>Corresponding Author : Sahel Imane
>Article Type : Case Report
>Volume : 5 | Issue : 9
>Received Date : 27 July, 2025
>Accepted Date : 07 August, 2025
>Published Date : 11 August, 2025
>DOI : https://doi.org/10.54289/JCRMH2500143
>Citation : Imane S, Ezahraa TF, Mrida M, Benchrif Y, Ennachit S, et al. (2025) Phyllodes Tumors of the Breast: About 34 Cases. J Case Rep Med Hist 5(9): doi https://doi.org/10.54289/JCRMH2500143
>Copyright : © 2025 Imane S, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Case Report | Open Access | Full Text
1Resident Physician, Department of Gynecology and Obstetrics, at Ibno Rochd University Hospital, Casablanca, Morocco
2Professor in the Department of Gynecology and Obstetrics at the Ibno Rochd University Hospital in Casablanca, Morocco
*Corresponding author: Sahel Imane, Resident Physician, Department of Gynecology and Obstetrics, Ibno Rochd University Hospital, Casablanca, Morocco
Abstract
Phyllodes tumors of the breast are rare fibroepithelial tumors. They are the subject of Controversy, particularly concerning terminology, histological classification and Treatment. The aim of this study is to highlight the epidemiological, clinical, paraclinical, therapeutic and prognostic features of these tumors.
Patients and methods: This was a retrospective study of cases of phyllodes tumours Collected in the gynaecological-mammary surgery department of CHU Ibn Rochd, Casablanca, over a 6-year period.
Results: Thirty-four patients were included in our study. The mean age was 30.2 years. A history of fibroadenoma was found in 20.58%. The mean tumor size was 7.3 cm. Diagnosis was based on breast ultrasound, with or without mammography depending on the patient’s age, and micro biopsy. Treatment consisted of lumpectomy in 76.47% of Cases. Grade III was found in 14.7% of cases. Eight patients had non-healthy resection Margins, 6 of whom underwent revision surgery. After 3 years and 3 months, there were Two cases of metastatic recurrence.
Discussion: Phyllodes tumor of the breast is a rare entity. In our series, one of the Particularities is that it affects younger women in comparison with the literature. In the Majority of cases, it is benign, but histological examination must be meticulous in order to eliminate malignant forms. In benign forms, a wide lumpectomy with healthy Margins allows a favorable evolution with a very low risk of local recurrence. On the Other hand, in borderline and especially malignant forms, mastectomy seems to be Necessary in the majority of cases, along with adjuvant radiotherapy, to reduce the risk of local and metastatic recurrence.
Conclusion: The frequency of benign forms should not blind us to the risk of malignant or even metastatic recurrence. This underlines the importance of correct initial Management.
Keywords: Phyllodes tumor; Breast; Clinical features; Prognosis; Surgery
Introduction
Phyllodes breast tumors (TPS) are biphasic tumors consisting of a connective stromal Component and a foliaceous epithelial component (“phyllos” means “leaf” in Greek) [1]. These are rare tumors, accounting for 0.3 to 4% of female breast tumors [2]. However, they have two mains.
The first is that TPS encompasses a spectrum of pathologies ranging from benign tumors or phyllodes fibroadenomas to phyllodes carcinosarcomas.
WHO has distinguished three categories of GST: benign, borderline and malignant [3]. The second particularity is that all these tumors, whatever their grade, have a risk of local and metastatic evolution. This underscores the importance of understanding this entity, especially as it affects young patients with age extremes ranging from 13 to 55 years. The aim of this work is to review current diagnostic and therapeutic strategies for phyllodes tumors, while presenting our experience in the gynecological-mammary surgery department at CHU Ibn Rochd in Casablanca from 2015 to 2020.
Patients and methods
This was a retrospective study from 2015 to 2020, at the IBN ROCHD University Hospital in Casablanca, involving 34 patients. The aim is to highlight the epidemiological, clinical, paraclinical, therapeutic and prognostic features of these tumors. The study is based on the records of patients treated for phyllodes tumors of the breast. Diagnosis was established by anatomopathological examination of the surgical specimen. Patients underwent surgery in the gynecological-mammary surgery department of Ibn Rochd Hospital, Casablanca. Surgical specimens were analyzed in the anatomopathology laboratory of the same hospital.
