>Corresponding Author : Benhadouga Khadija
>Article Type : Case Report
>Volume : 5 | Issue : 6
>Received Date : 30 June, 2025
>Accepted Date : 10 July, 2025
>Published Date : 14 July, 2025
>DOI : https://doi.org/10.54289/JCRMH2500127
>Citation : Benhaddouga K, Fatima ZC, Elhodaigui N, Monkid H, Assal A, et al. (2025) Incomplete hydatidiform mole: a case report. J Case Rep Med Hist 5(6): doi https://doi.org/10.54289/JCRMH2500126
>Copyright : © 2025 Benhadouga K, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Case Report | Open Access | Full Text
1Resident Physician, Department of Gynecology and Obstetrics, at Ibn Rochd University Hospital, Casablanca, Morocco
2Professor in the Department of Gynecology and Obstetrics at the Ibno Rochd University Hospital in Casablanca, Morocco
*Corresponding author: Benhadouga Khadija, Resident Physician, Department of Gynecology and Obstetrics, at Ibno Rochd University Hospital, Casablanca, Morocco
Abstract
Molar pregnancies are part of a group of diseases classified as gestational trophoblastic diseases.
For any woman of childbearing age presenting with abnormal vaginal bleeding, an hCG assay should always be carried out and, if elevated, a pelvic ultrasound should be performed. Non-molar pregnancy (normal intrauterine pregnancy, ectopic pregnancy and spontaneous abortion) is the most likely diagnosis, but hydatidiform mole should always be considered.
Molar pregnancy is now diagnosed and managed earlier, thanks to the systematic use of ultrasound in all pregnant patients.
Post-molar pregnancies have an extremely variable course, ranging from repeated abortions, stillbirths, premature births, live births, or reproducing in other molar pregnancies.
Keywords: Incomplete Hydatidiform Mole, Pregnancy, BhCG
Abbreviations: HCG: Human Chorionic Gonadotropin
Introduction
Hydatidiform mole is a rare gynecological disease of the trophoblast, which can be classified as a complete or incomplete mole pregnancy, with an incidence of between 0.6 and 11.5 per 1000 deliveries worldwide [1-3].
Complete hydatidiform mole occurs when an enucleated ovum is fertilized by two spermatozoa or one duplicated haploid spermatozoon; partial hydatidiform mole occurs when a haploid ovum is fertilized by two spermatozoa or one duplicated spermatozoon [4].
The most frequent clinical manifestation is metrorrhagia and increased uterine size with abnormal human chorionic gonadotropin (HCG) levels for gestational age [5].
Histological study is the gold standard of diagnosis, and endovaginal ultrasound is a useful tool in the diagnostic algorithm, showing typical snowflake and grape cluster features in the absence of a clear embryonic structure [6].
Diagnosis is often accidental after aspiration curettage, which is the treatment of first choice [7].
Case Report
This is a 34-year-old patient, IIG IP (1 live child by caesarean section), with a history of undocumented congenital blindness, admitted to our facility for first-trimester metrorrhagia with emission of vesicles during a pregnancy of 18 weeks of amenorrhoea and 02 days.
Clinical examination: patient conscious, hemodynamically and respiratorily stable, with speculum examination: gravid cervix + minimal bleeding of endo-uterine origin. The rest of the examination was unremarkable.
Pelvic ultrasound: Incomplete hydatidiform mole in an evolving monofetal pregnancy estimated at 18 weeks' amenorrhea and 02 days (Figures 1-2-3-4).
Laboratory results: Hb:10.4 Lc:8760 pq:230 000 PT:98% APTT:28,3 Fg:4,18 BhCG:50 000
Due to heavy bleeding, a caesarean section was performed to save the mother's life, giving birth to a stillborn baby of undetermined sex, birth weight: 150g (Figure 5).
