>Corresponding Author : Benhaddouga Khadija
>Article Type : Case Report
>Volume : 5 | Issue : 7
>Received Date : 06 July, 2025
>Accepted Date : 16 July, 2025
>Published Date : 20 July, 2025
>DOI : https://doi.org/10.54289/JCRMH2500135
>Citation : Benhaddouga K, Elhodaigui N, Sakim M, Chyate FZ, Hayat M, et al. (2025) Gynecologic Uterine Inversion: A Case Report. J Case Rep Med Hist 5(7): doi https://doi.org/10.54289/JCRMH2500135
>Copyright : © 2025 Benhaddouga K, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Case Report | Open Access | Full Text
1Department of Obstetrics and Gynecology, Ibn Rochd University Hospital / El Harouchi Mother and Child Hospital, Casablanca, Morocco
2Faculty of Medicine and Pharmacy, Hassan II University of Casablanca, Casablanca, Morocco
*Corresponding author: Benhaddouga Khadija, Department of Obstetrics and Gynecology, Ibn Rochd University Hospital / El Harouchi Mother and Child Hospital, Casablanca, Morocco
Abstract
Neuroendocrine breast tumors represent a rare subtype of breast cancer, accounting for less than 1% of all neuroendocrine neoplasms. Starting from their pathology definition, and going through their prevalence, prognosis and treatment, our knowledge is still really uncertain.
In the present short review of the medical literature on this topic, we have evaluated their epidemiology, pathogenesis, pathology, clinical presentation, radiographic aspects, prognosis, and therapy. Our ultimate aim was actually to try to understand whether neuroendocrine neoplasms of the breast can be considered a definite clinical entity and if neuroendocrine differentiation of breast tumors has a really clinical relevance.
Keywords: Uterine inversion, Non-puerperal, Uterine preservation
Abbreviations:CBE: Curettage Biopsy of the Endometrium, CT: Computed Tomography, MRI: Magnetic Resonance Imaging, SA: Semaines d'Aménorrhée
Introduction
Uterine inversion is a rare and serious condition, more common in obstetrics than gynecology, and can be life-threatening due to hypovolemic shock. It is characterized by the turning inside out of the uterus like a glove finger. The condition is classified into different degrees based on the position of the uterine fundus:
• First degree: Depression of the fundal area within the vaginal cavity, resembling a "cup shape."
• Second degree: The fundus passes through the external cervical os.
• Third degree: The fundus is completely within the vagina or even protruding through the vulva.
• Fourth degree: Vaginal walls are also inverted along with the uterus.
Due to its rarity, diagnosis is often delayed. The main differential diagnosis is a prolapsed fibroid.
Two clinical presentations are described: an acute form with severe, sudden symptoms, and a chronic form, which may cause pelvic heaviness and/or mild abnormal bleeding, or even remain asymptomatic and only discovered via imaging.
Observation:
The patient is a 45-year-old woman, single, nulligravida. She had her menarche at 12 years old, with regular menstrual cycles. She underwent an endometrial biopsy curettage (CBE) in January 2024, which revealed endocervical polypoid endometrial hyperplasia.
She has a 9-month history of progressively worsening menometrorrhagia. Initially light, the bleeding gradually increased in amount and frequency over the months, accompanied by acute pelvic pain and general condition deterioration (asthenia).
Pelvic ultrasound revealed a globular uterus with regular contours and homogeneous echotexture. An intra-cavitary, round, well-circumscribed, homogeneous, hypoechoic formation measuring 17 x 19 x 17.5 mm was noted.

Figure 1: Pelvic Ultrasound
Pelvic MRI (27/03/2024):
A large pedunculated polyp with cystic and hemorrhagic changes was identified. The polyp’s stalk was implanted at the left uterine horn and measured 6 x 2 cm. Its main body occupied and distended the cervico-isthmic cavity, measuring 7 x 6 x 7.7 cm.
Abdomino-pelvic CT scan findinding an indented appearance of the uterine fundus within the vaginal cavity, consistent with uterine inversion. The vaginal cavity and cul-de-sacs were occupied by an intermediate-density mass measuring 95 x 84 x 74 mm, juxtaposed with a cystic liquid component containing air bubbles. There was a small amount of intra-peritoneal fluid in the right iliac fossa.
CT findings indicate uterine inversion secondary to a probable polyp expelled through the cervix.
