>Corresponding Author : Addi Salma
>Article Type : Case Report
>Volume : 5 | Issue : 11
>Received Date : 08 July, 2025
>Accepted Date : 21 July, 2025
>Published Date : 16 October, 2025
>DOI : https://doi.org/10.54289/JCRMH2500154
>Citation : Addi S, Chyate F, Fallah C, Boufettal H, Mahdaoui S, et al. (2025) Residual Micropapillary Carcinoma of the Breast after Neoadjuvant Treatment: a Rare Entity with a Poor Prognosis. J Case Rep Med Hist 5(11): doi https://doi.org/10.54289/JCRMH2500154
>Copyright : © 2025 Addi S, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Case Report | Open Access | Full Text
1Resident Physician, Department of Gynecology and Obstetrics at the Ibn Rochd University Hospital, Casablanca, Morocco
2Professor in the Department of Gynecology and Obstetrics at the Ibn Rochd University of Hospital in Casablanca Morocco
*Corresponding author: Salma Addi, Resident Physician, Department of Gynecology and Obstetrics, Ibno Rochd University Hospital, Casablanca, Morocco
Abstract
Micro-papillary carcinoma of the breast (MPBC) is a rare histological subtype, accounting for around 1-2% of invasive breast cancers. It is characterized by a distinctive inverted pseudopapillary architecture and a strong tendency to lymphovascular invasion and lymph node metastasis. Despite frequent expression of hormone receptors, it is associated with an unfavorable prognosis due to its aggressive behavior. Diagnosis is based on specific morphological and immunohistochemical criteria, and treatment follows the general principles of breast cancer, although a more aggressive approach is sometimes warranted. A better understanding of its biological characteristics could improve the management of this under-appreciated entity.
Keywords: Micro-papillary carcinoma, Breast cancer, Breast histology, Lymph node metastasis, Immunohistochemistry, Prognosis, Aggressive subtype
Abbreviations: MPBC: Micro-Papillary Breast Carcinoma, ACR: American College of Radiology, SBR: Scarff-Bloom-Richardson, HER2: Human Epidermal growth factor Receptor 2, FISH: Fluorescence In Situ Hybridization, CMPS: Carcinoma Micro-Papillary Subtype, PMSC: Papillary Micro-papillary Subtype Carcinoma, MSCC: Mammary Subtype Carcinoma
Introduction
Micro-papillary carcinoma of the breast (MPBC) is a rare histological entity representing approximately 0.9% to 2% of all invasive breast cancers. First described in 1993 by Siriaunkgul and Tavassoli [1], this subtype is characterized by a particular histological architecture reminiscent of inverted pseudopapillary formations, often associated with high clinical aggressiveness, a marked tendency to lymph node metastasis and an unfavorable course. Despite its rarity, recognition of this variant is essential because of its specific prognostic and therapeutic implications [2].
Case Report
This is a 43-year-old patient with no specific pathological history who presented for further management of a right breast neoplasm.
The history of the disease dates back 6 months, discovered by autopalpation of a mass.
Initial clinical examination revealed a 35×35 mm mass located in the superior-internal quadrant of the right breast, with no signs of inflammation or nipple discharge.
Initial echomammography revealed two contiguous nodules in the same quadrant, measuring 23×15 mm and 15×11 mm respectively, associated with a homolateral axillary adenopathy of 11 mm; the examination was graded ACR 5.
An ultrasound-guided biopsy of the lesion revealed a non-specific invasive breast carcinoma, grade SBR III, luminal B, HER2 score 2, with positive FISH confirmation.
Lymph node biopsy revealed a poorly differentiated carcinoma compatible with a breast origin.
The extension work-up revealed no abnormalities.
The patient received 6 courses of neoadjuvant chemotherapy (3 EC followed by 3 courses of docetaxel) combined with double HER2 blockade.
Post-chemotherapy clinical examination revealed induration opposite the upper quadrant junction, with no inflammatory signs or nipple discharge.
Post-chemotherapy ultrasonography showed a 14×20 mm lesion opposite the clip inserted during treatment (Figure 1).
The patient underwent a right mastectomy with axillary curage (Figure 2). Pathological analysis concluded that:
1. Right mastectomy: residual invasive breast carcinoma, micropapillary type confirmed by immunohistochemistry, measuring 3 cm long, with healthy margins. The nipple and its base were infiltrated. No Paget's disease of the nipple.
