>Corresponding Author : Benhadouga Khadija
>Article Type : Case Report
>Volume : 5 | Issue : 5
>Received Date : 30 June, 2025
>Accepted Date : 10 July, 2025
>Published Date : 14 July, 2025
>DOI : https://doi.org/10.54289/JCRMH2500125
>Citation : Benhadouga K, Abdouni A, Zein M, Cheikh, Benchrefi Y, et al. (2025) Primary Neuroendocrine Neoplasms of the Breast: Case Report and Review of the Literature. J Case Rep Med Hist 5(5): doi https://doi.org/10.54289/JCRMH2500125
>Copyright : © 2025 Benhadouga K, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Case Report | Open Access | Full Text
1Resident Physician, Department of Gynecology and Obstetrics, at Ibn Rochd University Hospital, Casablanca, Morocco
2Professor in the Department Mohammed VI Oncology Centre, University Hospital Center Ibn Rochd, Casablanca , Morocco
*Corresponding author: Benhadouga Khadija, Resident Physician, Department of Gynecology and Obstetrics, at Ibno Rochd University Hospital, Casablanca, Morocco
Abstract
Neuroendocrine breast tumors represent a rare subtype of breast cancer, accounting for less than 1% of all neuroendocrine neoplasms. Starting from their pathology definition, and going through their prevalence, prognosis and treatment, our knowledge is still really uncertain.
In the present short review of the medical literature on this topic, we have evaluated their epidemiology, pathogenesis, pathology, clinical presentation, radiographic aspects, prognosis, and therapy. Our ultimate aim was actually to try to understand whether neuroendocrine neoplasms of the breast can be considered a definite clinical entity and if neuroendocrine differentiation of breast tumors has a really clinical relevance.
Keywords: Neuroendocrine carcinoma, Breast cancer, Case report, Chromogranin
Abbreviations: Nens: Neuroendocrine Neoplasms, BIRADs: Breast Imaging Reporting and Data System, SBR: Scarff–Bloom–Richardson, CT: Computed Tomography, NSE: Neuron-Specific Enolase, Pnets: Primary Neuroendocrine Tumors of the Breast, Nets: Neuroendocrine Tumors
Introduction
Neuroendocrine neoplasms (NENs) of the breast are rare, accounting for less than 1% of all invasive breast cancers, although the reported incidence varies largely due to the lack of standardized diagnostic criteria [1].
These tumors were initially described by Cubilla [2] in 1977.
Neuroendocrine neoplasms (NENs) are a group of heterogeneous tumors deriving from neuroendocrine cells. Neuroendocrine cells are scattered around the body. Therefore, NENs have been reported to arise in multiple sites, such as central nervous system, respiratory tract, larynx, gastrointestinal tract, thyroid, skin, breast, and urogenital system [3].
In the more recent WHO classification published in 2019, BNEN can only be identified only when the proportion of neuroendocrine cells in samples is greater than 90% [4] at present, they do not identify a definite clinical entity, and no specific prognosis or therapy have been recognized yet.
Case Report
A 45-year-old in periods of reproductive activity, with no medical history presented with inflammatory signs in the right breast with no nipple discharge, her disease history dates back one year, The rest of the physical examination was normal.
Mammography (Fig. 1) and a breast ultrasound showed a diffuse edematous infiltration of the right breast associated with ductal ectasia with diffuse skin thickening and homolateral axillary ADP assessed as Breast Imaging Reporting and Data System (BIRADS) 5
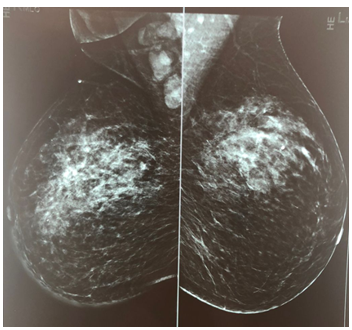
Figure 1: Mammographic profile showing a diffuse edematous infiltration of the right breast associated with ductal ectasia with diffuse skin thickening and homolateral axillary ADP
A biopsy of the breast was performed and disclosed the diagnosis of an invasive breast neuroendocrine carcinoma, partially necrotic graded as Scarff–Bloom–Richardson (SBR) II. At immunohistochemical analysis, Hormonal receptors were highly expressed (estrogen receptors, 80%; progesterone receptors, 60%), the Ki-67 proliferation index was 40 % and Her2/neu was negative.
A thoracoabdominal computed tomography (CT) scan and bone scintigraphy imaging showed a left clavicular and left iliac hyperfixation.
She subsequently received of neoadjuvant chemotherapy with eight cycles (4 courses of taxanes and 4 courses of anthracyclines AC60) with a good clinical course and a clear regression of the tumor.

Figure 2: clinical breast image before chemotherapy
Radical mastectomy and axillary lymph node resection were performed. A histopathological examination a showed the presence of a carcinoma large-cell neuroendocrine breast carcinoma, graded as Scarff–Bloom–Richardson (SBR) III , The surgical margins were negative ; with endovascular emboli , and with 5% of carcinoma in situ with intermediate nuclear grade, without comedonecrosis, There were ten metastatic lymph nodes with capsular invasion and endolymphatic emboli (10 N +/15 N). At immunohistochemical analysis, tumor cells stained positive with synaptophysin; chromogranin, cytokeratin, and neuron-specific enolase (NSE). Hormonal receptors were highly expressed, the Ki-67 proliferation index was 1% and Her2/neu was negative.

