>Corresponding Author : Huda A
>Article Type : Case Report
>Volume : 5 | Issue : 9
>Received Date : 20 July, 2025
>Accepted Date : 30 July, 2025
>Published Date : 11 July, 2025
>DOI : https://doi.org/10.54289/JCRMH2500142
>Citation : Huda A, Mounssif A, Moulay-Rchid Z, Arous A. (2025) Critical Left Main Coronary Stenosis During on-Call Hours: A Case for Delayed Revascularization? J Case Rep Med Hist 5(9): doi https://doi.org/10.54289/JCRMH2500142
>Copyright : © 2025 Huda A, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Case Report | Open Access | Full Text
1CH de Gonesse, France
2Centre hospitalier de Gonesse, France -CHU Ibn Rochd Casablanca, Morocco
*Corresponding author: Huda Ayoub, CH de Gonesse, France
Abstract
Introduction: Critical left main coronary artery (LMCA) stenosis is a life-threatening emergency that requires rapid but well-coordinated intervention. However, during on-call shifts, limited staff availability may necessitate stabilization strategies before definitive treatment.
Case Report: We report the case of an 84-year-old woman with a history of ischemic heart disease and atrial fibrillation (CHA DS -VA = 4) who presented with acute chest pain and hemodynamic instability. ECG showed ST elevation in aVR, and diffuse ST depression in lateral and inferior leads. Emergency angiography revealed a 90–99% stenosis of the LMCA with extensive calcification, along with proximal LAD 70% stenosis and 90% circumflex stenosis. An intra-aortic balloon pump (IABP) was inserted for stabilization, and PCI was deferred to the next day. The patient improved clinically and electrocardiographically under IABP. Definitive PCI using a culotte technique was successfully performed the next day with favorable outcomes.
Conclusion: In selected unstable patients with critical LMCA stenosis, early mechanical support with IABP may allow safe deferral of complex PCI until optimal team conditions are available. This case highlights the value of a staged strategy under specific emergency conditions.
Keywords: Left main stenosis, intra-aortic balloon pump, acute coronary syndrome, calcified lesion, staged PCI, elderly patient
Abbreviations: ACS: Acute Coronary Syndrome, AF: Atrial Fibrillation, BCIS-1: Balloon Pump-Assisted Coronary Intervention Study 1, CAD: Coronary Artery Disease, Cx: Circumflex Artery, DFG: Glomerular Filtration Rate, ECG: Electrocardiogram, ESC: European Society of Cardiology, FEVG / LVEF: Left Ventricular Ejection Fraction, HB / Hb: Hemoglobin, IABP: Intra-Aortic Balloon Pump, IVL: Intravascular Lithotripsy, IVUS: Intravascular Ultrasound, LAD / IVA: Left Anterior Descending artery, LMCA: Left Main Coronary Artery, PCI: Percutaneous Coronary Intervention, POT: Proximal Optimization Technique, RCA: Right Coronary Artery, STEMI: ST-Segment Elevation Myocardial Infarction
Introduction
Critical stenosis of the left main coronary artery (LMCA) is a cardiologic emergency associated with high mortality if not rapidly addressed. Primary percutaneous coronary intervention (PCI) is often required; however, certain situations—such as extreme patient frailty, anatomical complexity, and limited technical resources during on-call hours—may demand a more conservative and staged approach. Mechanical circulatory support, particularly via intra-aortic balloon pump (IABP), can provide temporary stabilization and time to organize optimal conditions for intervention.
We present a case of critical LMCA stenosis in an elderly woman admitted during an on-call period, where a conservative, staged strategy including IABP use led to a successful outcome.
Case Report
An 84-year-old female patient with a medical history of ischemic heart disease, previously treated with right coronary artery (RCA) stenting (although procedural documentation was unavailable) and paroxysmal atrial fibrillation (with a CHA DS VA score of 4), presented with acute-onset chest pain that had persisted for approximately four hours. Upon admission, she was hypotensive, with a blood pressure of 70/40 mmHg, and continued to experience anginal symptoms.
