease with worse prognosis: the experience of the European Institute of Oncology and review of the literature. Breast Cancer ResTreat. 2007;101(3):349‒353. [PubMed.]
- Rakha EA., et al. Prognostic markers in triple‒negative breast cancer. Cancer. 2007;109(1):25‒32. [PubMed.]
- Günhan-Bilgen I., et al. Metaplastic carcinoma of the breast: clinical, mammographic, and sonographic findings with histopathologic correlation. AJR Am J Roentgenol. 2002;178(6):1421‒1425. [PubMed.]
- Wargotz ES., Norris HJ. Metaplastic carcinomas of the breast. I. Matrix-producing carcinoma. Hum Pathol. 1989;20(7):628‒635. [PubMed.]
- Leibl S., Moinfar F. Metaplastic breast carcinomas are negative for HER2 but frequently express EGFR. Histopathology. 2005;46(5):441‒447. [PubMed.]
- Pezzi CM., et al. Characteristics and treatment of metaplastic breast cancer: analysis of 892 cases from the National Cancer Data Base. Ann SurgOncol. 2007;14(1):166‒173. [PubMed.]
- Bae SY., et al. Prognosis of metaplastic breast cancer: comparison with triple-negative breast cancer. Breast Cancer ResTreat. 2011;126(2):471‒478. [PubMed.]
- Ong CT., et al. Metaplastic breast cancer: clinic opathologic features and outcome in a single institution. Ann Acad Med Singapore. 2006;35(9):595‒599. [Ref.]
- Lester TR., et al. Metaplastic breast cancer: clinic opathologic features and prognostic factors. Am J Surg Pathol. 2015;39(6):711‒718. [Ref.]
- Adams S., et al. Current landscape of immunotherapy in breast cancer: a review. JAMA Oncol. 2019;5(8):1205‒1214. [PubMed.]