>Corresponding Author : Douha El Karoini
>Article Type : Case Report
>Volume : 5 | Issue : 12
>Received Date : 15 Nov, 2025
>Accepted Date : 25 Nov, 2025
>Published Date : 06 Dec, 2025
>DOI : https://doi.org/10.54289/JCRMH2500157
>Citation : El Karoini D, Dinia A, Bouadi O, Boufettal H, Mahdaoui S, et al. (2025) Non-Puerperal Uterine Inversion: A Rare Complication of Submucous Fibroids. J Case Rep Med Hist 5(12): doi https://doi.org/10.54289/JCRMH2500157
>Copyright : © 2025 El Karoini D, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Case Report | Open Access | Full Text
1Resident Physician, Department of Gynecology and Obstetrics at the Ibn Rochd University Hospital, Casablanca, Morocco
2Professor in the Department of Gynecology and Obstetrics at the Ibn Rochd University of Hospital in Casablanca Morocco
*Corresponding author: El Karoini Douha, Resident Physician, Department of Gynecology and Obstetrics, Ibn Rochd University Hospital, Casablanca, Morocco
Abstract
Non-puerperal uterine inversion is an exceptionally uncommon condition, most frequently described in multiparous patients. It is typically triggered by an underlying uterine mass, either benign or malignant, with submucous myomas being the most frequent cause. Diagnosis is often challenging due to its nonspecific presentation. In younger women, this condition may raise suspicion of an associated malignancy. We present the case of a 44-year-old woman who developed a non-puerperal uterine inversion secondary to a benign submucous fibroid.
Keywords: Non-Puerperal Uterine Inversions, Submucous Myoma, Abnormal Uterine Bleeding
Introduction
Uterine inversion is more commonly described as an obstetric complication than a gynaecological one; it is defined as the inverting of the uterus into a finger or ‘uterine invagination’. Uterine inversion is serious and can be life-threatening due to the hypovolaemic shock it causes [1]. Several degrees of inversion have been described, depending on the location of the uterine fundus. This unusual complication may lead to a delay in diagnosis, given the paucity of imaging data. The main differential diagnosis is a fibroid delivered through the cervix. The aim of our work is to report the case of a chronic non puerperal uterine inversion in a 44-year-old woman with no particular pathological history, apart from a full-term delivery and an abortion, who consulted us for intermittent menometrorrhagia of low intensity which had been evolving for 7 months.
Observation
A 44-year-old patient, nulligravid, with no particular pathological history presented with abnormal uterine bleeding and dysmenorrhoea. Clinical examination revealed an asthenic, tachycardic patient with pale skin and mucous membranes; gynaecological examination revealed vulvar external bleeding, but the examination under speculum and vaginal touch were not performed as the patient was a virgin. Preoperative ultrasound showed a uterus with heterogeneous material visualised in a thickened endometrial cavity measuring 53.9 × 51.4 mm. Pelvic MRI showed the mass as a pedunculated and prolapsed submucosal myoma. Myomectomy was scheduled. Surgical exploration confirmed the diagnosis of uterine inversion with a 5x5cm submucosal myoma.
We opted for a surgical management with a double approach: vaginal route with laparotomy (figure 1). Manual reduction of the uterus after myomectomy (figure2). Conservative treatment was carried out after checking the vascularisation of the uterus and adnexa, given the patient's desire to become pregnant. The post-operative period was uneventful and the patient was discharged from hospital four days after the operation. At follow-up, her menstrual cycle was regular, with no dysmenorrhoea. The final histopathology report revealed a benign submucosal leiomyoma.
Uterine inversion occurred when the uterus retracted to expel the submucosal myoma with its attachment to the fundus.
