>Corresponding Author : Addi Salma
>Article Type : Case Report
>Volume : 5 | Issue : 11
>Received Date : 04 July, 2025
>Accepted Date : 15 July, 2025
>Published Date : 16 October, 2025
>DOI : https://doi.org/10.54289/JCRMH2500153
>Citation : Addi S, Zein M, Fallah C, Boufettal H, Mahdaoui S, et al. (2025) Adult Granulosa Cell Tumor of the Ovary: A Case Report and Literature Review. J Case Rep Med Hist 5(11): doi https://doi.org/10.54289/JCRMH2500153
>Copyright : © 2025 Addi S, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Case Report | Open Access | Full Text
1Resident Physician, Department of Gynecology and Obstetrics at the Ibn Rochd University Hospital, Casablanca, Morocco
2Professor in the Department of Gynecology and Obstetrics at the Ibn Rochd University of Hospital in Casablanca Morocco
*Corresponding author: Salma Addi, Resident Physician, Department of Gynecology and Obstetrics, Ibno Rochd University Hospital, Casablanca, Morocco
Abstract
Adult granulosa cell tumor is a rare sex cord-stromal tumor of the ovary, accounting for less than 5% of ovarian tumors [1]. It often progresses slowly and has an unpredictable malignant potential. We report the case of a postmenopausal woman presenting with a suspicious ovarian mass revealed by chronic pelvic pain. Histological examination confirmed an adult granulosa cell tumor. This case highlights the importance of multidisciplinary management and long-term follow-up.
Keywords: Granulosa Cell Tumor; Ovarian Tumor; Stromal Tumor; Gynecological Surgery; Histology
Introduction
Granulosa cell tumors belong to the group of sex cord-stromal tumors of the ovary. Two forms are distinguished: adult and juvenile, with the former being the most common. Diagnosis relies primarily on histology [1,2], often supported by immunohistochemistry. The prognosis is generally good, but the risk of late recurrence requires prolonged follow-up [1,3]. We present here a typical case of adult granulosa cell tumor in a postmenopausal woman, incidentally discovered during an evaluation for pelvic pain.
Case Report
A 51-year-old woman, married, with one child born by vaginal delivery, with no notable medical history and postmenopausal for one year, presented with chronic pelvic pain described as a sensation of heaviness, without associated digestive or urinary symptoms. Her general condition was preserved.
Gynecological examination was unremarkable.
Pelvic ultrasound revealed a normal-sized uterus with small myomas (the largest measuring 24 x 18 mm, FIGO 3), as well as a left ovary increased in volume with heterogeneous echotexture, measuring 62 x 46 mm (Figure 1).
Pelvic MRI showed a predominantly solid left ovarian mass measuring 67 x 54 x 53 mm, classified as ORADS 4, with an additional submucosal myoma measuring 20 x 21 mm (Figure 2). CA-125 level was 18.25 IU/mL.
Surgical exploration was performed, including left oophorectomy, omental biopsy, peritoneal biopsy, and peritoneal fluid sampling. The ovarian mass measured approximately 6 cm. No ascites or peritoneal carcinomatosis was observed.
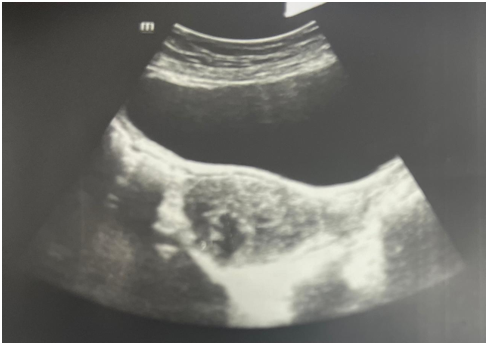
Figure 1: Ultrasound image showing an enlarged left ovary with heterogeneous echotexture, measuring 62x46 mm
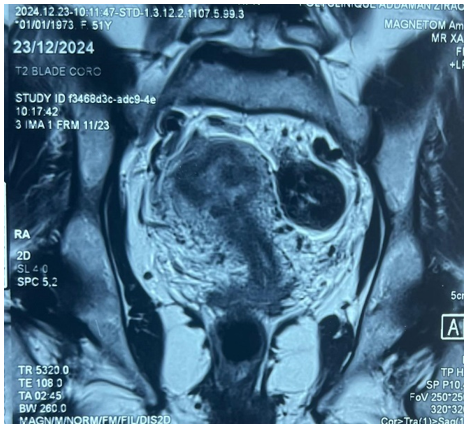
Figure 2: Frontal MRI view showing a predominantly solid left ovarian mass measuring 67x54x53 mm.
