>Corresponding Author : Benhaddouga Khadija
>Article Type : Case Report
>Volume : 5 | Issue : 8
>Received Date : 06 July, 2025
>Accepted Date : 16 July, 2025
>Published Date : 20 July, 2025
>DOI : https://doi.org/10.54289/JCRMH2500138
>Citation : Benhaddouga K, Bahlioui FE, Guezri A, Chyate FZ, Benchrifi Y, et al. (2025) Papillary Endometrial Carcinoma: 1 Case Report and Review of the Literature. J Case Rep Med Hist 5(8): doi https://doi.org/10.54289/JCRMH2500138
>Copyright : © 2025 Benhaddouga K, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Case Report | Open Access | Full Text
1Resident Physician, Department of Gynecology and Obstetrics, at Ibno Rochd University Hospital, Casablanca, Morocco
2Professor in the Department of Gynecology and Obstetrics at the Ibno Rochd University Hospital in Casablanca, Morocco
*Corresponding author: Benhaddouga Khadija, Resident Physician, Department of Gynecology and Obstetrics, at Ibno Rochd University Hospital, Casablanca, Morocco
Abstract
Papillary endometrial carcinoma is a rare and aggressive form of uterine cancer, distinct from the more common endometrioid types. It occurs mainly in post-menopausal women, in the absence of hyperestrogenism. Histologically, it is characterized by a complex papillary architecture and marked nuclear atypia. Diagnosis is based on histology and immunohistochemistry, enabling differentiation from serous carcinoma. Treatment is based on a multimodal approach combining surgery, chemotherapy and sometimes radiotherapy. Due to its aggressive nature, the prognosis remains guarded, with a high risk of recurrence and metastasis. Recognition of this entity is helping to optimize management and steer research towards more targeted therapies.
Keywords: Papillary Carcinoma, Endometrium, Uterine Cancer, Histology, Immunohistochemistry, Treatment, Prognosis, Type II, Aggressive Tumor
Abbreviations: MRI: Magnetic Resonance Imaging, p53: Tumor Protein 53, p16: Cyclin-Dependent Kinase Inhibitor 2A, CT: Computed Tomography, N+: Number of positive lymph nodes, N: Total number of lymph nodes examined, 5-year survival: Five-year overall survival rate, FIGO: International Federation of Gynecology and Obstetrics
Introduction
Papillary endometrial carcinoma is a rare and poorly described histological form of endometrial cancer, often confused with serous carcinoma due to their morphological similarity. Although the majority of endometrial cancers are of the low-grade endometrioid type, this papillary variant presents distinct biological and clinical features, associated with more aggressive behavior. Histologically, it is an epithelial tumor with complex papillary structures, a fibrovascular axis and marked nuclear atypia. This form of tumor occurs mainly in post-menopausal patients, often without a history of endometrial hyperplasia or prolonged exposure to estrogen, which distinguishes it from the more frequent type I forms [1]. Precise diagnosis is often difficult, and relies on rigorous histopathological and immunohistochemical criteria, essential to avoid underestimating the prognostic risk.
Case Report:
A 63-year-old woman with no specific pathological history presented with 5 episodes of postpartum metrorrhagia dating back 5 months.
On clinical examination: presence of a 1.5 cm polyp of the anterior lip of the cervix with exocervical implantation + 5 mm polypoid lesion of the right lateral wall of the vagina (figure 1).
Pelvic ultrasound: 25 mm endometrial thickening (figure 2)
Pelvic MRI: heterogeneous endometrial thickening, enhanced after gadolinium injection, measuring 33 mm spread over 84 mm, this thickening appears to infiltrate almost the entire anterior myometrium. No effusion, no adenopathy. (figure 3)
Cervical biopsy: remodelled cervical ectropion.
Vaginal biopsy: fibroepithelial hyperplasia consistent with polyp.
Cervico-uterine smear: no signs of malignancy.
Endometrial biopsy: papillary endometrial carcinoma infiltrating the myometrium.
The patient underwent total hysterectomy without adnexal preservation + omentectomy + bilateral pelvic and lombo-aortic curage, with anatomopathological study:
Total hysterectomy without adnexal preservation: invasive papillary endometrial carcinoma measuring3.5cm long axis, infiltrating more than 50% of the myometrium. Absence of images of vascular emboli and peri-nervous sheathing.
Omentectomy: no evidence of malignancy.
