>Corresponding Author : Benhaddouga Khadija
>Article Type : Case Report
>Volume : 5 | Issue : 7
>Received Date : 06 July, 2025
>Accepted Date : 16 July, 2025
>Published Date : 20 July, 2025
>DOI : https://doi.org/10.54289/JCRMH2500133
>Citation : Benhaddouga K, Moustatir M, Mesnaoui O, Chyate FZ, Hossaine B, et al. (2025) Male Breast Cancer: About 1 Case. J Case Rep Med Hist 5(7): doi https://doi.org/10.54289/JCRMH2500133
>Copyright : © 2025 Benhaddouga K, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Case Report | Open Access | Full Text
1Resident Physician, Department of Gynecology and Obstetrics, at Ibno Rochd University Hospital, Casablanca, Morocco
2Professor in the Department Mohammed VI Oncology Centre, University Hospital Center Ibn Rochd, Casablanca , Morocco
*Corresponding author: Benhaddouga Khadija, Resident Physician, Department of Gynecology and Obstetrics, at Ibno Rochd University Hospital, Casablanca, Morocco
Abstract
Male breast cancer is a rare and little-known pathology. Its incidence is increasing in industrialized countries. There are many similarities with cancer in women, but there are also particularities in management, linked to patient age, the presence of co-morbidities, longer diagnosis times and smaller breast volume. Total mastectomy with axillary curage remains the gold standard. Sentinel node sampling is a promising option for early-stage management. Adjuvant irradiation is generally systematic, and tamoxifen remains the hormone therapy of choice. Adjuvant chemotherapy may be offered to high-risk patients. Overexpression of the HER2 oncoprotein, observed in 10-15% of patients, may justify the prescription of trastuzumab. Against the backdrop of the considerable progress achieved in recent years in the management of female breast cancer, we feel it is important to take stock of the data acquired and the possibility of exploiting these advances to improve the management of male breast cancer. Based on an observation of breast cancer, we review the clinico-radiological, therapeutic and prognostic aspects of this condition.
Keywords: Male breast cancer; Prognostic factors; Treatment
Abbreviations:HER2: Human Epidermal Growth Factor Receptor 2, RE: Estrogen Receptor, RP: Progesterone Receptor, ACR: American College of Radiology, ADP: Adenopathy, CAT scan: Computed Axial Tomography scan, MRI: Magnetic Resonance Imaging, BRCA1: Breast Cancer Gene 1, BRCA2: Breast Cancer Gene 2, c-erbB-2: Human Epidermal Growth Factor Receptor 2, UICC: Union for International Cancer Control, SBR grade: Scarff-Bloom-Richardson Grade
Introduction
Male breast cancer is a rare condition, accounting for around 1% of all breast cancers and less than 1% of all male neoplasia. [1]
The incidence of this male pathology has risen steadily from 0.86/100,000 to 1.06/100,000 over the past three decades. [2]
Ductal carcinoma is the most common histological type. It is a pathology most often diagnosed at an advanced stage, making its prognosis bleak. [3]
The appearance of cutaneous signs is the main reason for consultation; on the occasion of a new observation of infiltrating ductal carcinoma of the breast in men, we have reviewed the literature with the essential aim of clarifying its similarities to that of women.
Therapeutic management has been extrapolated from knowledge acquired in women. Conservative surgical treatment is rarely appropriate for male breast cancer, partly because of the small size of the breast and partly because mastectomy is readily accepted. On the other hand, all other treatments - surgical (axillary curage or sentinel lymph node), radiotherapy, chemotherapy, hormone therapy (tamoxifen or antiaromatases) and biotherapy (trastuzumab) - can form part of the therapeutic arsenal available to us to combat this rare form of cancer. [4]
Case Report
This 53-year-old patient, whose father had died of breast neo at the age of 81, without any other pathological history, presented with a retroareolar swelling of the neglected right breast, which had been evolving for 2 years and was progressively increasing in size.
Clinical examination revealed an ulcerative-bourgnant mass dependent on the right breast areolar plate, hard, fixed to the deep and superficial planes, measuring 4 cm in long axis. Accompanied by homolateral axillary adenopathy (fig. 1).

Figure 1: An ulcerative breast mass on the right nipple-areolar plate
Examination of the external genitalia was unremarkable.
An ultrasound scan revealed a nodular lesion at the nipple; well limited, with irregular contours, vascularized on color Doppler, infiltrating the posterior parietal plane; hypoechoic, heterogeneous, measuring 37x36x25 mm
A homolateral hypoechoic, heterogeneous axillary adenopathy measuring 20x11 mm was associated; the lesion was classified as ACR5 (fig. 2).
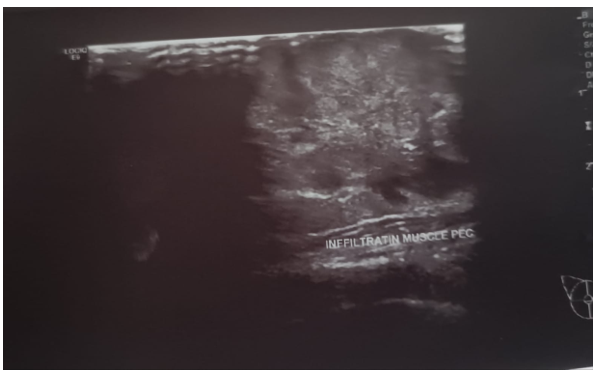
Figure 2: Ultrasonographic appearance of a nodular lesion suspected of malignancy that appears to infiltrate the posterior parietal plane.