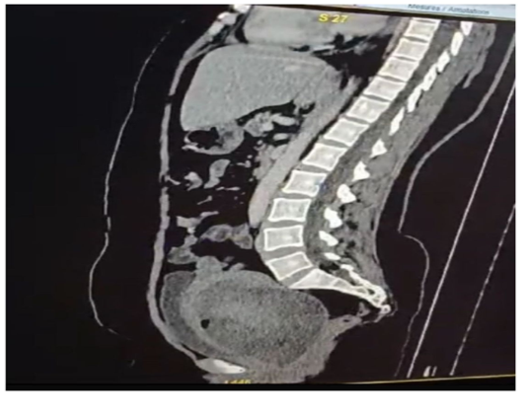
Figure 2: Abdomino-pelvic CT scan findings indicate uterine inversion secondary to a probable polyp expelled through the cervix.
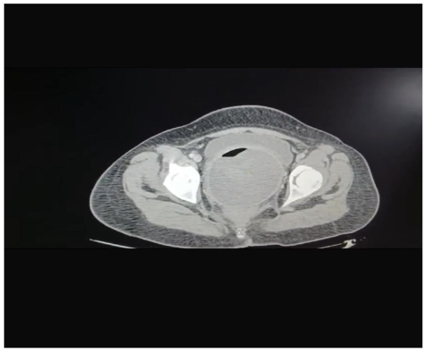
Figure 3: Abdomino-pelvic CT scan findings indicate uterine inversion
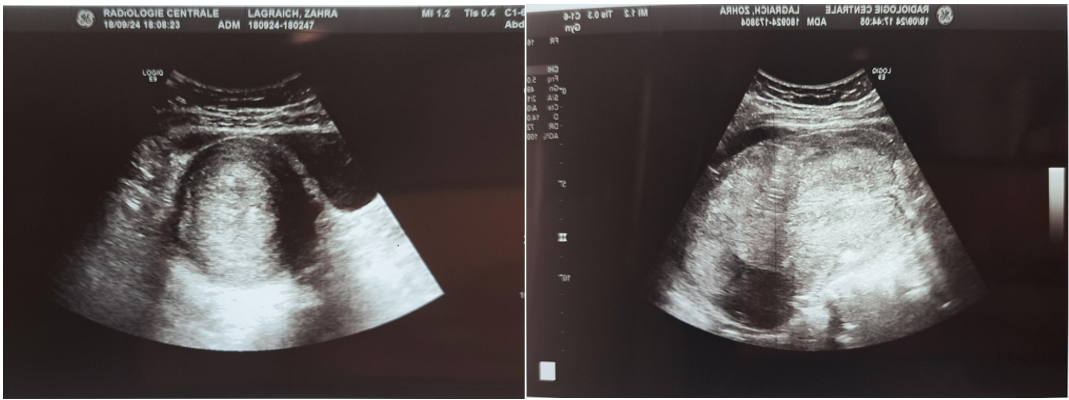
Figure 4-5: Pelvic ultrasound
Surgical exploration was performed under general anesthesia. On vaginal examination, a prolapsed mass was found in the vagina. A median skin incision was made, and exploration revealed a moderate peritoneal effusion. An intrauterine myoma was identified as the cause of the uterine inversion. Additionally, a right para-tubal cyst was noted.
The surgical procedures performed included a para-tubal cystectomy, an anterior isthmectomy, and a myoma resection. Additionally, the uterine inversion was reduced using a conservative approach.

Figure 6: The intraoperative pelvic finding of the chronic uterine inversion

Figure 7: Surgical parts
Discussion
Uterine inversion is an extremely rare but severe complication. In the postpartum context, its incidence is about 1 in 100,000 deliveries in France [1], and fewer than 200 cases have been reported in the literature [2].
Most reported cases involve postmenopausal women or those over 45 years old [3]. Four cases involving embryonal rhabdomyosarcoma in adolescent girls have also been described [4].
As previously mentioned, inversion is classified into four degrees depending on the descent of the fundus. Alternative classifications exist, such as partial or total inversion [5], and acute or chronic inversion, based on the onset and progression of symptoms [6].
Acute non-puerperal inversion is usually dramatic, marked by severe pelvic pain and heavy bleeding [7].
Chronic non-puerperal inversion presents more subtly, with pelvic discomfort, vaginal discharge, mild bleeding, and often severe anemia [7]. In this case, the patient had a total inversion of acute onset, triggered by uncontrolled traction on a fibroid, evolving into a chronic state.