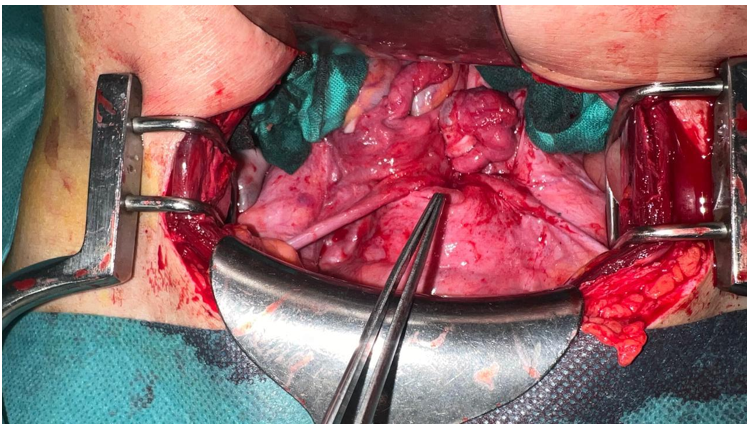
Figure 1: Per Operative Aspect of Uterine Inversion

Figure 2: Myomectomy Surgical Specimen
Discussion
Uterine inversion is an extremely rare complication. Apart from the puerperal period, there are no epidemiological data. These are sporadic cases [2]. Two conditions are necessary for uterine inversion to occur: uterine hypotonia and sufficient cervical dilatation. Several factors are involved in the pathophysiology of non-puerperal uterine inversion: the presence of a uterine tumour located preferentially on the uterine fundus; on a thin uterine wall; with a small tumour pedicle; rapid tumour growth; and cervical dilatation due to distension of the uterine cavity. Non-puerperal uterine inversion can also be classified as acute or chronic depending on its onset and course. The acute form is more dramatic and characterised by acute pelvic pain and haemorrhage, while the chronic form is insidious and characterised by pelvic discomfort, vaginal discharge and irregular abnormal uterine bleeding [3].
The aetiology found in 70 to 85% of cases, depending on the author, is submucosal myoma [4]. In 15 to 30% of cases, malignant tumours are involved, the most common of which are uterine sarcomas (leiomyosarcoma, embryonal rhabdomyosarcoma, endometrial stromal sarcoma). Depending on the severity, there are four degrees [4]: first degree: the uterine fundus is depressed into a ‘flask’ or cup; second degree: the inverted uterus passes through the external orifice of the cervix; third degree: the uterine body becomes intra-vaginal and may be completely externalized; fourth degree or total inversion: the vaginal walls participate in the inversion. Lewin et al. recommend the use of T2-weighted MRI to detect a U-shaped uterine cavity, a thickened and inverted uterine fundus on a sagittal image and a ‘bull's eye’ configuration on an axial image as indicative signs of uterine inversion [5].
Several approaches have been described in the literature: conservative treatment when reduction of uterine inversion is possible, mainly in cases of 1st or 2nd degree uterine inversion. Radical treatment is preferred if there is no desire to become pregnant, and is virtually indispensable in cases of 3rd and 4th degree uterine inversion [6].
Hysterectomy may then be performed vaginally, exposing the surgeon to technical difficulties due to changes in the usual anatomical landmarks, particularly in relation to the urinary excretory tracts (ureters and bladder). The abdominal route has also been described, but requires the inversion to be reduced and the uterus returned to the pelvic cavity. The combination of laparoscopy and the vaginal route already described by the Auber et al team [7] seems to be a good alternative for confirming the diagnosis, assessing the degree of ischaemia of the adnexa and vagina, and revascularizing the uterus laparoscopically by controlling the uterine pedicle from its origin. In the literature, uterine artery embolization is indicated in chronic non-puerperal uterine inversions, generally of the 2nd and 3rd degree, and in acute puerperal inversions reducible to conservative treatment.
Conclusion
Non-puerperal uterine inversion is a very rare condition. It is difficult to diagnose on the basis of clinical examination and ultrasound alone. Today, MRI has become the best examination not only for correcting the diagnosis, but also for contributing significantly to the aetiological assessment.
References
- Beringer RM., Patteril M. Puerperal uterine inversion and shock. Br J Anaesth. 2004;92(3):439–4. [PubMed.]
- Inversion utérine non puerpérale chronique: à propos d’un cas. Pan Afr Med J. 2018;31:231. [Ref.]
- Krenning RA., Dorr PJ., De Groot WH., et al. Inversion utérine non puerpérale. Rapport de cas. Br J Obstet Gynaecol. 1982;89:247–249. [PubMed.]
- Lupovitch A., Edwin R., Ruey C. Non-puerperal uterine inversion in association with uterine sarcoma: case report in a 26-year-old and review of the literature. Gynecol Oncol. 2005;97(3):938–41. [PubMed.]
- Lewin JS., Bryan PJ. Imagerie par résonance magnétique de l'inversion utérine. J Comput Assist Tomogr. 1989;13: 357–359. [PubMed.]
- Pelissier-Komorek A., Lucereau-Barbier M., Diab J., Gavillon N., Graesslin O. Acute non-puerperal uterine inversion the third degree. Gynécologie Obstétrique & Fertilité. 2013;41(2):130–2. [PubMed.]
- Auber M., Darwish B., Lefebure A., Ness J., Roman H. Management of nonpuerperal uterine inversion using a combined laparoscopic and vaginal approach. Am J Obstet Gynecol. 2011;204(6):e7. [PubMed.]