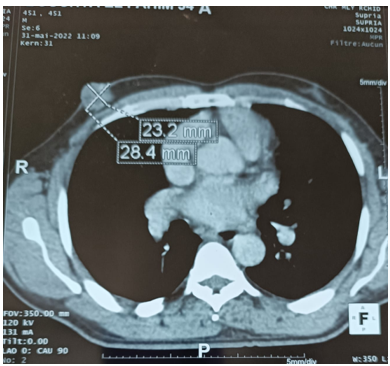
Figure 3: Scannographic appearance of a tumor-like process on the right nipple without signs of locoregional extension
The extension workup (bone scan, CA 15-3) was negative. CAT scan: showed a right mamma process measuring 28x23 mm with a tumoral appearance and no signs of locoregional extension, associated with a right axillary ADP measuring 16.6 mm (fig. 3).
A skin biopsy was performed, showing the localization of an invasive breast adenocarcinoma with strong, diffuse expression of hormone receptors (RE100% and RP 90%); no overexpression of anti-HER 2 and Ki67% at 30%; the patient had undergone neoadjuvant chemotherapy.
Discussion
Male breast cancer is an extremely rare disease, accounting for 0.5 to 1% of breast cancers in Western countries, and 0.4 to 1.2% of all male cancers [5].
The first description dates back to 1307 and was made by an English surgeon, John of Arderne [6]. Its incidence has risen sharply over the past 25 years [7]. The average age of onset of breast cancer in men is around 60. In fact, its incidence increases with age [8]; The etiopathogenesis of male breast cancer is still unknown [9]; Certain predisposing factors have been identified. These are mainly pathological situations with a common factor represented by an anomaly of hormonal metabolism related to relative hyperestrogenism or hyperprolactinemia [10].
Family and genetic antecedents are found in 5 to 10% of cases [9]. This notion of “breast cancer families” is related to the existence of genetic mutations in numerous genes, the most common of which are: BRCA1, BRCA2, p53 and c-erbB-2 [11]
Statistically confirmed risk factors in several studies are:
A family history of breast cancer and especially breast cancer among first-degree relatives [9]
The existence of a BRCA2 gene mutation; male infertility: it seems to increase the risk of breast carcinoma in men [12];
Obesity, which is thought to be responsible for an increase in the conversion of androgens to estrogens by peripheral aromatization in adipose tissue. [13]
Ultramammography is the basic investigation of breast nodules in men. The sensitivity and specificity of mammography in the diagnosis of male breast cancer are 92% and 90% respectively. Mammography is well suited to differentiating between gynecomastia and cancerous lesions. A single incidence may be performed. It must include the same study elements as in women (tonality, dimensions, location, contours, micro-calcifications, etc.) and must result in the same ACR classification. [14] The signs of malignancy to look for are the same as in women, such as stellate opacity or architectural distortion. [14] On the other hand, microcalcifications are less frequent than in women, found in the first case of our work [14]. Ultrasound also reveals the same signs of malignancy and offers the possibility of an ultrasound-guided biopsy, which alone will enable a diagnosis of malignancy to be made with certainty. [14] MRI is only exceptionally indicated [14] in most cases, male breast cancer presents as a painful subareolar swelling, nipple retraction or bloody discharge; the delay between the first symptoms and diagnosis is later than in women [15].
The most common histological type is invasive ductal carcinoma, which accounts for between 71.7% and 91.5% of male breast cancers in all epidemiological studies [16].
Other histological forms are rarer: 1-10% (papillary carcinoma, infiltrating lobular carcinoma, ductal carcinoma in situ and sarcoma)
Histological lymph node involvement is a poor prognostic factor, with a frequency of 50-60% [6].
Male breast cancer is characterized by strong hormone dependence. In studies conducted by Oger et al, Tounon de Lara et al, Hill et al, and Giordano et al, [16, 2]. showed estrogen receptor positivity in 90 to 97.4% of cases, progesterone receptors in 80.2% to 83%. Overexpression of HER2 genes was found in 7 to 38% of cases.
72% to 82% of male breast cancers are high-grade (grade II and III) [16]
The therapeutic strategy for managing cancer in men is similar to that for women [11]. In the early stages, most men are treated with a modified radical mastectomy combined with axillary curage or selective lymphadenectomy [17].
