>Corresponding Author : Hilalou Aymane
>Article Type : Case Report
>Volume : 5 | Issue : 10
>Received Date : 08 September, 2025
>Accepted Date : 18 September, 2025
>Published Date : 03 October, 2025
>DOI : https://doi.org/10.54289/JCRMH2500151
>Citation : Aymane H, Oumnia EB, Boufettal H, and Mahdaoui S. (2025) Iatrogenic Metallic Foreign Body in the Endopelvic Region: A Case Report. J Case Rep Med Hist 5(10): doi https://doi.org/10.54289/JCRMH2500151
>Copyright : © 2025 Aymane H, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Case Report | Open Access | Full Text
1Resident Physician, Department of Gynecology and Obstetrics at the Ibn Rochd University Hospital, Casablanca, Morocco
2Professor in the Department of Gynecology and Obstetrics at the Ibn Rochd University of Hospital in Casablanca Morocco
*Corresponding author: Hilalou Aymane, Resident Physician, Department of Gynecology and Obstetrics at the Ibn Rochd University Hospital, Casablanca, Morocco
Abstract
The retention of a medical device is a surgeon’s nightmare. It occurs in various situations, and its prevalence is estimated at 0.3 to 1 case per 1000 abdominal procedures [1]. Despite its low frequency, diagnostic difficulties and economic impact make this issue a pathology whose clinical forms and therapeutic options should be well known, and prevention strategies revisited [2]. We present the case of a 58-year-old woman operated on 28 years earlier for a ruptured ectopic pregnancy. Surgical exploration revealed multiple metallic foreign bodies in the pelvis, whose spatial arrangement suggested a surgical instrument similar to a Halstead clamp. Complete removal of these foreign bodies required multidisciplinary collaboration involving urology, visceral surgery, and neurosurgery teams, performed under intraoperative fluoroscopic control. Postoperative recovery was uneventful.
Abbreviations: BMI: Body Mass Index
Introduction
Iatrogenic surgical foreign body retention is a rare medical error but continues to occur. Feared by surgeons, its consequences can be severe for the patient [3].
Various types of foreign bodies can be involved during different procedures. Diagnosis can be made using various imaging techniques (ultrasound, X-ray, CT scan), but for some foreign bodies, such as textile fibers in gossypibomas, definitive diagnosis requires histological or cytological examination [4]. In light of a case of forgotten medical device, we review risk factors and recommendations to prevent such incidents, whose frequency is probably underestimated.
Case Report
The patient is a 58-year-old woman, mother of one child, previously operated 28 years ago by laparotomy for ruptured ectopic pregnancy, and 6 months ago for an anal fistula, presenting with pelvic pain. Symptoms began one year earlier with chronic, intermittent pelvic pain localized in the hypogastric region and radiating to the back. The pain occurred in crises with periods of remission, without associated urinary, digestive, or hemorrhagic signs. Clinical examination on admission found a patient in good general condition; gynecological and abdominal exams were normal. The rest of the examination was unremarkable.
Diagnostic workup started with a pelvic ultrasound, which was unremarkable, followed by a pelvic CT scan revealing metallic-density material near the bladder dome causing significant artifact. This material extended posteriorly in contact with the sacral bone (at the S3-S4 junction) outside the sacral foramina, with bone lysis surrounded by osteosclerotic reaction.
Preoperative pelvic X-rays (frontal and lateral) were performed to identify and localize the metallic foreign body. An exploratory laparotomy was done under general anesthesia with a Pfannenstiel transverse incision. Palpation revealed a metallic foreign body at the bladder dome. Urologists intervened and extracted half of the instrument intravesically. Exploration revealed a fistulous tract between the bladder and meso-sigmoid. Another fragment of the clamp was removed, followed by fistula closure and placement of two ureteral stents.
Intraoperative fluoroscopy identified two additional metallic fragments in pararectal positions. A visceral surgery team performed a Douglas pouch resection and dissection in an avascular presacral plane, allowing extraction of the remaining metallic fragments under radiological control. Postoperative course was uncomplicated.
