>Corresponding Author : Salma Addi
>Article Type : Case Report
>Volume : 5 | Issue : 5
>Received Date : 23 June, 2025
>Accepted Date : 02 June, 2025
>Published Date : 07 July, 2025
>DOI : https://doi.org/10.54289/JCRMH2500123
>Citation : Addi S, Chyate F, Bensouda M, Assal A, Gotni A, et al. (2025) OHVIRA Syndrome in a 13-Year-Old Girl: A Case Report and Literature Review. J Case Rep Med Hist 5(5): doi https://doi.org/10.54289/JCRMH2500123
>Copyright : © 2025 Addi S, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Case Report | Open Access | Full Text
1Resident Physician, Department of Gynecology and Obstetrics, at Ibn Rochd University Hospital, Casablanca, Morocco
2Professor in the Department of Gynecology and Obstetrics at the Ibn Rochd University Hospital in Casablanca, Morocco
*Corresponding author: Salma Addi, Resident Physician, Department of Gynecology and Obstetrics, Ibno Rochd University Hospital, Casablanca, Morocco
Abstract
OHVIRA (Obstructed Hemivagina and Ipsilateral Renal Anomaly) syndrome, or Herlyn-Werner-Wunderlich syndrome, is a rare malformation of the female reproductive tract combining a didelphic uterus, obstructed hemivagina and homolateral renal agenesis. It usually manifests at puberty as cyclical pelvic pain and severe dysmenorrhea. Diagnosis is based on imaging, in particular MRI, which enables precise evaluation of pelvic structures. Treatment is surgical, based on resection of the obstructive vaginal septum.
We report a case of ohvira syndrome in a 13-year-old girl in the maternity ward at the abderrahim Harouchi university hospital in Casablanca.
Keywords: Ohvira Syndrome, Congenital Malformation, MRI
Abbreviations: OHVIRA: Obstructed Hemivagina and Ipsilateral Renal Anomaly, MRI: Magnetic Resonance Imaging
Introduction
OHVIRA (Obstructed Hemivagina and Ipsilateral Renal Anomaly) syndrome, also known as Herlyn-Werner-Wunderlich syndrome, is a rare congenital malformation resulting from an anomaly in the embryonic development of the Müller ducts and ureteral bud [1].
This pathology manifests mainly in adolescent girls at the time of puberty, causing cyclical pelvic pain, severe dysmenorrhea, even hematocolpos or hematometria [2].
Imaging plays a central role in diagnosis. While pelvic ultrasound may suggest the anomaly, magnetic resonance imaging (MRI) remains the gold standard for accurate visualization of utero-vaginal anatomy and identification of associated malformations [3]. Early surgical management, including resection of the obstructed vaginal septum, can help avoid long-term complications and improve patients' quality of life.
Case Report
This is a 13-year-old patient from a first-degree consanguinity marriage, with no particular pathological history, menarche at the age of 12, presenting with cyclic pelvic pain with progressive and disabling dysmenorrhea unrelieved by Tier 1 analgesics, as well as a sensation of pelvic heaviness, with no urinary signs and no cycle disorders.
On clinical examination, there was slight hypogastric tenderness with no palpable mass, normal external genitalia and a normally perforated annular hymen.
On pelvic ultrasound
Didelphic uterus visualized, site of significant hematometry in the right cavity with presence of a posterior median fluid formation suggestive of hematocolpos, absence of visualization of the kidney or right (Figure 1).
With pelvic MRI
Bicervical bicornuate uterus with a right hemi uterus increased in size of fluid content with hematometry, hematocolpos, hematosalpinx, and a hematocervix with a blind right hemivagina associated with right renal agenesis, the left hemi uterus is high situated, retroflexed, retroverted, well-differentiated, of normal size and regular contours, the site of an endo-cavitary retention of liquid signal, communicating with the vaginal wall via a small pertus, 15 mm in maximum diameter, corresponding to an elongated cervix (Figure 2-3).
Biological workup
Hemoglobin: 10.8, White blood cells: 3700, Platelets: 431000
Hemostasis and renal function correct, ferritinemia: 3
Vaginal evacuation of the hematocolpos with cure of the vaginal septum, and hysteroscopic exploration of the two uterine hemi-cavities: returned normal (Figure 4-5).

