>Corresponding Author : Salma Addi
>Article Type : Case Report
>Volume : 5 | Issue : 5
>Received Date : 17 June, 2025
>Accepted Date : 27 June, 2025
>Published Date : 02 July, 2025
>DOI : https://doi.org/10.54289/JCRMH2500121
>Citation : Addi S, Chyate FZ, Ezahraa TF, Benchrifi Y, Benhessou M, et al. (2025) Breast Tuberculosis in Women: A Case Report. J Case Rep Med Hist 5(5): doi https://doi.org/10.54289/JCRMH2500121
>Copyright : © 2025 Addi S, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Case Report | Open Access | Full Text
1Resident Physician, Department of Gynecology and Obstetrics, at Ibn Rochd University Hospital, Casablanca, Morocco
2Professor in the Department of Gynecology and Obstetrics at the Ibn Rochd University Hospital in Casablanca, Morocco
*Corresponding author: Salma Addi, Resident Physician, Department of Gynecology and Obstetrics, Ibno Rochd University Hospital, Casablanca, Morocco
Abstract
Mammary tuberculosis is a very rare pathology. The clinical presentations of this disease are multiple, often mimicking breast carcinoma.
It represents a diagnostic and therapeutic challenge.
We report here the case of a 34-year-old patient presenting with breast tuberculosis. The diagnosis was confirmed by histological study and the evolution was favorable under anti-bacillary treatment.
Keywords: Breast Tuberculosis, Differential Diagnosis, Antibacillary Treatment
Introduction
The prevalence of tuberculosis and its extra-pulmonary manifestations has increased considerably worldwide [1,2].
The mammary gland is a rare localization of tuberculosis [3,4]. It ranks last among the visceral localizations of tuberculosis, but it remains important to mention it, as it poses a problem of differential diagnosis with other benign or malignant mammary pathologies, notably breast abscess and breast cancer, due to the clinical similarities [5,6].
Only anatomopathological and bacteriological examinations can confirm the diagnosis and differentiate between breast abscess, cancer and tuberculosis [7].
Case Report
This is a 34-year-old patient with no specific pathological history, no history of tuberculosis infection, menarche at the age of 12, II gesture II pare with a history of exclusive breastfeeding, who presented with right mastodynia and nipple retraction.
Clinical examination: symmetrical breasts, retraction of the right nipple with no palpable mass, inflammatory signs or nipple discharge in both breasts, with free lymph nodes (figure 1).
On mammography: overdensity of the right breast compared with the contralateral side, with several confluent flaky opacities predominating in the upper-external quadrant and diffuse skin thickening of the right breast.
Left breast: absence of stellate opacity, absence of microcalcifications, absence of axillary opacities (figures 2 and 3).
On breast ultrasonography: diffuse dilatation of the right galactophore ducts, predominantly in the superolateral quadrant, with irregular contours and heterogeneous echogenic content with areas of posterior attenuation.
Two reshuffled and dedifferentiated right axillary adenopathies measuring 13.5 x 5.7mm and 4.9 x 8.7mm respectively. No tissue or cystic nodule in the left breast, with a free axillary fossa (figure 4): examination classified as ACR BI-RADS 4 on the right and ACR BI-RADS 1 on the left.
On breast MRI: regional reticular massless enhancement involving the outer quadrants associated with infiltration of the right mammary gland classified BI-RADS 4. Rather suspicious looking right axillary adenopathies (Figure 5 and 6).
Ultrasound-guided biopsy: tuberculoid granulomatous inflammation with patchy necrosis, compatible with progressive tuberculosis without signs of malignancy.
Chest X-ray was normal.
Extension workup revealed no other tuberculous foci.

Figure 1: Breast image (the arrow indicates retraction of the right nipple)
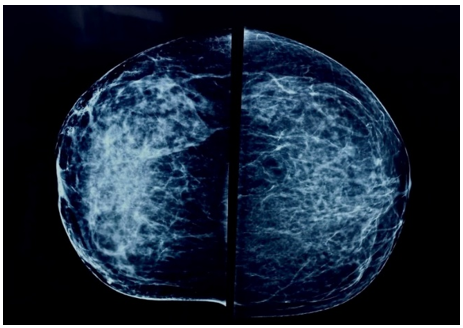
Figure 2: Bilateral craniocaudal view of the mammography

