>Corresponding Author : Addi Salma
>Article Type : Case Report
>Volume : 5 | Issue : 11
>Received Date : 04 July, 2025
>Accepted Date : 15 July, 2025
>Published Date : 16 October, 2025
>DOI : https://doi.org/10.54289/JCRMH2500152
>Citation : Addi S, Fallah C, Zein M, Boufettal H, Mahdaoui S, et al. (2025) Refractory Vulvar Bowen’s Disease: A Case Report and Literature Review. J Case Rep Med Hist 5(11): doi https://doi.org/10.54289/JCRMH2500152
>Copyright : © 2025 Addi S, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Case Report | Open Access | Full Text
1Resident Physician, Department of Gynecology and Obstetrics at the Ibn Rochd University Hospital, Casablanca, Morocco
2Professor in the Department of Gynecology and Obstetrics at the Ibn Rochd University of Hospital in Casablanca Morocco
*Corresponding author: Salma Addi, Resident Physician, Department of Gynecology and Obstetrics, Ibn Rochd University Hospital, Casablanca, Morocco
Abstract
Vulvar Bowen’s disease, a rare form of vulvar intraepithelial neoplasia (VIN III), represents a precancerous lesion mostly linked to high-risk human papillomavirus (HPV) infection. Diagnosis is often delayed due to non-specific clinical presentation mimicking benign dermatoses. We report the case of a 63-year-old woman with a chronic pruritic vulvar lesion initially treated unsuccessfully with topical corticosteroids. Biopsy confirmed HPV-associated Bowen-type VIN III. Topical treatment with 5-fluorouracil was ineffective, and complete surgical excision with clear margins was performed. This case highlights the importance of early histological diagnosis and tailored management to prevent progression to invasive carcinoma.
Keywords: Bowen’s Disease; VIN III; Vulva; Squamous Cell Carcinoma in Situ; 5-Fluorouracil; Surgical Excision; HPV; Vulvar Precancerous Lesion
Abbreviations: VIN: Vulvar Intraepithelial, HPV: Human Papillomavirus, FU: Fluorouracil
Introduction
Bowen’s disease is a form of intraepithelial squamous cell carcinoma, first described by John T. Bowen in 1912 [1]. When it affects the vulva, it falls within the spectrum of vulvar intraepithelial neoplasia (VIN), representing a non-invasive precancerous entity. It is frequently associated with persistent high-risk human papillomavirus (HPV) infection, particularly types 16 and 18 [2]. Clinical presentation may be misleading, resembling benign conditions such as lichen sclerosus, eczema, or psoriasis. Diagnosis is histological, and treatment varies depending on lesion extent, ranging from topical chemotherapy to surgical excision [3].
Case Report
We report the case of a 63-year-old woman who had menarche at 11, had been menopausal for 10 years, and had given birth to one child vaginally. She had no history of oral contraceptive use. Her medical history included type 2 diabetes managed with oral antidiabetics for 10 years, and a thyroidectomy for a benign multinodular goiter three years earlier, with ongoing levothyroxine therapy.
The disease began about a year earlier with the appearance of a pruritic vulvar lesion that gradually increased in size and was resistant to treatment with topical corticosteroids and antihistamines. Her general condition remained stable.
A pelvic ultrasound showed no abnormalities.
The patient consulted dermatology, where a vulvar biopsy was performed, revealing high-grade vulvar intraepithelial neoplasia (VIN III) of the Bowen type associated with HPV. Topical treatment with 5-fluorouracil (5-FU) was initiated without clinical improvement.
She was referred for surgical management. Clinical examination revealed a whitish nodular lesion with an irregular and indurated surface, painful to palpation, measuring 2 x 2 cm, located on the left paramedian aspect of the labia minora (Figure 1).
Complete surgical excision was performed (Figure 2). Histopathological analysis of the specimen revealed a VIN III corresponding to carcinoma in situ (Bowen type), measuring 2 cm in greatest dimension, with complete excision. Lateral margins showed VIN I of the flat condyloma type, without margin involvement. The postoperative course was uneventful, with no signs of recurrence at three-month follow-up.

Figure 1: Whitish nodular lesion with irregular and indurated surface, located on the left paramedian aspect of the labia minora.
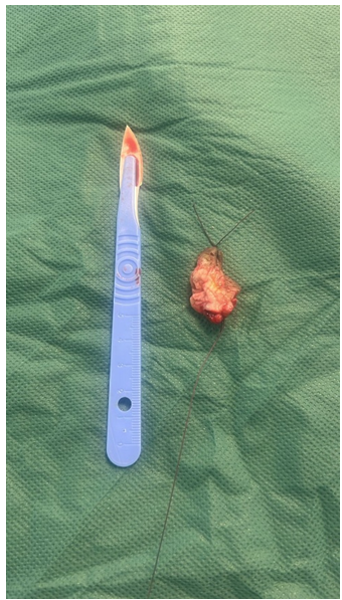
Figure 2: Surgical specimen after excision, showing the resected vulvar lesion beside a scalpel for scale.