Histopathological Findings
- Left ovary: A solid tumor occupying the entire organ, showing cystic and hemorrhagic changes. Histological examination revealed a diffuse proliferation with cord-like and microfollicular structures. The cells were monomorphic, with oval nuclei and fine chromatin, and sometimes exhibited nuclear grooves. Mitotic index: 3 per 10 HPF. No capsular rupture was observed.
Conclusion: Morphological features consistent with an adult granulosa cell tumor.
- Omental and peritoneal biopsies: No evidence of malignant tumor proliferation; nonspecific inflammatory appearance.
Discussion
Granulosa cell tumors of the ovary are rare neoplasms, accounting for approximately 2 to 5% of all ovarian tumors [1,3]. They belong to the group of sex cord-stromal tumors and are classified into two histological subtypes: the adult type (95% of cases) and the juvenile type (5%). The adult subtype, as in our patient, primarily occurs in middle-aged or postmenopausal women, with a mean age at diagnosis between 50 and 55 years [1,4].
These tumors originate from granulosa cells of the follicle, which are involved in estrogen production. This explains the clinical symptoms related to hyperestrogenism, including metrorrhagia, endometrial hyperplasia, and even endometrial adenocarcinoma in 5 to 25% of cases [3]. Other clinical signs include mastodynia, menstrual disorders, or precocious puberty in the juvenile form. However, in 30 to 50% of cases, as in our patient, the presentation is nonspecific, consisting of pelvic pain or the incidental discovery of an ovarian mass.
Preoperative diagnosis is often challenging, as imaging does not allow for precise identification of the tumor. Ultrasound and MRI typically reveal a solid or mixed, unilateral ovarian mass without ascites or carcinomatosis, as observed in our patient. The ORADS 4 score indicates a suspicion of malignancy [2], though it is not specific. Tumor markers such as CA-125 may remain within normal ranges, as in this case, which is common in stromal tumors [3], unlike epithelial tumors.
Definitive diagnosis relies on histopathological examination. The typical pattern of adult granulosa cell tumors includes a diffuse, nodular, or microfollicular architecture, with Call-Exner bodies and nuclei resembling 'coffee beans' [1,4]. In our case, histology showed a monomorphic proliferation with compatible morphological characteristics. Ongoing immunohistochemical studies could confirm the diagnosis using markers such as inhibin α, calretinin, CD56, and the recently described FOXL2 (C134W) mutation, present in over 95% of cases [3].
Treatment is primarily surgical. In postmenopausal women, radical surgery including hysterectomy [2] and bilateral salpingo-oophorectomy is recommended. In our case, unilateral oophorectomy was performed along with surgical staging, including peritoneal and omental biopsies and peritoneal cytology. Most granulosa cell tumors are diagnosed at an early stage (FIGO stage I in 75 to 90% of cases), which is a favorable prognostic factor [2,4]. The absence of capsular rupture, malignant cells in cytology, and peritoneal carcinomatosis in our patient significantly reduces the risk of dissemination.
The overall prognosis is good, but the recurrence rate remains significant, ranging from 20 to 30% [1,3]. Recurrences may occur late, sometimes more than 10 or 20 years after initial treatment. This underscores the need for prolonged, if not lifelong, clinical and radiological follow-up. This includes regular clinical examinations, annual pelvic ultrasound, and if serum inhibin levels were initially measured, periodic monitoring as a marker of recurrence. In the event of recurrence, treatment is again based on surgery and may be complemented by chemotherapy or hormone therapy [2,3].
This case highlights the importance of multidisciplinary management combining accurate histological diagnosis, appropriate surgical treatment, and long-term follow-up to optimize prognosis and prevent late recurrence.
Conclusion
This case illustrates a typical presentation of adult granulosa cell tumor of the ovary, diagnosed after menopause and revealed by pelvic pain. Diagnosis is established through histological examination, and treatment is mainly surgical. Postoperative vigilance is essential due to the risk of late recurrence.
References
- Schumer ST., Cannistra SA. Granulosa cell tumor of the ovary. J Clin Oncol. 2003;21(6):1180-9. [PubMed.]
- Colombo N., Parma G., Zanagnolo V., Insinga A. Management of ovarian stromal cell tumors. J Clin Oncol. 2007;25(20):2944–51. [PubMed.]
- Kottarathil VD., Antony MA., Nair IR., Pavithran K. Recent advances in granulosa cell tumor ovary: A review. Indian J Surg Oncol. 2013;4(1):37–47. [PubMed.]
- Lee IH., Choi CH., Hong DG., et al. Clinicopathologic characteristics of granulosa cell tumors of the ovary. Yonsei Med J. 2011;52(5):906–12. [PubMed.]