Bilateral pelvic and lumbo-aortic curage: absence of lymph node metastasis 0N+/10N.

Figure 1: Speculum examination showing polypoid lesions of the cervix and vagina
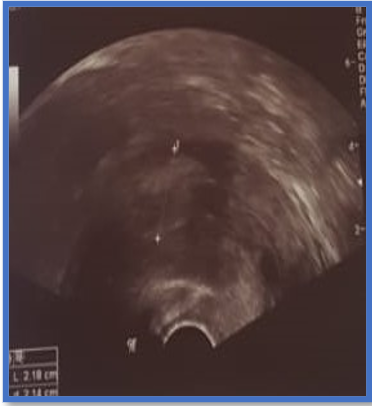
Figure 2: Ultrasound image of endometrial thickening

Figure 3: MRI image of endometrial thickening appearing to infiltrate the anterior myometrium
Discussion
Papillary endometrial carcinoma is classified as a type II carcinoma, a group of non-oestrogen-dependent tumours with poor differentiation and a poor prognosis [2]. Its frequency is estimated at less than 5% of endometrial cancers, but it is probably under-diagnosed due to its morphological overlap with other entities, notably serous endometrial carcinoma. Histologically, it presents a complex papillary architecture, with a cell lining featuring severe nuclear atypia and frequent mitosis. Immunohistochemistry is often necessary to distinguish this form from other serous tumours: abnormal and diffuse expression of p53 and overexpression of p16 are often found in serous forms, whereas some papillary forms may show a more heterogeneous profile [3,4].
Clinically, papillary carcinoma usually manifests as post-menopausal metrorrhagia. Imaging can detect an endometrial mass, but only histological examination of an endometrial biopsy or surgical specimen can provide a definitive diagnosis. Treatment is mainly based on complete excision surgery (total hysterectomy with bilateral adnexectomy), often combined with pelvic and para-aortic lymph node dissection, depending on risk factors. Because of the high risk of locoregional and metastatic recurrence, adjuvant chemotherapy (often carboplatin and paclitaxel) is recommended for advanced or high-grade forms [5]. Radiotherapy, in particular vaginal brachytherapy, may be indicated as a complement. Targeted therapies have not yet been validated for this subpopulation, although specific molecular abnormalities are being investigated.
The prognosis of papillary carcinoma is generally poor compared with well-differentiated endometrioid forms. Several studies have shown a 5-year survival rate of less than 50% in advanced stages, largely due to the propensity for early dissemination and chemoresistance [6]. Knowledge of this entity by pathologists and clinicians is therefore essential to ensure appropriate management.
Conclusion
Papillary endometrial carcinoma is a rare but clinically significant tumor, due to its aggressiveness and unfavorable prognosis. Recognition is based on precise histopathological and immunohistochemical analysis. Optimal treatment requires a multimodal approach including surgery, chemotherapy and possibly radiotherapy. Better characterization of this tumor type, particularly through molecular analysis, will enable us to develop more targeted and potentially more effective therapeutic strategies in the future.
Reference
- Kurman RJ, Carcangiu ML, Herrington CS, Young RH. WHO classification of tumours of female reproductive organs. 4th ed. Lyon: IARC; 2014. [Ref.]
- Bokhman JV. Two pathogenetic types of endometrial carcinoma. Gynecol Oncol. 1983;15(1):10–17. [PubMed.]
- Zheng W, Wolf M, Kramer EE, Yang GC, Schwartz PE, Chambers JT. Papillary carcinoma of the endometrium: a clinicopathologic study of 15 cases. Int J Gynecol Pathol. 1995;14(4):300–6. [Ref.]
- Tafe LJ, Garg K, Chew I, et al. Endometrial carcinomas with ambiguous features: diagnostic utility of immunohistochemistry and the importance of accurate classification. Am J Surg Pathol. 2010;34(9):1370–80. [Ref.]
- Colombo N, Preti E, Landoni F, Carinelli S, Colombo A, Marini C, Sessa C. Endometrial cancer: ESMO Clinical Practice Guidelines. Ann Oncol. 2013;24(Suppl 6):vi33–8. [PubMed.]
- Hamilton CA, Cheung MK, Osann K, et al. Uterine papillary serous and clear cell carcinomas predict poor outcome: a SEER analysis. Gynecol Oncol. 2006;102(2):279–83. [Ref.]