>Corresponding Author : Nouri Meriem
>Article Type : Case Report
>Volume : 5 | Issue : 12
>Received Date : 05 September, 2025
>Accepted Date : 16 September, 2025
>Published Date : 28 October, 2025
>DOI : https://doi.org/10.54289/JCRMH2500150
>Citation : Meriem N, Ezahraa TF, Isselmou NC, Younes B, Mustapha B, et al. (2025) Breast Tuberculosis in Men: A Rare Case Report. J Case Rep Med Hist 5(12): doi https://doi.org/10.54289/JCRMH2500150
>Copyright : © 2025 Meriem N, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Case Report | Open Access | Full Text
Mohamed VI center of oncology and gynecology; Obstetrics and Gynecology Department, University Hospital Ibn Rochd, Faculty of Medicine and Pharmacy, Hassan II University of Casablanca, Morocco
*Corresponding author: Nouri Meriem, Mohamed VI center of oncology and gynecology; Obstetrics and Gynecology Department, University Hospital Ibn Rochd, Faculty of Medicine and Pharmacy, Hassan II University of Casablanca, Morocco
Abstract
Breast tuberculosis accounts for 0.06 to 0.1% of extrapulmonary tuberculosis cases. It primarily affects women and remains exceptionally rare in men. We report a rare case of primary breast tuberculosis in a male patient. The patient was a 79-year-old man who presented with a chronic left breast mass and an overlying atrophic skin ulceration. Chest computed tomography (CT) revealed an enlarged and dense left mammary gland measuring 24 mm, with a soft tissue mass measuring 76.7 × 32.2 × 62 mm in projection of the 4th rib. A thick pleural effusion and a 5 mm lymph node in the left mammary chain were also noted. A trucut biopsy revealed fibroadipose tissue without evidence of normal or pathological mammary parenchyma. GeneXpert and acid-fast bacilli (AFB) tests performed on a swab from the ulceration were negative. The patient subsequently underwent surgical biopsy, which revealed caseous necrosis. Histopathological analysis showed epithelioid and giant-cell granulomatous inflammation, highly suggestive of tuberculous origin.
Keywords: Breast Tuberculosis, Primary, Male
Abbreviations: CT: Computed Tomography, AFB: Acid-Fast Bacilli, CNS: Central Nervous System
Introduction
Tuberculosis remains a major global public health concern [1]. Extrapulmonary forms account for 20–25% of all cases [2]. Breast involvement is rare, even in endemic regions, with a prevalence ranging from 0.06% to 0.1% [3]. First described by Cooper in 1829 as a “cold mammary tumor,” only 725 cases have been reported to date.
Breast tuberculosis predominantly affects women and is extremely uncommon in men [4]. While numerous cases have been documented in women, very few have been reported in men. Hence, this case adds to the limited literature on male breast tuberculosis.
Case Report
We present the case of a 79-year-old male, with no known history of tuberculosis contact, who presented to the Mohamed V Center for Onco-Gynecological Surgery at the University Hospital of Casablanca with a left breast mass.
Symptoms began 9 months earlier with a painless left breast swelling, without fever, cough, anorexia, or weight loss. One month later, a painful and inflamed ulceration developed over the mass (Figure 1). Breast ultrasound revealed a retro-areolar hypoechoic heterogeneous tissue mass with necrotic areas, measuring 78 × 40 mm, with irregular borders and contact with the chest wall, appearing suspicious with local wall infiltration. No axillary lymphadenopathy was detected. BI-RADS 5 was assigned (Figure 2).
Chest CT showed hypertrophy and densification of the left mammary gland (24 mm), with a soft tissue mass measuring 76.7 × 32.2 × 62 mm projecting over the 4th rib, which appeared slightly demineralized near the chondrocostal junction. Mediastinal fat infiltration and centimeter- to subcentimeter-sized lymph nodes were identified, the largest in Barety’s space. A thick pleural effusion and a 5 mm left mammary chain lymph node were noted. The pleura appeared thickened (8.1 mm), slightly hyperdense. Lung window analysis showed peribronchial micronodules in the upper lobe and apical segment of the right lung, with bilateral interstitial involvement and additional micronodules in the left lung (Figure 3). A tissue biopsy was performed on fatty and fibrous tissue. Absence of normal or pathological breast parenchyma. the GeneXpert and the search for acid-fast bacilli (AFB) performed on the ulceration swab were negative.
The patient had benefited from a surgical biopsy with an aspect of caseum at exploration (Figure 4). Result Anapath was in favor of an epithelial-giganto-cellular granulomatous lesion primarily suggestive of a tubercular origin.

Figure 1: An inflammatory and ulcerated mass measuring 4 cm located in the lower inner quadrant of the left breast.