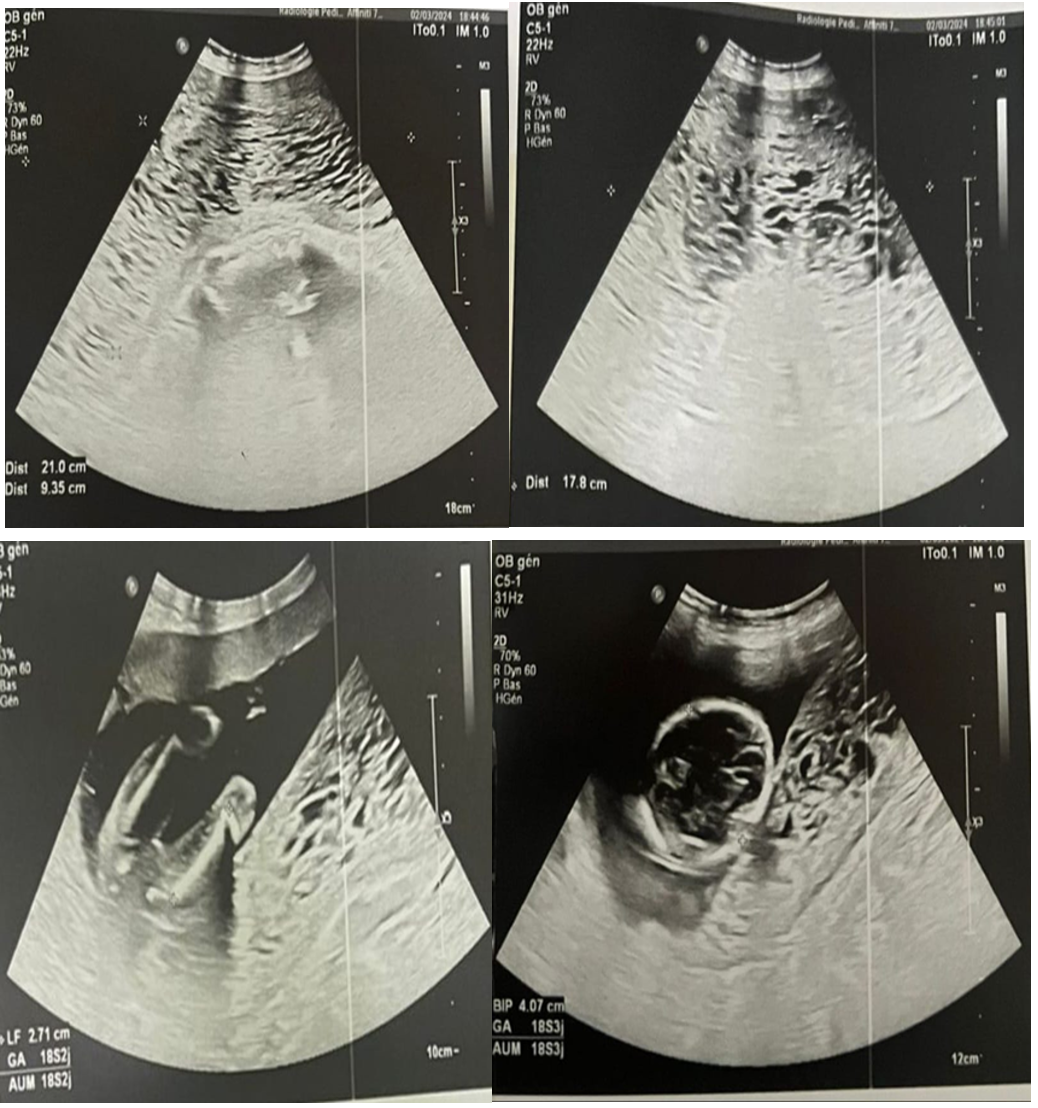
Figure 1,2,3,4: Sonographic appearance of incomplete hydatidiform mole in a pregnancy estimated at 18 weeks of amenorrhea + 02 days

Figure 5: Stillborn + incomplete hydatidiform mole
Discussion
The spectrum of gestational trophoblastic diseases includes benign forms such as hydatidiform mole, and malignant forms such as choriocarcinoma, invasive mole, epithelioid trophoblastic tumor and placental site trophoblastic tumor. All malignant forms are referred to as gestational trophoblastic neoplasia, the most common form of gestational trophoblastic disease being hydatidiform mole, also known as molar pregnancy [8].
Hydatidiform mole results from abnormal fertilization and is classified as complete or incomplete on the basis of differences in distinct pathological processes with cytogenetic, histological and clinical features [8].