Results
Over the study period, 34 cases of phyllodes tumours were identified, representing a frequency of 0.3% of breast tumours treated in our hospital. Patients ranged in age from 16 to 57 years at diagnosis. The mean age was 30.2 years. The majority of our patients were nulliparous, with a frequency of 67.6%. A history of fibroadenoma of the breast was found in seven cases, and two patients had a family history of breast cancer. The average consultation time was 3.8 months. The mean tumour size was 7.3cm. These tumors occupied the whole breast, with inflammatory signs opposite in five cases, i.e. a frequency of 14.7% (figure 1), and 2 patients had mobile homolateral axillary adenopathies.

Figure 1: Clinical appearance of a grade III phyllodes tumour
20 patients underwent mammography, a frequency of 58.82%. Mammography revealed A hyperdense, well-limited opacity without microcalcifications. Ultrasound was Performed in all patients, revealing a rounded, lobulated, hypoechoic formation, Heterogeneous in all cases. Diagnostic confirmation was histological by micro biopsy in 24 cases (70.58%), Revealing 13 benign GSTs, 8 borderline GSTs and 3 breast sarcomas. Micro biopsy was Positive for adenofibromas in 5 patients, and revealed no specific lesion in two, so it Was decided to complete the diagnosis with an extemporaneous examination. In favor of adenofibroma.
Two patients underwent immediate lumpectomy outside our facility. Histological examination revealed a benign GST in the young girl and a breast sarcoma in the second 41-year-old patient.
One patient had an 18 cm tumour with inflammatory signs, having had a surgical biopsy Objectifying a breast sarcoma.
A total of 21 cases of grade 1 phyllodes (61.67%), 8 cases of grade 2 phyllodes (23.52%) And 5 cases of grade 3 phyllodes (14.7%) were identified. With the exception of one patient with metastatic breast sarcoma, for whom palliative Treatment was recommended, all other patients underwent surgery. Twenty-six Underwent extended lumpectomy. Seven patients underwent total mastectomy. In two Patients, mastectomy was combined with removal of palpable axillary adenopathy, 3 patients underwent breast reconstruction using a dorsalis major flap. of the 26 Patients who underwent wide lumpectomy, 17 benefited from remodelling, and clips Were used in 3 patients.
Histological study of the definitive resection specimen showed 20 cases of grade I GST, 9 cases of grade II GST and 4 cases of grade III GST.
Adenectomies revealed no tumour extension of the 20 patients who underwent wide lumpectomy for grade 1 GST, the margins came Back unhealthy in 6 cases, hence the indication for tumour bed revision. One patient Refused revision and was lost to follow-up. She consulted us after 15 months, and we Noted no clinical or radiological recurrence at the tumour site of the 20 patients who underwent wide lumpectomy for grade 2 GST, two had Unhealthy margins and refused mastectomy.
All patients who underwent mastectomy (grade II: 3 cases, grade III: 4 cases) had Histologically healthy margins.
All patients with a grade III phyllodes tumour underwent mastectomy. Mastectomy followed by prophylactic chest wall irradiation, no axillary or internal No axillary or internal mammary chain irradiation was performed. Radiotherapy was Well tolerated in all patients.
Palliative FAC chemotherapy (5-fluorouracil, adriamycin, cyclophospamide) was given to the patient with pulmonary metastasis. At a mean follow-up of 3 years and 3 Months (4 months-76 months), two tumours recurred locally, with an enormous mass Taking up the whole breast. These patients underwent lumpectomy for grade II GST With unhealthy margins and refused revision. Recurrence was noted within 12 months and 8 months with the same histological same histological aspect with pulmonary metastases. They received adjuvant Radiotherapy (15 sessions at 42 Gy). Both patients died. The remaining patients had Good locoregional control.
Discussion
Breast phyllodes represent less than 1% of breast tumors and 2.5% of fibroepithelial Tumors, which also include adenofibromas [4]. In our series, the rate was 0.3%. They Occur in women of all ages, with a peak between 40 and 50 years of age, i.e. on average Around ten years later than a fibroadenoma [5]. In our study, the mean age of onset Was 26 years. The tumour occurs most frequently in nulliparous patients [6], as was the Case in our study. Macroscopically, GSTs vary in size, up to 40 cm. In our series, tumor Size ranged from 2 cm to 20 cm, with an average of 7.3 cm.