Discussion
Vulvar Bowen’s disease is a rare form of high-grade vulvar intraepithelial neoplasia (VIN), classified among the precursors of invasive squamous cell carcinoma of the vulva. It is often confused with benign dermatoses such as lichen sclerosus or eczema, leading to delayed diagnosis and management [1]. It predominantly affects postmenopausal women and is strongly associated with persistent high-risk HPV infection, particularly type 16, which is implicated in about 80–90% of classic VIN cases (HPV-related) [2,3]. In our case, the patient was postmenopausal, and the histological findings were consistent with HPV-related VIN III, matching epidemiological data from the literature.
Clinically, Bowen’s disease manifests as an erythematous, keratotic, or verrucous lesion, sometimes pigmented, pruritic, or painful, with a slow progression. This clinical variability often leads to misdiagnoses. According to the series by Jones et al., over 60% of patients with VIN had previously been treated for benign vulvar dermatoses before the correct diagnosis [4].
Diagnosis relies on biopsy, which shows complete disruption of epithelial architecture, marked nuclear atypia, high mitotic activity, and absence of stromal invasion. Immunohistochemistry may help differentiate subtypes: diffuse p16 expression characterizes HPV-related forms, while p53 overexpression is more common in HPV-independent differentiated forms [5,6]. In our case, pathology revealed VIN III with peripheral foci of condylomatous VIN I, suggesting multifocal HPV infection.
Treatment depends on several factors: size, location, unifocal or multifocal character, patient’s age and comorbidities. Medical treatments like 5-fluorouracil (5-FU) or imiquimod can be considered first-line in limited lesions or in patients wishing to avoid surgery. However, efficacy varies. In van Seters et al.'s trial, imiquimod showed a complete response rate of 81% but with high incidence of local side effects [7]. 5-FU, though less commonly used today, remains an alternative but has lower efficacy and higher recurrence rates [8].
Surgery remains the gold standard for extensive, resistant, or suspicious lesions. Wide local excision allows for full histologic evaluation and ensures clean margins. In our case, 5-FU failure led to surgical excision, which confirmed the absence of invasive carcinoma and clear margins, thus ensuring local disease control.
The prognosis is favorable with early diagnosis and treatment, but recurrence is common, with rates ranging from 10% to 30% in various series [9]. Follow-up must include regular gynecological exams and evaluation of other anogenital sites potentially affected by multifocal HPV infection.
This case illustrates the diagnostic and therapeutic challenges of vulvar Bowen’s disease. It emphasizes the importance of early biopsy in any persistent atypical vulvar lesion and supports a personalized approach considering comorbidities, treatment tolerance, and surgical acceptability.
Conclusion
Vulvar Bowen’s disease is a rare but clinically significant condition, representing a form of high-grade intraepithelial neoplasia with high malignant transformation potential. This case highlights the diagnostic difficulties due to non-specific clinical presentation and the need for increased vigilance in persistent vulvar lesions unresponsive to standard treatments. Early biopsy is essential for diagnosis and management guidance.
When topical treatment fails, surgical excision is an effective therapeutic alternative, providing both treatment and full histologic assessment of the lesion. The prognosis is favorable with appropriate management, but regular follow-up is crucial due to the risk of local recurrence and associated HPV-induced lesions. This case underscores the importance of a multidisciplinary and individualized approach in managing vulvar intraepithelial neoplasias.
References
- Bornstein J., et al. The 2015 International Society for the Study of Vulvovaginal Disease (ISSVD) Terminology of Vulvar Squamous Intraepithelial Lesions. J Low Genit Tract Dis. 2016;20(1):11-14. [PubMed.]
- Joura EA., et al. Immunogenicity and safety of a nine-valent human papillomavirus vaccine in women aged 27–45 years compared to women 16–26 years of age: An open-label phase 3 study. Vaccine. 2021;39(20):2800–2809. [PubMed.]
- van de Nieuwenhof HP., et al. Vulvar squamous cell carcinoma development after diagnosis of VIN increases with age. Eur J Cancer. 2009;45(5):851–856. [PubMed.]
- Jones RW, Rowan DM, Stewart AW. Vulvar intraepithelial neoplasia: aspects of the natural history and outcome in 405 women. Obstet Gynecol. 2005;106(6):1319–1326. [PubMed.]
- Darragh TM., et al. The Lower Anogenital Squamous Terminology Standardization Project for HPV-Associated Lesions: background and consensus recommendations from the CAP and ASCCP. Arch Pathol Lab Med. 2012;136(10):1266–1297. [PubMed.]
- Eva L., et al. HPV-independent and HPV-associated vulvar squamous cell carcinoma: two different cancers. Int J Gynecol Cancer. 2022;32(9):1108–1114. [PubMed.]
- van Seters M., et al. Treatment of vulvar intraepithelial neoplasia with topical imiquimod. N Engl J Med. 2008;358(14):1465–1473. [PubMed.]
- Simões AC., et al. Treatment Interventions for Usual-Type Vulvar Intraepithelial Neoplasia: A Systematic Review and Meta-analysis. J Low Genit Tract Dis. 2025. [PubMed.]
- Lebreton M., et al. Vulvar intraepithelial neoplasia: Classification, epidemiology, diagnosis, and management. J Gynecol Obstet Hum Reprod. 2020;49(9):101801. [PubMed.]