>Corresponding Author : Errih Leila
>Article Type : Case Report
>Volume : 5 | Issue : 4
>Received Date : 08 April, 2025
>Accepted Date : 19 May, 2025
>Published Date : 11 June, 2025
>DOI : https://doi.org/10.54289/JCRMH2500119
>Citation : Younes B, Leila E, Ezzahra BF, Amina G, Mustapha B, et al. (2025) Adenoid Cystic Carcinoma of Bartholin's Gland: A Case Report. J Case Rep Med Hist 5(4): doi https://doi.org/10.54289/JCRMH2500119
>Copyright : © 2025 Younes B, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Case Report | Open Access | Full Text
1Resident Physician, Department of Gynecology and Obstetrics, at Ibno Rochd University Hospital, Casablanca, Morocco
2Professor in the Department of Gynecology and Obstetrics at the Ibno Rochd University Hospital in Casablanca, Morocco
*Corresponding author: Atlas I, Cardiology Department, Ibn Rochd hospital university, Casablanca, Morocco
Abstract
Adenoid cystic carcinoma of the Bartholin gland is a rare tumor representing 10-15% of Bartholin gland cancers, characterized by slow growth and unpredictable evolution. They pose a problem of differential diagnosis with Bartholin's gland cysts and abscesses. Treatment is based essentially on vulvectomy and inguino-femoral curage. We report a case of cystic adenoid carcinoma of Bartholin's gland discovered in a 38 year-old patient following a marsupliation indicated for a cyst of Bartholin's gland, which was treated by partial vulvectomy and bilateral inguino-femoral curage.
Keywords: Adenoid carcinoma, Tumor, Vulva, Bartholin, Vulvectomy
Abbreviations: BGC: Bartholinian Gland Carcinoma
Introduction
Bartholinian gland carcinoma (BGC) is an extremely rare malignant tumor. It accounts for less than 5% of vulvar carcinomas and less than 1% of all gynaecological cancers [1].
CGB can originate from either the canal or the vestibular.
The vestibular orifice of Bartholin's gland, or from the gland itself, giving rise to multiple histological subtypes including adenoid cystic carcinoma [2].
In this article, we report a case of cystic adenoid carcinoma of Bartholin's gland managed in the carcinological surgery department of the Mohamed VI center of CHU IBN ROCHD.
Case Report
A 38-year-old female patient with no previous history consulted a gynecologist for painful swelling of the left labia majora. A diagnosis of Bartholin's gland cyst was made and a left bartholinectomy was performed. Anatomopathological examination concluded to a cystic adenoid carcinoma of Bartholin's gland with invaded exeresis limits. The patient was referred to us for further management.
A pelvic mri was performed, which came back without any abnormalities.
The patient underwent a deep total vulvectomy and bilateral superficial inguino-femoral curage bringing back 6 reactive nodes.
The definitive anatomopathological study of the operative specimen revealed a poorly limited, infiltrating tumour proliferation measuring 5*2.5*1.5cm. After inclusion, the examination showed the presence of a carcinomatous focus arranged in guts with cystic cavities containing mucoid material.
Basal cells were flattened with eosinophilic cytoplasm.
The proliferation extended over 3 cm and was 4 mm from the superior border, 2 mm from the left border, 3 mm from the inferior border, 4 mm from the right border and 1 mm from the deep border. perineural sheathing was seen, with no vascular emboli.
This was consistent with a cystic adenoid carcinoma that had been completely removed. Given the unhealthy margins, the patient underwent radiotherapy.
Discussion
Primary Bartholin gland cancer was first documented in 1864 by Klob as a rare pathology representing 0.001% of all gynecological neoplasia [3]. The histological criteria confirming the primitive origin of carcinomas of this gland were established in 1897 by Honan: a deep labial primitive tumoral localization, the absence of adjacent skin lesions and the presence of tumoral glandular epithelial structures [4].
Cystic adenoid carcinomas of Bartholin's gland are characterized by their slow growth and tendency to peri-nervous invasion, which explains the frequency of pruritus and burning that may even precede tumor appearance. Dyspareunia, bleeding and ulceration are less frequent and non-specific signs [5].
In most cases, these carcinomas pose a differential diagnosis with cysts and abscesses, which are generally treated by drainage or marsupliation [6], raising the problem of exploration and therapeutic management of any mass developing at the expense of this gland in women in their forties [7].