In a series of 31 cases of ductal carcinoma in situ, they showed three relapses after six lumpectomies (50%), whereas they found only one case of relapse after 25 mastectomies. The small size of the mammary gland makes it difficult to move to healthy margins [17]. Conservative surgical treatment is therefore not indicated in the treatment of male breast cancer, due to the small volume of the breast and the ease with which men accept mastectomy. Post-operative radiotherapy improves local control and progression-free survival but has no impact on overall survival Tamoxifen-type hormone therapy is considered the standard adjuvant treatment for patients expressing hormone receptors. [12] The main side effects remain the risk of thromboembolic complications, hot flushes and reduced libido [17]. Prognosis depends on several clinical, histological and biological parameters
International Union Against Cancer (UICC) clinical stage, histological type, lymph node involvement, SBR grade, vascular emboli and hormone receptor expression.
Male breast cancer is reputed to have a worse prognosis than female breast cancer. However, survival is similar to that of female breast cancer if we compare adjusted survival rates excluding deaths from intercurrent disease or second cancer.
Conclusion
Male breast cancer is a rare and little-known condition and is therefore often diagnosed at an advanced stage. It occurs at a higher age than in women. Its causes are as yet unknown.
Locoregional treatment is dominated by surgery; in our context, Patey-type mastectomy is recommended. Complementary treatment is based on radiotherapy of the chest wall and lymph node chains, which reduces the risk of locoregional recurrence. Because of the more established hormone dependence of this tumour, its general treatment calls for additive hormone therapy, both in the treatment of metastases and as a preventive measure in stages II and III. The role of chemotherapy is still unclear, but the protocols applied in women can be extrapolated to men.
The prognosis of male breast cancer is identical to that of women at the same stage, dominated by size, stage, tumour grade and histological lymph node invasion, on which the therapeutic strategy must be based.
Reference
- Speirs V, Shaaban AM. The rising incidence of male breast cancer. Breast Cancer Res Treat. 2008 May; 115(2):429–30. [PubMed.]
- Giordano SH, Cohen DS, Buzdar AU, Perkins G, Hortobagyi GN. Breast carcinoma in men: a population-based study. Cancer. 2004; 101(1):51–7. [PubMed.]
- El Mhabrecha H, Neji H, Stita W, et al. Male breast cancer: similarities or differences with female breast cancer. Elsevier Masson. 2014. [Ref.]
- Slimani KA, Debbagh A, Sbitti Y, Errihani H, Ichou M. Cancer du sein chez l’homme au Maroc: épidémiologie et facteurs pronostiques. À propos de 140 cas. Elsevier Masson. 2016. [Ref.]
- Bourhafour M, Belbaraka R, Souadka A, M’rabti H, Tijami F, Errihani H. Male breast cancer: a report of 127 cases at a Moroccan institution. BMC Res Notes. 2011 Jun 29; 4:219. [PubMed.]
- Korde LA, Zujewski JA, Kamin L, Giordano S, Domchek S, Anderson WF, et al. Multidisciplinary meeting on male breast cancer: summary and research recommendations. J Clin Oncol. 2010 Apr; 28(12):2114–22. [PubMed.]
- Brinton LA, Key TJ, Kolonel LN, et al. Prediagnostic sex steroid hormones in relation to male breast cancer risk. J Clin Oncol. 2015 Jun; 33(18):2041–50. [PubMed.]
- Fiala L, Coufal O, Fait V, Foretova L, et al. Male breast cancer: our experience. Rozhl Chir. 2010; 89(10):612–8. [PubMed.]
- Karlsson CT, Malmer B, Wiklund F, Gronberg H. Breast cancer as a second primary in patients with prostate cancer—estrogen treatment or association with family history of cancer? J Urol. 2006; 176:538–43. [PubMed.]
- Contesso G, Mathieu MC, Guinebretiere JM. Anatomie pathologique des cancers du sein. Rev Prat. 1998; 48:29–35. [PubMed.]
- Esteller M, Silva JM, Dominguez G, et al. Promoter hypermethylation and BRCA1 inactivation in sporadic breast and ovarian tumors. J Natl Cancer Inst. 2000; 92:564–9. [PubMed.]
- Gordon DJ, Chin KH, Budny PG, Taylor AR. Male breast cancer in World War II aviation: a case report and review. Breast. 2003; 12:156–7. [PubMed.]
- Giordano SH, Hortobagyi GN. Leuprolide acetate plus aromatase inhibition for male breast cancer. J Clin Oncol. 2006; 24:42–3. [PubMed.]
- Shi A, Georgian-Smith D, Cornell DL, Rafferty A, Staffa E, Hughes MK, Kopans DB. Male breast mass with calcifications. AJR Am J Roentgenol. 2005; 185:S205–13. [PubMed.]
- Zhu J, Davis CT, Silberman S, Spector N, Zhang T. A role for the androgen receptor in the treatment of male breast cancer. Crit Rev Oncol Hematol. 2016 Feb; 98:358–63. [PubMed.]
- Oger A-S, Boukerrou M, Cutuli B, Campion L, Rousseau E, et al. Le cancer du sein chez l’homme: approche épidémiologique, diagnostique et thérapeutique: étude multicentrique rétrospective à propos de 95 cas. Gynécologie Obstétrique Fertilité. 2015. [Ref.]
- Gennari R, Curigliano G, Jereczek-Fossa BA, et al. Male breast cancer: a special therapeutic problem. Anything new? Int J Oncol. 2004; 24:663–70. [PubMed.]