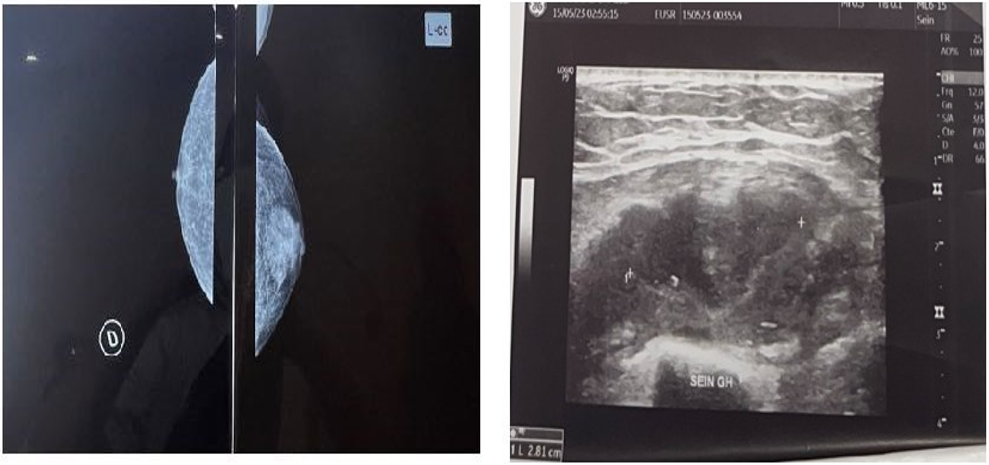
Figure 2: Breast ultrasound showing a suspicious 78 mm mass, classified as ACR 5.

Figure 3: Axial CT scan showing a left breast mass with a maximum diameter of 76.7 mm.
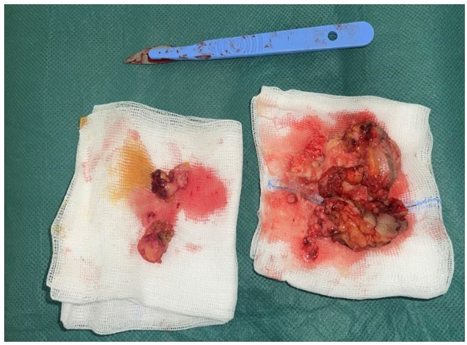
Figure 4: Surgical specimen: excision of the breast mass.
Discussion
Breast tuberculosis is among the most unusual of tuberculosis extra-pulmonary (0.1%), and about 4.5% of breast tumors [5]. It commonly affects young women (95% of cases) [1]. It rarely affects men, and the literature reports…very few isolated clinical cases. Tuberculous breast involvement is most often secondary to a pulmonary tuberculosis (37%) or extra-pulmonary (7.6%) and the pathway of contamination is either lymphatic from a thoracic focus or abdominal, either direct from a costal focus, chondrocostal, or sterno- clavicular [6]. In our context, the pleural focus seems to be the focus primitive. In humans, the first case was described in 1927 and until 2017, that is 90 years later, only 26 cases were reported in the literature including 4 cases in Africa [7]. Due to this rarity, human breast tuberculosis is little known and therefore easily confused with other differential diagnoses should include breast carcinoma and gynecomastia or abscess to pyogen, non-tuberculous granulomatous mamopathy, the mamopathy atypical mycobacterial, plasmocellular mastitis [8]. This was the case in our patient who, for a hypothesis of a malignant breast tumor.
A recent study had highlighted the polymorphic nature of tuberculosis mammary in men. The clinical presentation of the disease is poorly described in the literature, and important clinical elements are not reported uniformly or at all. The combination of signs and specific symptoms, the challenges of diagnosing tuberculosis mammary, lead to a significant delay in diagnosis: the median delay in the diagnosis was 10 months in our observation [7]. Classical systemic symptoms such as fever or general malaise are frequently absent (21.4%) in breast TB [4]. Our patient presented with a left breast mass and mild ulceration, without systemic symptoms or any other warning signs.
Although both breasts may be affected with equal frequency, bilateral forms occur in only 3% of cases [9]. Axillary adenopathies are found in 75% of cases, mobiles can evolve towards the fistulisation [10]. Mammography is not a decisive contribution because most of the images are malignant in appearance. Ultrasound usually reveals a hypoechoic mass in 60% of cases [11]. CT and MRI assess the extension towards the chest wall and explore the pulmonary parenchyma in search of an associated pulmonary form; can provide useful information, in particular about the extent of the disease. However, none of these results of image is not specific to breast tuberculosis. Tuberculosis coexistent pulmonary may be suggestive of mammary tuberculosis, but the active disease is often absent
Cytopuncation rarely discovers epithelioid cells or bacilli of Koch as is the case of our patient, and she can show cells dyscaryotics in favor of a carcinoma. The new techniques (the culture on liquid medium Bactec, or by PCR improve the diagnosis) [12]. The research yield of BAAR in pathological products is very heterogeneous. It varies between 8.7 and 68.7% depending on the studies [13]. In the series of Kilic et al., the positivity of PCR alone was 50%.