The incidence of hydatidiform mole varies according to geographical region, and is generally thought to be higher in developing countries. Incidence is higher in young people under 20 and over 40, as well as in nulliparous women, pregnant women of low economic status, and patients with diets deficient in protein and folic acid [9].
Partial molar pregnancy coexisting with a normal living fetus has been divided into three types: the most common type is a twin pregnancy with a normal fetus having a normal placenta and complete mole; the second type is a twin pregnancy with a normal fetus and placenta and partial mole; and the third and rarest type is a single normal fetus with a partial molar placenta [10].
Vaginal bleeding occurred in 90% of our patients, anemia in 51%, hyperemesis gravidarum in 29%, increased uterine size beyond that expected for gestational age in 62%, small uterine size for dates in 12%, increased ovarian size in 27%, bilateral in 72% and unilateral in 28% [11,12].
The availability of ultrasound scans and the estimation of serum BhCG have contributed to early diagnosis and patient follow-up.
Diagnosis is often accidental after aspiration curettage, which is the treatment of first choice [7]. Non-conservative management including hysterectomy and bilateral salpingectomy is indicated if there is no desire for fertility, while chemotherapy is recommended for ectopic disease according to international guidelines [13].
Conclusion
In conclusion, in every case of suspected molar pregnancy for a normal fetus, it is necessary to counsel the patient appropriately and to ensure strict follow-up during and after pregnancy to detect the risk of persistence of trophoblastic pathology [14].
Reference
- Lin M., Chen J., Liao B., et al. When a vesicular placenta meets a live fetus: case report of twin pregnancy with a partial hydatidiform mole. BMC Pregnancy Childbirth. 2021; 21:694. [PubMed.]
- Bracken MB., Brinton LA., Hayashi K. Epidemiology of hydatidiform mole and choriocarcinoma. Epidemiol Rev. 1984; 6:52–75. [PubMed.]
- Lurain JR. Gestational trophoblastic disease I: epidemiology, pathology, clinical presentation and diagnosis of gestational trophoblastic disease., and management of hydatidiform mole. Am J Obstet Gynecol. 2010; 203(6):531–9. [PubMed.]
- Yuk JS., Baek JC., Park JE., et al. Incidence of gestational trophoblastic disease in South Korea: a longitudinal, population-based study. PeerJ. 2019; 7:e6490. [PubMed.]
- Simms-Stewart D., Mcdonald G., Fletcher H., et al. A review of molar pregnancy at theuniversityhospitaloftheWestIndiesover a16-yearperiod. J Obstet Gynaecol. 2013; 33(3):298–300. [PubMed.]
- Abdi A., Stacy S., Mailhot T., et al. Ultrasound detection of a molar pregnancy in the emergency department. West J Emerg Med. 2013; 14(2):121–2. [PubMed.]
- Cavaliere A., Ermito S., Dinatale A., et al. Management of molar pregnancy. J Prenat Med. 2009; 3(1):15–7. [PubMed.]
- Abu-Rustum NR., Yashar CM., Bean S., et al. Gestational trophoblastic neoplasia, Version 22019, NCCN Clinical Practice Guidelines in Oncology. J Natl Compr Canc Netw. 2019; 17(11):1374–91. [PubMed.]
- Mulisya O., Roberts DJ., Sengupta ES., et al. Prevalence and factors associated with hydatidiform mole among patients undergoing uterine evacuation at Mbarara Regional Referral Hospital. Obstet Gynecol Int. 2018. [PubMed.]
- Atuk FA., Basuni JBM. Molar pregnancy with normal viable fetus presenting with severe pre-eclampsia: a case report. J Med Case Rep. 2018. [PubMed.]
- Grimes DA. Epidemiology of gestational trophoblastic disease. Am J Obstet Gynecol. 1984; 150(3):309-18. [PubMed.]
- Akinkugbe A. Incidence and malignancy rate in hydatidiform molar pregnancy in Ile-lfe. Nig Med J. 1976. [Ref.]
- Worley MJ., Joseph NT., Berkowitz RS., Goldstein DP. Women with a partial mole during their first pregnancy and diagnosed earlier in gestation are at increased risk of developing gestational trophoblastic neoplasia. Int J Gynecol Cancer. 2014; 24(5):941-5. [PubMed.]