2. Axillary curage: Single lymph node metastasis (1 positive lymph node out of 10).
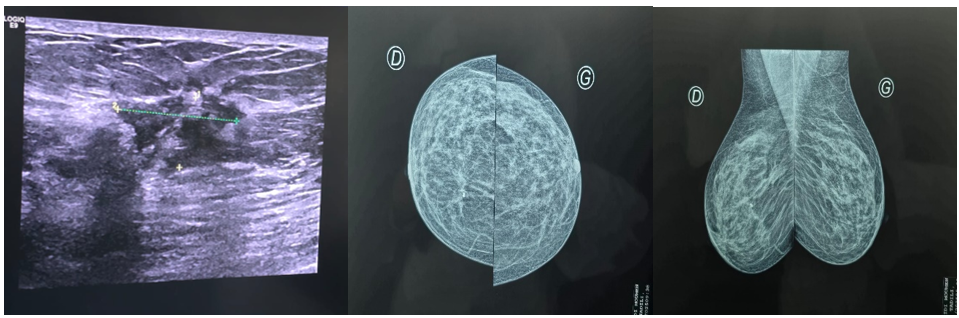
Figure 1: Ultramammography image of upper quadrant junction lesion

Figure 2: Right mastectomy specimen and axillary curage
Discussion
Micro-papillary carcinoma of the breast is characterized histologically by the presence of small tumoral structures forming compact clusters arranged in pseudopapillae without a fibrovascular axis, often surrounded by stromal clearances simulating lymphatic channels [1, 2]. This architectural pattern, reminiscent of micro-papillary carcinoma of the lung, has been associated with a high frequency of vascular emboli and lymph node metastases at diagnosis, sometimes reaching up to 75% of cases [3].
Immunohistochemically, CMPS generally expresses hormone receptors (RE+ in 70-90% of cases, RP+ in 50-80%), while HER2 expression varies from series to series [4]. The predominant molecular profile is luminal B, although cases of HER2-enriched or triple-negative subtypes have also been reported. Reverse marking of cell polarity by anti-EMA and MUC1 antibodies, localized at the outer pole of the cells, is a major diagnostic clue [2]. These features suggest an inverted epithelial phenotype favoring tumor dissemination.
Clinically, patients with PMSC often present with a palpable mass of moderate size, but the diagnosis may be delayed by an unspecific appearance on imaging [4]. The frequent association of PMSC with other histological types, notably non-specific infiltrating ductal carcinoma, can complicate the diagnosis. However, the micro-papillary component, even if a minority, retains an important prognostic weight [3, 5].
Treatment of SMC does not differ fundamentally from that of other invasive breast carcinomas. It is based on surgery, radiotherapy, hormone therapy and chemotherapy, depending on tumour and lymph node characteristics. However, because of the high risk of lymph-node dissemination and distant dissemination, some authors suggest a more aggressive therapeutic strategy, including complete axillary dissection even in the case of a positive sentinel node [3, 5].
The prognosis of MSCC is generally unfavourable, with a 5-year overall survival rate lower than that of ductal carcinomas of the same stage [5]. The presence of massive lymphovascular invasion, the high frequency of locoregional relapse and rapid progression to visceral metastases explain this unfavorable outcome. Nevertheless, early identification of this subtype and appropriate management can improve therapeutic prospects.
Conclusion
Micro-papillary carcinoma of the breast is a rare but aggressive histological subtype, recognized on the basis of specific morphological and immunohistochemical criteria. It is associated with a high metastatic risk and unfavourable prognosis, justifying optimized therapeutic management. A better understanding of its mechanisms of dissemination and molecular features could pave the way for new targeted strategies.
References
- Siriaunkgul S, Tavassoli FA. Invasive micropapillary carcinoma of the breast. Mod Pathol. 1993 Nov;6(6):660–2. [PubMed.]
- Walsh MM, Bleiweiss IJ. Invasive micropapillary carcinoma of the breast: eighty cases of an underrecognized entity. Hum Pathol. 2001 Jun;32(6): 583–9. [PubMed.]
- Chen AC, Paulino AC, Schwartz MR, et al. Prognostic markers for invasive micropapillary carcinoma of the breast: a population-based analysis. Clin Breast Cancer. 2013 Apr;13(2): 133–9. [PubMed.]
- Vingiani A, Maisonneuve P, Dell'Orto P, et al. The clinical relevance of micropapillary carcinoma of the breast: a case-control study. Histopathology. 2013 Aug;63(2): 217–24. [PubMed.]
- Magnoni F, Bianchi B, Pagan E, Corso G, Sala I, et al. Long-term outcome of invasive pure micropapillary breast cancer compared with invasive mixed micropapillary and invasive ductal breast cancer: a matched retrospective study. Breast Cancer Res Treat. 2024 Nov;208(2): 333–47. [PubMed.]