The study by Yilmaz et al. [7], based on mammograms of 31 patients, found significant hyper density in phyllodes tumours compared with adjacent mammary parenchyma. In Our series, 35.29% of phyllodes tumours were classified as ACR4 mammography. Ultrasonography typically reveals a hypoechoic, oval-polylobed image, sometimes with Areas of cystization; there are no arguments pointing to a malignant appearance, but a Lobulated appearance should prompt micro biopsy. [8,9]. Color-coded pulsed Doppler Shows harmonious hypervascularization, predominantly around the lesion, and a high Resistance index [10].
In cytology, it is often easier to differentiate a benign GST from a malignant one than to Separate a GST from an adenofibroma *7+. Many authors feel that cytology is not Sufficient for the diagnosis of GST [11] since the diagnosis of GST is based on the Demonstration of a specific architectural appearance. In our series, no patient Underwent needle cytopuncture.
The histological diagnosis of benign phyllodes can only be made on the lumpectomy Specimen, due to the heterogeneous nature of these tumours. Micro biopsies, although often correlated with lumpectomy, may have focused on less typical areas [12]. Micro biopsy was performed in 91.17% of cases and concluded to be a phyllodes tumor in 70.58% of cases. For some authors, intraoperative extemporaneous examination is unreliable because of the difficulty of differentiating benign PT from adenofibromas. Moreover, the Sarcomatous elements of PT may be mistaken for undifferentiated carcinomas requiring Untimely radical treatment [13]. Extemporaneous examination was carried out in three Patients, but it was only on definitive examination that the diagnosis of TPS was Accepted. Most authors agree on the need for wide surgery, with healthy margins as far as possible, Given the major impact on local recurrence. In two major studies, after conservative Surgery, ten-year relapse rates of 7-13% were observed for pure benign forms [14,15]. For borderline or malignant tumors, radical treatment significantly reduces local recurrence rates. In the case of borderline or malignant tumours, radical treatment significantly reduces Local recurrence rates, sometimes with a benefit in terms of overall survival.An immediate mastectomy is indicated for large tumours over 5 cm in size, and for Grade 3 tumours.For some authors, if tumour size allows conservative surgery with a sufficient margin (at least 1 cm) and a good aesthetic result, there is no reason to systematically propose mastectomy for malignant phyllodes tumours [16]. The results of the main studies are presented in (Table 1).
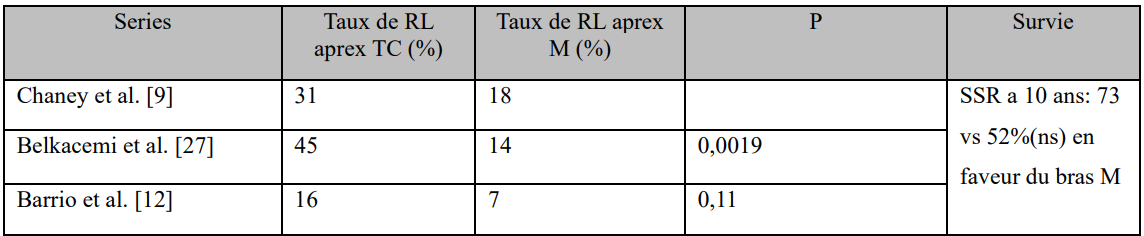
Table 1: Impact of type of surgery on relapse rate: borderline and malignant forms.
LR: local relapse; CT: conservative treatment; M: mastectomy; RSR: recurrence-free survival.
Whatever the type of surgery chosen, the majority of authors [16,17] consider that There is no indication for axillary lymph node dissection, due to the low risk of invasion. Indeed, 20% of axillary nodules are found on clinical examinations in association with a phyllodes tumor. Only 5% are histologically metastatic.
Many teams recommend adjuvant radiotherapy after conservative treatment, especially if the margins are invaded [18-20]. After mastectomy, it is recommended for tumors larger than 5 cm and for high-grade tumors. The usual dose is 60 Gy. [21,22]. In the neoadjuvant setting, chemotherapy does not appear to offer any benefit, due to low chemosensitivity and the fact that the majority of breast sarcomas are operable from the outset [18]. Chemotherapy could therefore be discussed for high-grade breast sarcomas larger than 5 cm or with incomplete excision [23]. Given the very poor prognosis of these tumors and their early metastatic potential, it seems logical to systematically discuss a anthracycline-based adjuvant chemotherapy.