Figure 3: Bilateral mediolateral oblique view of the mammography

Figure 4: Ultrasoud image of the upper outer quadrant of the right breast

Figure 5: Breast MRI

Figure 6: Breast MRI
Discussion
Mammary tuberculosis generally affects young, multiparous and breast-feeding women.
In the literature, 95.5% of cases occur in women, and only 4.5% in men.
Its incidence in Western countries is less than 0.1%, whereas in developing countries, where tuberculosis is endemic, the incidence is between 0.25 and 4.5% [1,8].
According to previous reports in the literature, the symptoms of breast tuberculosis have generally been present for less than a year prior to diagnosis.
In addition, the disease mainly affects women of childbearing age and may represent the first manifestation of HIV infection. [9-11].
Nursing mothers are the most vulnerable, as the breast is more vascularized during lactation, with dilated ducts predisposed to trauma, making the organ more susceptible to tuberculosis infection [12,13].
Our patient reported having had her symptoms for less than a month, as well as being of childbearing age and not a carrier of HIV.
The diagnosis of breast tuberculosis is difficult due to nonspecific clinical and radiological findings. Tuberculous lesions such as nodular mastitis, disseminated mastitis and sclerosing lesions clinically mimic adenofibroma, carcinoma and fibrocystic change, depending on the mode of presentation. A young, multiparous, lactating woman presenting with a lesion should be carefully examined. Diagnostic modalities include mammography, fine-needle aspiration cytology and excisional biopsy, with respective accuracy rates of 14%, 12% and 60% [12].
Histopathology of the lesion contributes to the diagnosis, in the majority of cases, by identifying chronic granulomatous inflammation with caseous necrosis and Langhans-type giant cells [12], the method used in our case.
The main differential diagnosis to be considered is cancer, although other breast diseases, such as fat necrosis, plasmacytic mastitis, periareolar abscess, actinomycosis and blastomycosis [14].
The therapeutic management of mammary tuberculosis, according to the national tuberculosis control program, is generally based on conventional tuberculosis treatment, which is generally based on conventional quadritherapy (category III) combining isoniazid, rifampicin, ethambutol and pyrazinamide for two months, followed by isoniazid and rifampicin (six days apart), for four months [15] in complicated forms such as abscesses, persistent fistulas, large masses or suspected co-infection, antibacillary treatment may be extended for up to 9 months, depending on the course of the disease.
Surgical treatment is essentially a diagnostic tool, involving biopsies, excisions or lumpectomies, and drainage of suppurated collections, enabling histological diagnosis [16,17].
Moreover, in cases of resistance to anti-tuberculosis treatment or locally advanced disease, mastectomy may be proposed for therapeutic purposes [16-19].
At present, some authors recommend percutaneous drainage of the abscess under tomographic or ultrasound control [19].
Conclusion
Mammary tuberculosis is a rare extra-pulmonary localization of tuberculosis which can be difficult to diagnose. In countries where tuberculosis is endemic, this diagnosis should not be overlooked and should be considered in the light of certain clinical and radiological findings. In the absence of bacteriological certainty, pathological examination remains a key element of differential diagnosis. Breast cancer remains the main differential diagnosis to be ruled out.
References
- G Engin., B Acunaş., G Acunaş., M Tunaci. Imaging of extrapulmonary tuberculosis. Radiographics. 2000;20(2):471-488; quiz 529-532. [PubMed.]
- A N Chalazonitis., G Tsimitselis., J Tzovara., P Chronopoulos. Tuberculosis of the breast. Breast J. 2003;9(4):327-329. [PubMed.]
- A Ashturkar., A Bhosale., A Joshi., G Pathak. Primary tuberculosis of breast: A case series. Ann Trop. Med Public Health. 2012;5(3):262. [Ref.]
- T L Lin., S Y Chi., J W Liu., F F Chou. Tuberculosis of the breast: 10 years’ experience in one institution. Int J Tuberc. Lung Dis. 2010;14(6):758-763. [PubMed.]
- M Fadaei-Araghi., L Geranpayeh., S Irani., R Matloob., S Kuraki. Breast tuberculosis: report of eight cases. Arch Iran Med. 2008;11(4):463-465. [PubMed.]
- S Gon., A Bhattacharyya., B Majumdar., S Kundu. Tubercular mastitis - a great masquerader. Turk Patoloji Derg. 2013;29(1):61-63. [PubMed.]
- S T Dodiyi-Manuel., A Dodiyi-Manuel. Tuberculosis of the breast. Niger J, Med. 2013;22(1):72-74. [PubMed.]
- M R Al-Marri., A Almosleh., Y Almoslmani. Primary tuberculosis of the breast in Qatar: ten-year experience and review of the literature. Eur J Surg. 2000;166(9):687-690. [PubMed.]
- M Tewari., H S Shukla. Breast tuberculosis: diagnosis., clinical features & management. Indian J Med Res. 2005;122(2):103-110. [PubMed.]
- M Hartstein., H L Leaf. Tuberculosis of the breast as a presenting manifestation of AIDS. Clin Infect Dis. 1992;15(4):692-693. [Ref.]
- S H Harris., M A Khan., R Khan., F Haque., A Syed., M M Ansari. Mammary tuberculosis: analysis of thirty-eight patients. ANZ J Surg. 2006;76(4):234-237. [PubMed.]
- S R Shinde., R Y Chandawarkar., S P Deshmukh. Tuberculosis of the breast masquerading as carcinoma: a study of 100 patients. World J Surg. 1995;19(3):379-381. [PubMed.]
- S N Banerjee., N Ananthakrishnan., R B Mehta., S Parkash. Tuberculous mastitis: a continuing problem. World J Surg. 1987;11(1):105-109. [PubMed.]
- C Cohen. Tuberculous mastitis. A review of 34 cases. S Afr Med J. 1977;52(1):12-14. [PubMed.]
- Z Mnif., et al. Mastite tuberculeuse : aspects en imagerie à propos de 7 cas. Imag Femme. 2004;14(4):299-305. [Ref.]
- J Ben Hassouna., et al. Tuberculose mammaire: étude rétrospective de 65 cas. Gynécol Obstét Fertil. 2005;33(11):870-876. [PubMed.]
- S Luh., J Hsu., Y Lai., S Chen. Primary tuberculous infection of breast: experiences of surgical resection for aged patients and review of literature. J Zhejiang Univ Sci B. 2007;8(8):580-583. [PubMed.]
- R Khanna., G V Prasanna., P Gupta., M Kumar., S Khanna., A K Khanna. Mammary tuberculosis: report on 52 cases. Postgrad Med J. 2002;78(921):422-424. [PubMed.]
- C Romero., C Carreira., C Cereceda., J Pinto., R Lopez., F Bolaños. Mammary tuberculosis: percutaneous treatment of a mammary tuberculous abscess. Eur Radiol. 2000;10(3):531-533. [PubMed.]