Figure 3: clinical breast images after chemotherapy she received adjuvant hormonotherapy with an antiestrogen un anti-estrogène (Tamoxifen 20 mg daily) for 10 months and radiotherapy. She is on regular follow-up at our cancer center
Discussion
Primary neuroendocrine tumors of the breast (PNETs) are a rare entity, accounting for less than 1% of all breast tumors [5]. Their rarity makes their diagnosis, classification and management particularly complex. Since they were first described in 1977 by Cubilla and Woodruff [6], diagnostic criteria have evolved, notably with WHO recommendations in 2003, 2012 and more recently in 2019.
The diagnosis of TNEPS is based on morphological and immunohistochemical criteria. Histologically, these tumors present organoid, trabecular or rosette-like structures, similar to those of gastroenteropancreatic neuroendocrine tumors [7]. Expression of neuroendocrine markers such as synaptophysin, chromogranin A and CD56 is essential to confirm neuroendocrine character [8]. However, a variable proportion of classical breast carcinomas may express these markers focally, hence the importance of combining morphological and immunohistochemical data to make the diagnosis [9].
The main differential diagnosis includes breast metastases of neuroendocrine tumors of other localizations, notably pulmonary or digestive. Rigorous clinico-radiological correlation and the search for associated breast carcinoma in situ are fundamental to confirm the primary mammary origin [10].
The subtyping of NETs according to the 2019 WHO classification now distinguishes between well-differentiated neuroendocrine tumors (NETs), poorly differentiated neuroendocrine carcinomas (small- or large-cell), and nonspecific breast carcinomas with neuroendocrine differentiation. This classification provides a better correlation with prognosis and guides treatment strategies [11].
Therapeutic management is based primarily on the same principles as those applied to other breast cancers, notably surgery and radiotherapy. However, the frequent expression of hormone receptors (ER+/PR+) in these tumors suggests a good response to hormone therapy [12]. Chemotherapy is generally reserved for poorly differentiated or metastatic forms, although the efficacy of somatostatin analogues or targeted therapies remains poorly defined in the absence of specific clinical trials [13].
The prognosis of TNEPS remains controversial. Some studies suggest a prognosis similar or even better than that of conventional breast carcinomas, particularly in the case of well-differentiated tumours [14]. Other reports indicate aggressive behavior, especially in poorly differentiated forms, with an increased risk of recurrence and metastasis [15].
Due to the rarity of TNEPS, the available data come mainly from retrospective series or isolated cases, underlining the need for specific registries and multicenter studies to better understand this entity, refine prognostic criteria and define appropriate therapeutic protocols.
Conclusion
Neuroendocrine tumors of the breast are rare tumors; they can be primary or secondary. Histopathological analysis is the only way to achieve their correct diagnosis by using appropriate immunohistochemical staining. Studies including larger series are needed in order to understand the biological behavior of breast neuroendocrine tumors.
Translational research and clinical trials dedicated to these rare entities in order to improve their long-term prognosis.
Reference
- Rakha EA., Reis-Filho JS., Sasano H., Wu Y. Neuroendocrine neoplasms. In: WHO Classification of Tumors Editorial Board (eds) WHO classification of tumours, 5th edn, Breast Tumours. IARC Press, Lyon, France. 2019;155–161. [Ref.]
- Cubilla AL., Woodruff JM. Primary carcinoid tumor of the breast. A report of 8 patients. Am J Surg Pathol. 1977;1:283–92. [Ref.]
- Oronsky B., Ma PC., Morgensztern D., Carter CA. Nothing But NET: A Review of Neuroendocrine Tumors and Carcinomas. Neoplasia. 2017;19(12):991–1002. [PubMed.]
- WHO Classification of Tumours. Breast Tumours. 5th Edition. Lyon., France: IARC. 2019. [Ref.]
- Sapino A., Papotti M., Righi L., et al. Neuroendocrine differentiation in breast carcinomas: a review of 51 cases. Virchows Arch. 2001;439(1):16–23. [PubMed.]
- Cubilla AL., Woodruff JM. Primary carcinoid tumor of the breast: a report of eight patients. Am J Surg Pathol. 1977;1(3):283–292. [Ref.]
- Bussolati G., Badve S., Sapino A. Breast carcinomas with neuroendocrine features. Pathology. 2016;48(5):495–502. [PubMed.]
- Ogawa H., Nishio A., Satake H., et al. Neuroendocrine tumor in the breast. Radiat Med. 2008;26(1):28–32. [PubMed.]
- Rakha EA., Tan PH., Varga Z., et al. Prognostic significance of neuroendocrine differentiation in breast carcinoma: a study of 359 cases. Breast Cancer Res Treat. 2017;151(2):337–348. [Ref.]
- Adams RW., Dyson P., Barthelmes L. Neuroendocrine breast tumours: breast cancer or neuroendocrine cancer presenting in the breast? Breast. 2014;23(2):120–127. [PubMed.]
- WHO Classification of Tumours Editorial Board. WHO Classification of Tumours: Breast Tumours. 5th ed. IARC. 2019. [Ref.]
- Günhan-Bilgen I., Zekioglu O., Ustun EE., Memis A., Erhan Y. Neuroendocrine differentiated carcinomas of the breast: imaging features correlated with clinical and histopathological findings. Eur Radiol. 2003;13(4):788–793. [PubMed.]
- Liu Y., Wei W., Wang K., et al. Primary neuroendocrine breast carcinoma: a retrospective analysis of 27 cases. Cancer Med. 2020;9(7):2459–2469. [PubMed.]
- Zhang Y., Chen Z., Bao Y., et al. Primary neuroendocrine breast carcinomas: a retrospective analysis of 126 cases in China. Pathol Res Pract. 2020;216(2):152746. [Ref.]
- Sapino A., Righi L., Cassoni P., et al. Expression of neuroendocrine markers in nonneuroendocrine breast carcinomas: a study of 345 cases. Virchows Arch. 2003;442(5):421–428. [Ref.]