The rate of local recurrence of TPS ranges from 10% to 40% in most series. The average is 15%. Local recurrence seems to be related to the initial surgery and should be considered a treatment failure. It is not clear what flaws in the surgical management may explain the recurrence, but the surgical margin has been shown to be the only factor predictive of local recurrence. Indeed, the risk of local recurrence is generally low with excisional margins exceeding 1 cm*10, [24].
In most patients, local recurrence is isolated and does not correlate with the risk of developing distant metastases [10]. In our series, there was no isolated local recurrence. This may be explained by the fact that we ensured margins greater than 10 mm, with Revision surgery in all cases where satisfactory margins were not obtained, except in the Case of the two patients who refused revision.
The risk of metastasis in breast phyllodes is 10%. The majority of distant metastases Develop without evidence of local recurrence. Remissions rarely exceed 6 months, and Death occurs less than a year later [24,25]. In our series, two patients presented with Pulmonary metastatic recurrence, and the prognosis was poor in both cases. Mortality rates vary from 3% to 12% depending on the study [26]. The study by Pandey et al. [27] involving 37 patients, shows that the survival rate is dependent on the surgical Margins of exeresis. Surgical margins. Taken together, these studies show that the main prognostic factor in Terms of local recurrence, metastatic spread and survival is the surgical margins of the Surgical specimen [28]. Tumour size (5 cm) is also a negative factor [27] as is stromal Infiltration at the time ofAnalysis of the surgical specimen [29]. Patients should be monitored clinically every 6 months for the first two years (risk of Recurrence is highest in the first two years), and then annually. Patients should be Advised to have their breasts examined regularly, and to seek medical advice if any abnormalities are detected [10].
Conclusion
Phyllodes tumour is a rare tumour. A wide lumpectomy with 10 mm margins remains the reference treatment in benign forms. For sarcomas, treatment is most often based on mastectomy without lymph node dissection, given the exceptional axillary invasion. The histological type associated with Type of excision (complete or incomplete) and stromal proliferation determines Prognosis. Progression is marked by the potential for local and/or metastatic relapses, particularly in the lung. Adjuvant radiotherapy is reserved for large, malignant breast Phyllodes tumors. Chemotherapy seems to have an ill-defined place.
Ethics approval: The requirement for informed consent was waived by the Ethics Committee.
References
- Lakhani SR., Ellis IO., Schnitt SJ., Tan PH., van de Vijver MJ (Eds.). Who Classifi cation of Tumors of the breast. Lyon: IARC 2012. [Ref.]
- Mangi AA., Smith BL., Gad MA. Surgical management of phyllodes tumors. Arch Surg. 1999;134(5):487–93. [PubMed.]
- World Health Organization, 2nd ed. Histologic typing of breast tumors, 2. Geneva, Switzerland: World Health Organization; 1981;22. [Ref.]
- Tavassoli FA., Devilee P. Pathology and genetics of tumors of the breast and female Genital organs. World Health Organization Classification of tumors. Lyon: IARC Press. 2003. [Ref.]
- Keelan PA., Myers JL., Wold LE., Katzmann JA., Gibney DJ. Phyllodes tumor: Clinicopathologic review of 60 patients and flowcytometric analysis in 30 patients. Hum Pathol. 1992;23(9):1048–54. [PubMed.]
- T Bouhafa., O Masbaha., I Bekkouch., S Afqir., N Mellas., N Ismaili., et al. Breast phyllodes tumors About 53 cases. Cancer Radiotherapy. 2009;13(2):85–91. [PubMed.]
- Yilmaz E., Sal S., Lebe B. Differentiation of phyllodes tumors versus fibroadenomas. Acta Radiol 2002;43(1):34–9. [PubMed.]
- J M Feder., E S de Paredes., J P Hogge., and J J Wilken. “Unusual breast lesions: Radiologic–pathologic correlation,” Radiographics. 1999;S11– S26. [Ref.]
- C Cole Beuglet., R Soriano., and A B Kurtz. “Ultrasound, X–ray mammography and Histopathology of cystosarcoma phylloides,” Radiology. 1983;146(2):481–486. [Ref.]
- Shashi Prakash Mishra., Satyendra Kumar Tiwary., Manjaree Mishra., and Ajay Kumar Khanna. Phyllodes Tumor of Breast: A Review Article. Hindawi Publishing Corporation ISRN Surgery. 2013;361469. [PubMed.]
- Petrek JA. Phyllodes tumors. Diseases of the breast. 2nd ed. Philadelphia: LippincottWilliams and Wilkins; 2000;669–75. [Ref.]