Electrocardiographic findings revealed STsegment elevation in lead aVR, and diffuse ST depression in and inferior leads, an electrocardiographic pattern highly suggestive of left main coronary artery involvement or severe proximal multivessel ischemia. (Figure 1) Owing to the patient's hemodynamic instability, inotropic support with dobutamine was initiated promptly, and an emergency coronary angiography was performed without delay. Preprocedural echocardiography showed a moderately reduced left ventricular ejection fraction (LVEF estimated at 40–45%) with anterior and apical hypokinesia. Laboratory tests revealed a significantly elevated troponin level, a reduced glomerular filtration rate (eGFR at 42 mL/min/1.73 m²), and anemia (hemoglobin at 9.6 g/dL), all contributing to the global frailty of the patient.
The angiogram demonstrated a critical stenosis (90–99%) of the left main coronary artery, characterized by a voluminous and heavily calcified plaque, (Figure 2). Additionally, a 70% narrowing of the proximal left anterior descending (LAD) artery and a 90% stenosis of the proximal circumflex artery were noted. In view of the complexity of the coronary anatomy, the frailty of the patient, and the absence of a full interventional team during on-call hours, the decision was to insert an intra-aortic balloon pump (IABP) for circulatory support. Revascularization was intentionally postponed to the following day to ensure the presence of the full catheterization team, including imaging and surgical backup.
By the next morning, the patient's clinical status had improved significantly. She was asymptomatic, and her ECG showed regression of the ST segment elevation in AVR.
A second coronary angiography was conducted, and percutaneous coronary intervention (PCI) of the left main bifurcation was successfully performed. The procedure began with endotracheal intubation and selective cannulation using an XB3 guiding catheter. A Sion 0.014" guidewire was advanced into the LAD, and a Fielder wire was used to cross into the distal circumflex artery. Lesion preparation involved predilatation of the distal circumflex with a 2.5 × 20 mm TREK balloon, followed by a non-compliant (NC) 3.0 × 25 mm balloon at the circumflex ostium and distal left main. A SYNERGY XD 2.75 × 28 mm drug-eluting stent was deployed across the distal left main, covering into the circumflex. Further balloon optimization was performed using a 3.5 × 15 mm balloon at the ostium of the circumflex and a PANTERA 3.5 × 8 mm balloon in the distal left main. A 3.0 × 15 mm balloon was passed through the stent struts into the LAD ostium, where a second SYNERGY 2.75 × 20 mm stent was deployed. Final kissing balloon inflation was performed using two NEON PTCA 3.0 × 15 mm balloons, one in each branch (LAD and Cx), followed by proximal optimization (POT) of the left main using a PANTERA PRO 3.5 × 10 mm balloon. During the intervention, a dissection occurred in the LAD, likely precipitated by manipulation within the densely calcified plaque. This complication was promptly managed by the deployment of an additional stent. The entire procedure followed a culotte stenting technique and was completed successfully without hemodynamic complications (Figure 3).
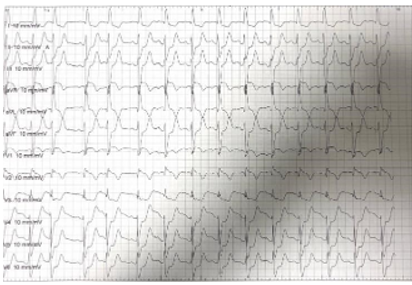
Figure 1: EKG at admission showing ST elevation in AVR and ST depression in lateral and inferior leads
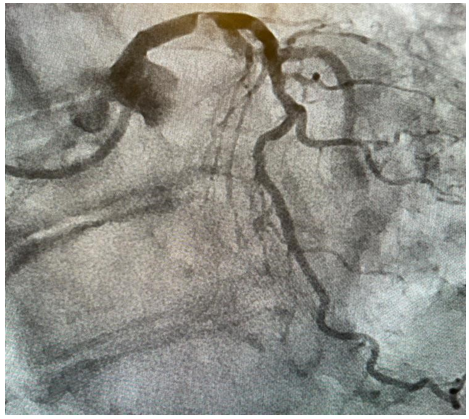
Figure 2: Angiogram showing severe stenosis of left main associated to severe stenosis in Cx and LAD

Figure 3: Angiogram showing final result
Discussion