Data on this condition in Africa remain scarce despite the high prevalence of uterine fibroids among Black women, identified as the main cause of non-puerperal inversion [8]. Additional contributing risk factors include thin uterine walls, disorganized tumor growth, large tumor size, its location, single-pedicle attachment, cervical dilation due to uterine distension, and tumor dehiscence [8].
In 70–85% of cases, the cause is a submucous fibroid [3]. In 15–30% of cases, malignant tumors are involved, mainly uterine sarcomas (leiomyosarcoma, embryonal rhabdomyosarcoma, and endometrial stromal sarcoma). Less frequently, inversion occurs in cases of endometrial carcinoma [9] or mixed Müllerian tumors [6].
In this reported case, the tumor was attached to the uterine fundus via a single pedicle. Prompt and appropriate management might have prevented the evolution toward chronicity and the severe anemic and infectious complications observed.
Management included initial medical stabilization over 48 hours with volume resuscitation and broad-spectrum antibiotics, followed by surgical intervention.
A conservative approach is preferred when reduction of the inversion is possible, particularly in first- and second-degree cases. Radical surgery, such as hysterectomy, is recommended when there is no fertility desire and is almost always necessary for third- and fourth-degree inversions.
Hysterectomy can be performed vaginally, though it poses technical challenges due to distorted anatomy, especially regarding the urinary tract (ureters and bladder). An abdominal approach has also been described, requiring reduction of the inversion before removal.
A combined laparoscopic and vaginal approach, as reported by Auber et al. [10], offers a promising alternative. It allows for confirmation of the diagnosis, assessment of ischemia in the adnexa and vagina, and uterine devascularization via laparoscopy by controlling the uterine pedicle at its origin.
In literature, uterine artery embolization has been described for chronic non-puerperal inversions (typically second or third degree) and reducible acute puerperal inversions as part of conservative management.
Conclusion
Acute non-puerperal uterine inversion is a rare complication that is often difficult to diagnose preoperatively due to the urgency of the presentation. Total hysterectomy using a combined laparoscopic and vaginal approach is a reliable and safe surgical technique. We present an exceptional case of acute non-puerperal uterine inversion in a young woman caused by a fibroid. Successful management was achieved through a conservative surgical approach combining both vaginal and abdominal methods.
Reference
- Jerbi M, Iraqui Y, Jacob D, Truc JB. Acute puerperal uterine inversion : about two cases. Gynecol Obstet Fertil. 2004; 32:224–47. [PubMed.]
- Martin A, Tranoulis A, Sayasneh A. Uterine inversion secondary to a large leiomyoma prolapse: diagnostic and management issues. Cureus. 2020; 12:e7168. [PubMed.]
- Lupovitch A, Edwin R, Ruey C. Non-puerperal uterine inversion in association with uterine sarcoma: case report in a 26-year-old and review of the literature. Gynecol Oncol. 2005; 97:938–41. [Ref.]
- Da Silva BB, Dos Santos AR, Parentes-Vieira JB, Lopes-Costa PV, Pires CG. Embryonal rhabdomyosarcoma of the uterine inversion in an adolescent: a case report and published work review. J Obstet Gynaecol Res. 2008; 34:735–8. [Ref.]
- Takano K, Ichikawa Y, Tsunoda H, Nishida M. Non-puerperal inversion in association with uterine sarcoma: a case report. Jpn J Clin Oncol. 2001; 31(1):39–42. [Ref.]
- Moulding F, Hawnaur JM. MRI of non-puerperal uterine inversion due to endometrial carcinoma. Clin Radiol. 2004; 59:534–7. [PubMed.]
- Tuckett JD, Yeung A, Timmons G, Hughes T. Non-puerperal inversion in association with uterine sarcoma and ascites demonstrated on CT and MRI. J Radiol Extra. 2010; 75(3):e119–23. [Ref.]
- Kouamé A, Koffi SV, Adjoby R, et al. Non-puerperal uterine inversion in an adolescent: a case report. J West Afr Coll Surg. 2015; 5(3):78–83. [Ref.]
- Oguri H, Maeda N, Yamamoto Y, Wakatsuki A, Fukaya T. Non-puerperal uterine inversion associated with endometrial carcinoma: a case report. Gynecol Oncol. 2005; 97:973–5. [PubMed.]
- Auber M, Darwish B, Lefebure A, Ness J, Roman H. Management of non-puerperal uterine inversion using a combined laparoscopic and vaginal approach. Am J Obstet Gynecol. 2011; 204:e7–9. [PubMed.]