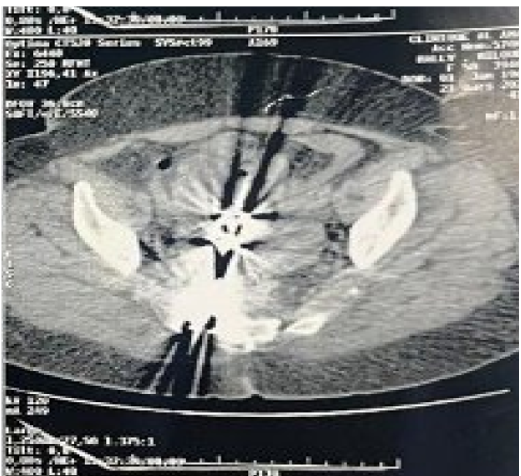
Figure 1: Pelvic CT scan showing an endopelvic gossypiboma
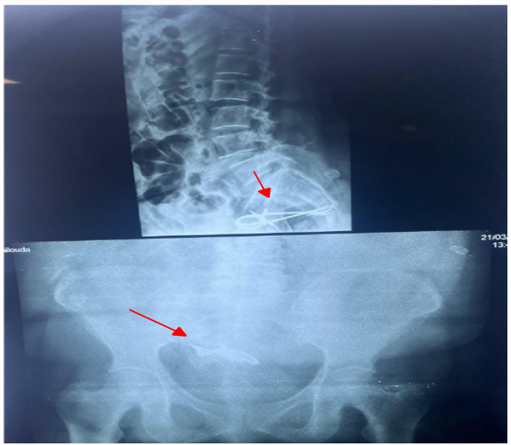
Figure 2: Preoperative pelvic X-ray localizing the metallic foreign body
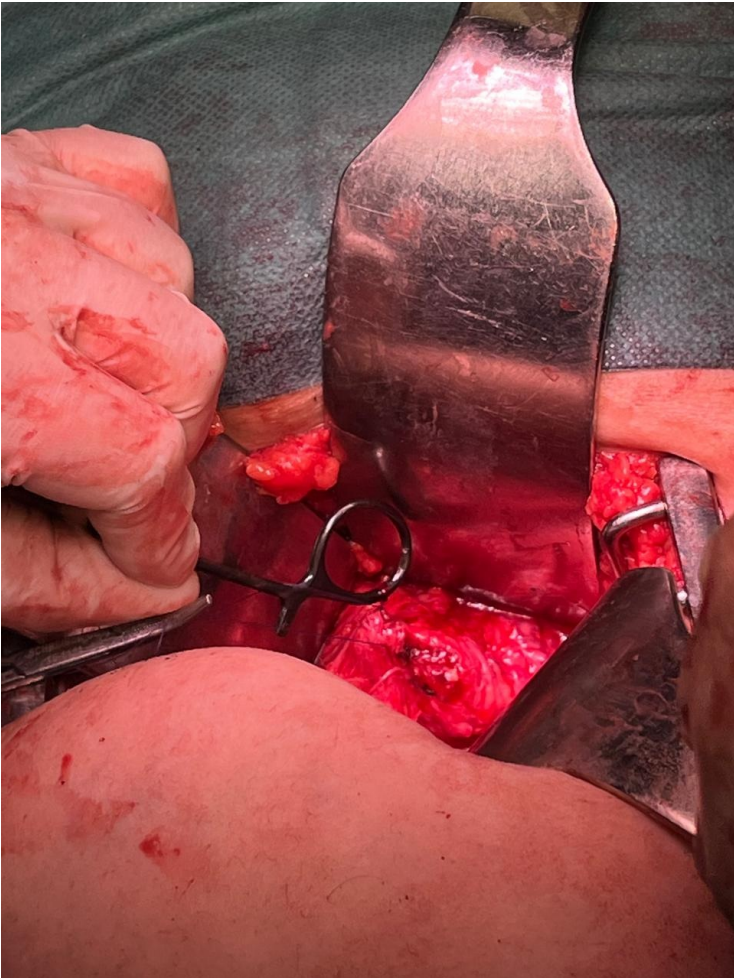
Figure 3: Extraction of half the intravesical clamp after cystostomy

Figure 4: Intraoperative fluoroscopy showing two metallic clamp fragments in the presacral space

Figure 5: Halstead clamp appearance after extraction
Discussion
Retention of a medical device during surgery is a serious event with potentially dramatic consequences for the patient. It also negatively impacts the surgeon, operating team, and healthcare facility. Beyond medico-legal implications, this incident causes frustration and embarrassment for healthcare professionals. Some insurance companies may refuse to cover costs related to reoperation for foreign body removal, highlighting the critical importance of prevention [5].