Figure 1: Ultrasound image of a didelphic uteruswith significant right hematoma
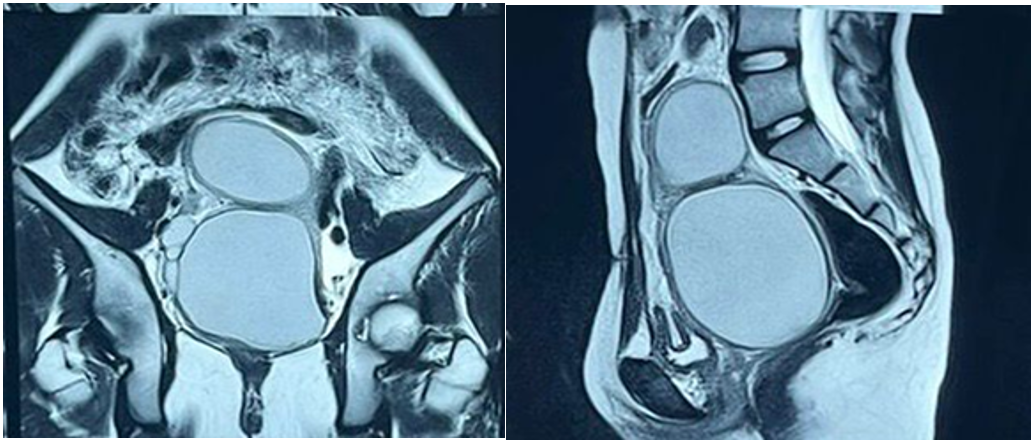
Figure 2-3: Pelvic MRI showing a bicornuate uterus with extensive hematocolposis

Figure 4-5: Intraoperative perineal view of hematocolpos evacuation with curettage of the vaginal septum.
Discussion
The OHVIRA (Obstructed Hemivagina and Ipsilateral Renal Anomaly) syndrome, although rare, represents an important clinical entity to recognize in gynecological and pediatric practice, due to its diagnostic, therapeutic and prognostic implications. Diagnosis of this syndrome is often delayed, on average several months to years after the onset of symptoms, which exposes patients to an increased risk of complications such as endometriosis, recurrent genital infections or impaired fertility [1].
The classic clinical picture includes cyclical pelvic pain onset at puberty, dysmenorrhea resistant to the usual treatments, and occasionally a palpable pelvic mass secondary to hematocolposis. However, atypical presentations, notably asymptomatic or discovered incidentally during an infertility or amenorrhea work-up, have also been reported [2]. Ipsilateral renal agenesis, often discovered on imaging, can be a valuable clue in orienting the diagnosis in symptomatic adolescent girls [3].
Magnetic resonance imaging (MRI) remains the reference modality for confirming the diagnosis. It allows precise visualization of uterine structures, the vaginal septum and the associated renal anomaly, while excluding other complex müllerian malformations [4].
Pelvic ultrasound can be used as a first line procedure, but is often insufficient on its own to establish a definitive diagnosis.
Treatment is based on surgical resection of the obstructive vaginal septum, usually vaginally. This procedure restores normal menstrual drainage and rapidly improves symptoms. In cases where the operation is performed early, reproductive function is generally preserved, and long-term gynaecological complications can be avoided [5]. Studies have shown that the fertility of patients with OHVIRA syndrome, once treated, is comparable to that of the general population, although cases of premature delivery and caesarean section are more frequent in this population due to the particular uterine anatomy [6].
Clinically, general practitioners, pediatricians, radiologists and gynecologists need to be made more aware of this syndrome. Any adolescent presenting with severe dysmenorrhea, hematocolpos, or isolated renal agenesis should undergo a targeted work-up in search of a utero-vaginal malformation. Early recognition and prompt management of this syndrome are essential to avoid complications that are sometimes serious, but perfectly avoidable.
Conclusion
OHVIRA syndrome, although rare, should be systematically evoked in the presence of any association of severe dysmenorrhea, pelvic pain at puberty, and unilateral renal anomaly. Multidisciplinary management, including gynecologists, radiologists and urologists, is essential for rapid diagnosis and optimal management. MRI is the key examination for establishing the exact topography of malformations. Early surgical intervention usually resolves symptoms and preserves fertility. Raising awareness of this syndrome would help reduce the still frequent delays in diagnosis and significantly improve the long-term prognosis of patients.
Conflict of interest: No conflict of interest
Bibliography
- A Zarfati., M C Lucchetti., et al. OHVIRA (Obstructed Hemivagina and Ipsilateral Renal Anomaly or Herlyn-Werner-Wunderlich syndrome): Is it time for age-specific management. J Pediatr Surg. 2022;57(11):696‑701. [PubMed.]
- H Mondelaers. Abord chirurgical du syndrome OHVIRA-like: une vidéo didactique. ISGE Consulté le. 2025. [Ref.]
- S Gholoum., P S Puligandla., T Hui., W Su., E Quiros., J M Laberge., et al. Management and outcome of patients with combined vaginal septum., bifid uterus, and ipsilateral renal agenesis (Herlyn-Werner-Wunderlich syndrome). J Pediatr Surg. 2006;41(5):987‑992. [PubMed.]
- J Tong., L Zhu., J Lang., et al. Clinical characteristics of 70 patients with Herlyn-Werner-Wunderlich syndrome. Int J Gynaecol Obstet. Off Organ Int Fed Gynaecol Obstet. 2013;121(2):173‑175. [PubMed.]
- R Del Vescovo., et al. Herlyn-Werner-Wunderlich syndrome: MRI findings., radiological guide (two cases and literature review)., and differential diagnosis. BMC Med Imaging. 2012;12(4). [PubMed.]
- P K Heinonen. Clinical implications of the didelphic uterus: long-term follow-up of 49 cases. Eur J Obstet Gynecol Reprod Biol. 2000;91(2):183‑190. [PubMed.]