The diagnostic accuracy is achieved by conducting bacteriological or histological examination on the biopsy samples, which demonstrate an epithelial-giganto-cellular granuloma with caseous necrosis [5,10]. The main differential diagnosis arises with breast cancer. Even if coexistence of breast cancer and tuberculosis has rarely been described, we think that the postoperative histological study of breast tissue is necessary in order to to eliminate an associated carcinoma.
Overall, breast tuberculosis seems to have a good prognosis, although no specific guidelines are available for the treatment of breast tuberculosis, whether in men or women. The optimal duration of the treatment is not clear and the objective criteria Evaluating the response is lacking [4]. A standard anti-TB regimen (phase intensive of two months to four medications followed by a phase of continuation of four months at two medications), often accompanied (or preceded) by an incision and drainage or excision of the mass, seems obtain satisfactory answers. Twelve subjects received a treatment surgical. However, it is not possible to determine to what extent these procedures were carried out as a first step towards the establishment of a diagnosis, rather than being part of the treatment plan. The protocol recommended by OMS should be followed when treating tuberculosis extrapulmonary [14,15].
Adults with EPTB (Drug-Susceptible TB): Standard regimen: Adults are eligible for the 6month regimen — 2 months of isoniazid, rifampicin, pyrazinamide, and ethambutol (2HRZE), followed by 4 months of isoniazid and rifampicin (4HR), as for pulmonary TB. Exceptions include EPTB of the central nervous system (CNS), bones, or joints, for which many experts suggest extending therapy to 9–12 months.
Conclusion
Breast tuberculosis in men is a rarely reported condition, even in countries with a high TB burden. Due to undefined clinical characteristics, diagnosis is challenging and often delayed. The most common presentation includes a mass with skin inflammation, pain, and axillary lymphadenopathy. Diagnosis relies on FNAC, culture, and biopsy. No standardized treatment protocols exist, but standard anti-tuberculosis regimens appear effective, with generally good prognosis.
Conflict of Interest: The authors declare that they have no conflict of interest.
Guarantor of Submission: The corresponding author is the guarantor of submission.
References
- WHO. Global tuberculosis report 2018. World Health Organisation. 2019. [Ref.]
- Mjid M., Cherif J., Salah NB., Toujani S., Ouahchi Y., Zakhama H., et al. Épidémiologie de la tuberculose. Rev Pneumol Clin. 2014;71(2‒3):67‒72. [Ref.]
- Bouhout T., Serji B., Egyir B., El Amri B., Bouhout I., Soufi M., et al. Tuberculose mammaire:à propos d’un cas. Pan Afr Med J. 2017;28:183. [Ref.]
- Rajagopala S., Agarwal R. Tubercular mastitis in men:case report and systematic review. Am J Med. 2008;121:539‒44. [PubMed.]
- Kumar M., Chand G., Nag VL., Maurya AK., Rao RN., et al. Breast tuberculosis in immunocompetent patients at tertiary care center:a case series. J Res Med Sci. 2012;17:199‒202. [PubMed.]
- Rakoto‒Ratsimba HN., Samison LH., Razafimahandry HJ., Rako-totiana AF., Imbiki Z., Ranaivozanany A. Two cases of breast tuberculosis in Madagascar. Med Trop. 2005;65:355‒8. [PubMed.]
- Quaglio G., Pizzol D., Bortolani A., Manenti F., Isaakidis P., Putoto G., et al. Breast tuberculosis in men:a systematic review. PLoS One. 2018;13(4):e0194766. [Ref.]
- Bani‒Hani KE., Yaghan RJ., Matalka II., Mazahreh TS. Tuberculosis mastitis:a disease not to be forgotten. Int J Tuberc Lung Dis. 2005;9:920‒5. [PubMed.]
- Morsad F., Ghazli M., Boumzgou K., Abbassi H., El Kerroumi M., Matar N., et al. Tuberculose mammaire. J Gynecol Obstet Biol Reprod. 2001;30:331. [Ref.]
- El Mrabet F., Ferhati D., Amenssag L., El Idrissi F., Erchidi I., Melhouf A., et al. Breast tuberculosis. Med Trop. 2002;62:77‒80. [PubMed.]
- Kachewar S., Sankaye S. Primary tubercular mastopathy. Aus‒ tralas Med J. 2012;5:436‒9. [PubMed.]
- Thompson KS., Donzelli J., Jensen J., Pachucki C., Eng AM., Reyes CV. Breast and cutaneous mycobacteriosis:diagnosis by fine‒needle aspiration biopsy. Diagn Cytopathol. 1997;17:45-9. [PubMed.]
- Kilic MO., Saglam C., Agca FD., Terzioglu SG. Clinical., diagnostic and therapeutic management of patients with breast tuberculosis:analysis of 46 Cases. Kaohsiung J Med Sci. 2016;32(1):27‒31. [PubMed.]
- WHO Consolidated Guidelines on Tuberculosis. Module 4:Treatment; – DrugSusceptible TB Treatment. 2022 [Ref.]
- Geneva. World Health Organization. 2022. [Ref.]