Epidemiologically, the prevalence of iatrogenic foreign body retention varies from 0.01% to 0.001% depending on studies. A 2003 New England Journal of Medicine study of malpractice claims in four UK hospitals estimated the incidence between 1 in 8,801 and 1 in 18,760 cases [6]. Another study found a similar postoperative detection rate of 1 in 14,000 [7]. The incidence is higher during abdominal surgeries (0.03% to 0.1%) [8].
Surgical sponges are the most frequently forgotten items, accounting for 50% to 69% of retained surgical foreign bodies in human medicine [9].
Because human error is inevitable, recommendations have been established to prevent or reduce these incidents. Identified risk factors include emergency surgeries, unexpected events or procedural changes, high body mass index (BMI), and prolonged operative time [8].
Clinical consequences of retained surgical foreign bodies vary and are often severe. Between 69% and 83% of patients require reoperation to remove the foreign body and manage complications such as fistulas, obstructions, and visceral perforations (22% of cases). Death has also been reported [6].
To prevent this rare but potentially serious intraoperative incident, the American College of Surgeons’ Perioperative Care Committee published recommendations in 2016 [10], including:
Strict adherence to standardized surgical item counting protocols
• Strict adherence to standardized surgical item counting protocols
• Systematic wound exploration before surgical site closure
• Use of radiopaque surgical sponges
• Maintaining an optimal operating environment to ensure concentration and precision
• Use of detection technologies such as radiography, radiofrequency, or barcode systems to confirm no items remain in the operative field
The operative report must document count results and actions taken if discrepancies occur. Careful planning of interventions is recommended, minimizing procedural changes or team switches during surgery. However, in life-threatening emergencies, these protocols may be relaxed or suspended [4].
Conclusion
Retention of a metallic foreign body in the pelvis is a rare but serious complication, reflecting a breach in operating room safety protocols. Such incidents may remain asymptomatic for years or present with chronic pelvic pain, recurrent infections, or nonspecific signs, delaying diagnosis. This underscores the importance of constant vigilance, rigorous counting of sponges, drapes, and surgical instruments, and a shared safety culture among the entire operating team. According to jurisprudence and medical law, discovery of a gossypiboma is recognized as a fault, implicating the surgeon’s responsibility.
References
- Health. Wolters Kluwer. 2025. [Ref.]
- Djoko I., Tchuenkam L., Mvondo P., Ndzie H., Boumal R., Bwelle G. Persistance d’un Textilome Abdominal Pendant 20 Ans: à Propos d’un Cas et Revue de la Littérature. 2023;1. [Ref.]
- Buy JN., Hubert C., Ghossain MA., Malbec L., Bethoux JP., Ecoiffier J. Computed tomography of retained abdominal sponges and towels. Gastrointest Radiol. 1989;14(1):41‒5. [PubMed.]
- Id H. Étude morphologique des corps étrangers d’origine chirurgicale utilisés en médecine vétérinaire. 2025 [Ref.]
- Conner R., Spruce L., Burlingame B., Denholm B., Ogg MJ., Van Wicklin SA., et al. Recommended Practices for Prevention of Retained Surgical Items. In: Perioperative Standards and Recommended Practices [Internet]. Association of peri Operative Registered Nurses. 2013;2025. [Ref.]
- Gawande AA., Studdert DM., Orav EJ., Brennan TA., Zinner MJ. Risk Factors for Retained Instruments and Sponges after Surgery. N Engl J Med. 2003;348(3):229‒35. [PubMed] [PubMed.]
- Egorova NN., Moskowitz A., Gelijns A., Weinberg A., Curty J., Rabin-Fastman B., et al. Managing the Prevention of Retained Surgical Instruments: What Is the Value of Counting? Ann Surg. 2008;247(1):13‒8. [PubMed.]
- Stawicki SPA., Moffatt-Bruce SD., Ahmed HM., Anderson HL., Balija TM., Bernescu I., et al. Retained Surgical Items: A Problem Yet to Be Solved. J Am Coll Surg. 2013;216(1):15‒22. [PubMed.]
- Gibbs VC., Coakley FD., Reines HD. Preventable Errors in the Operating Room: Retained Foreign Bodies after Surgery—Part I. Curr Probl Surg. 2007;44(5):281‒337. [PubMed.]
- Birolini DV., Rasslan S., Utiyama EM. Unintentionally retained foreign bodies after surgical procedures. Analysis of 4547 cases. Rev Colégio Bras Cir. 2016;43(1):12‒7. [PubMed.]