- Puay–Hoon Tan., Thiyagarajan Jayabaskar., Khoon–Leong Chuah., Hwei–Yee Lee., Yen Tan., Maryam Hilmy., et al. Phyllodes Tumors of the Breast. The Role of Pathologic Parameters. Am J Clin Pathol. 2005;123(4):529–540. [PubMed.]
- Moore MP., Kinne DW. Breast sarcoma. Surg Clin NorthAm. 1996;76(2):383–92. [PubMed.]
- Chaney AW., Pollack A., Mcneese MD., Zagars GK., Pisters PWT., Pollock RE., et al. Primary treatment of cystosarcoma phyllodes of the breast. Cancer. 2000;89(7):1502–11. [PubMed.]
- Salvadori B., Cusumano F., Del Bo R., Delledonne V., Grassi M., Rovini D., et al. Surgical treatment of phyllodes tumors of the breast. Cancer. 1989;63(12):2532–6. [PubMed.]
- Reinfuss M., Mitus J., Duda K., Stelmach A., Rys J., Smolak K. The treatment and prognosis of patients with phyllodes tumors of the breast. Cancer. 1996;77(5): 910–6. [PubMed.]
- Kapiris I., Nasiri N., A’Hern R., Kung FY., Scolyer RA., Lam RK., et al. Outcome and predictive Factors of local recurrence and distant metastases following primry surgical treatment of High–grade malignant phyllodes tumors of the breast. Eur J Surg Oncol. 2001;27:723–2001. [Ref.]
- Zelek L., Llombart–Cussac A., Terrier P., Pivot X., Guinebretiere JM., Le Pechoux C., et al. Prognostic factors in primary breast sarcomas: a series of patients with long–term Follow–up. J Clin Oncol. 2003;21(13):2583–8. [PubMed.]
- McGowan TS., Cummings BJ., O’Sullivan B., Catton CN., Miller N., Panzarella T. An analysis of 78 breast sarcoma patients without distant metastases at presentation. Int J Radiat Oncol Biol Phys. 2000;46(2):383–90. [PubMed.]
- D’Adamo DR., Keohan M., Schuetze S., Undevia S., Livingston M., Cooney M., et al. Clinical Results of a phase II study of sorafenib in patients with non–GIST sarcomas (ASCO Annual Meeting Proceedings). J Clin Oncol. 2007;25:10001. [Ref.]
- Hodgson NC., Bowen–Wells C., Moffat F., Prancschi D., Avisar E. Angiosarcomas of the Breast: a review of 70 cases. Am J Clin Oncol. 2007;30(6):570–2. [PubMed.]
- Sher T., Hennessy BT., Valero V., Broglio K., Woodward WA., Trent J., et al. Primary Angiosarcomas of the breast. Cancer. 2007;110(1):173–8. [PubMed.]
- Sarcoma Meta–Analysis Collaboration. Adjuvant chemotherapy for localised resectable soft–tissue sarcoma of adults: meta–analysis of individual data. Lancet. 1997;350:1647–54. [PubMed.]
- J P Ngou Mve Ngou., S Mayi–Tsonga., N P Boukanga., F Ondo Ndong. The Phyllodes Tumors of the Breast in Libreville. Epidemiology and prognosis J Le Sein. 2005;15(1–2):32–35. [Ref.]
- Hawkins RE., Schafield JB., Fisher C., Wiltshaw E. The clinical and histologic criteria that predict metastases from cystosarcoma phyllodes. Cancer. 1992;69:141–147. [PubMed.]
- Geisler DP., Boyle MJ., Malnar KF., McGee JM., Nolen MC., Fortner SM., et al. Phyllodes Tumors of the breast: a review of 32 cases. Am Surg. 2000;66:360–6. [PubMed.]
- Pandey M., Mathew A., Kattoor J., Abraham EK., Mathew BS., Rajan B., et al. Malignant phyllodes tumor. Breast J. 2001;7(6):411–6. [PubMed.]
- Cabaret V., Delobelle–Deroide A., Vilain MO. Phyllodes tumors. Arch Anat Cytol Pathol. 1995;43:59–72. [PubMed.]
- De Roos WK., Kaye P., Dent DM. Factors leading to local recurrence or death after surgical Resection of phyllodes tumours of the breast. Br J Surg. 1999;86:396–9. [PubMed.]