This case shows the complexity of acute left main coronary artery disease in a fragile, elderly patient presenting with hemodynamic instability. The decision to initially stabilize the patient with IABP, while delaying intervention until full technical support was available, was made in light of both clinical and logistical constraints. This approach allowed temporary ischemic relief and hemodynamic improvement, which created a safer window for revascularization the next day. Although surgical revascularization is often considered for left main disease, it was ruled out in this patient due to multiple high-risk factors, including advanced age, chronic atrial fibrillation requiring anticoagulation, reduced glomerular filtration rate, and underlying anemia, all of which significantly increased the perioperative risk [1]. Selective use of mechanical support such as IABP in unstable patients is supported by observational data showing improved procedural safety in left main and multivessel disease, even though randomized trials like BCIS-1 did not demonstrate a survival benefit in stable, elective PCI settings [2-4]. In this case, IABP provided a vital bridge that allowed us to avoid rushed intervention under suboptimal conditions. This approach is consistent with current European Society of Cardiology (ESC) 2023 guidelines, which do not recommend routine IABP use during PCI in acute coronary syndromes (Class III), but allow for its selective application (Class IIb) in patients with cardiogenic shock or severe hemodynamic compromise, as was the case in our patient [5]. During PCI, a dissection occurred in the LAD, most likely due to the dense calcific burden. Intravascular lithotripsy (Shockwave) could have been considered to modify the lesion more effectively, but its use was deferred [6]. Despite being available, we avoided it due to concerns over the need for repeated balloon inflations in a critically stenosed and unstable left main artery, where each inflation could carry hemodynamic consequences. Ultimately, the staged approach led to a successful outcome, emphasizing the importance of individualized decision-making that takes into account anatomical complexity, patient frailty, and procedural risk in high-stakes coronary interventions.
Conclusion
In high-risk patients presenting with critical left main stenosis during emergency hours, a conservative, staged approach supported by IABP may offer a safe and effective alternative to immediate PCI when resources are limited. This strategy allows for optimal timing, team readiness, and procedural success, particularly in anatomically complex or frail patients.
Ethics approval: The requirement for informed consent was waived by the Ethics Committee.
Consent for publication: Not applicable
Clinical trial number: Not applicable
Funding: Not applicable
References
- Waldo SW., Secemsky EA., O’Brien C., Kennedy KF., Pomerantsev E., Sundt TM., et al. Surgical ineligibility and mortality among patients with unprotected left main or multivessel coronary artery disease undergoing percutaneous coronary intervention. Circulation. 2014;130(25):2295–301. [PubMed.]
- Unverzagt S., Buerke M., De Waha A., Haerting J., Pietzner D., Seyfarth M., et al. Intra-aortic balloon pump counterpulsation (IABP) for myocardial infarction complicated by cardiogenic shock. Cochrane Heart Group, éditeur. Cochrane Database of Systematic Reviews [Internet]. 2015;27(3). [PubMed.]
- Truesdell AG., Davies R., Eltelbany M., Megaly M., Rosner C., Cilia LA. Mechanical Circulatory Support for Complex High-risk Percutaneous Coronary Intervention. US Cardiology. 2023;4:17:e03. [PubMed.]
- Luo D., Huang R., Wang X., Zhang J., Cai X., Liu F., et al. Intra-aortic balloon pump reduces 30-day mortality in early-stage cardiogenic shock complicating acute myocardial infarction according to SCAI classification. Shock [Internet]. 2023;60(3):385–391. [PubMed.]
- Byrne RA., Rossello X., Coughlan JJ., Barbato E., Berry C., Chieffo A., et al. 2023 ESC Guidelines for the management of acute coronary syndromes. European Heart Journal. 12 oct 2023;44(38):3720–826. [PubMed.]
- Elzain H., Alasousi N., Adel Mostafa M., Ali K., Babiker A. Successful Percutaneous Coronary Intervention (PCI) of a Heavily Calcified Left Main Artery Using Shockwave Intravascular Lithotripsy and Intra-aortic Balloon Pump (IABP) Support in an Octogenarian Acute Coronary Syndrome Patient Deemed High Risk. Cureus. 2025;17(5):e83585. [PubMed.]