At this age, some authors recommend a cytological study after preoperative or intraoperative puncture-aspiration of the mass, but the low diagnostic value of cytology makes biopsies after incision and drainage of abscesses, as well as complete excision of these cysts, the most reasonable approach to avoid delay in diagnosis of these carcinomas [8].
Bartholin adenoid cystic carcinoma contains glandular, myofiber, and epithelial components. Pathological examination shows that the tumor cells are round and uniform in size with deeply stained nuclei. The noncellular area contains mucin and hyaluronic acid with duct-like or glandular cavities. Sieve-like dilation and peripheral nerve infiltration are its main features [9].
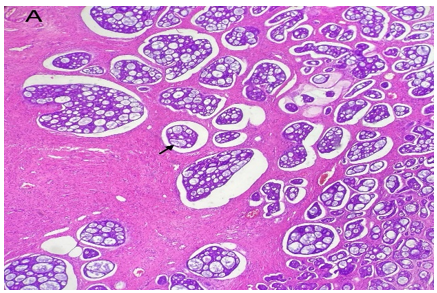
Figure 1: Hes x40 adenoid cystic carcinoma carcinomatous focus arranged in guts hollowed cystic cavities containing mucoid material (arrow)
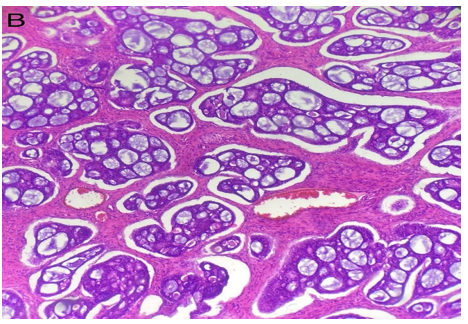
Figure 2: Hes x40 cribriform architecture
Surgical excision of Adenoid Cystic Carcinoma is associated with sentinel lymph node sampling for small tumors, or a deep inguinal lymphadenectomy for large or pN1 tumors [10]. According to the literature, inguinal lymph node status strongly affects patient survival [11]. However, whether unilateral or bilateral inguino-femoral lymphadenectomy or bilateral lymphadenectomy remains controversial; in view of the increased risk of contralateral lymph node involvement, which is proportional to tumour size, several authors recommend bilateral lymphadenectomy [12].
On the other hand the absence of clinical and radiological lymph node involvement, other authors suggest unilateral lymphadenectomy combined with adjuvant radiotherapy [13].
Regarding adjuvant treatment, it has been reported that less radical surgery combined with external radiotherapy is considered the best treatment for adenoid cystic carcinoma, providing good long-term survival and prevents complications [14].
Radiotherapy is recommended for patients with positive margins invasion and lymph node involvement. Chemotherapy is recommended for metastatic adenoid cystic carcinoma [11,13].
When the tumor is unresectable, or at the cost of significant mutilation, neoadjuvant treatment may be envisaged radio-chemotherapy or external radiotherapy and brachytherapy [15].
Adenoid cystic carcinoma of the bartholin gland is a slowly progressing tumour. Survival rates vary from author to author, ranging from 71% at 5 years, 59% at 10 years, and 18-2% in the case of metastasis [15]. It is therefore more appropriate to assess survival at 10-15 years [16].
Conclusion
The rarity of Bartholin's gland cancer means that its management is largely based on the more tried-and-tested management of median vulvar cancer.
There is a need for multicenter studies to provide high-level evidence on larger numbers of patients.
References
- Copeland LJ., Sneige N., Gershenson DM., McGuffee VB., Abdul-Karim F., Rutledge FN. Bartholin gland carcinoma. Obstet Gynecol. 1986;67(6):794–801. [PubMed.]
- Cardosi RJ., Speights A., Fiorica JV., Grendys Jr EC., Hakam A., Hoffman MS. Bartholin’s gland carcinoma a 15-year experience. Gynecol Oncol. 2001;82(2):247–51. [PubMed.]
- Klob JM. Pathologische anatomie der weiblichen Sexualorgane. W Braumüller. 1864. [Ref.]
- Masterson JG., Goss AS. Carcinoma of Bartholin gland. Review of the literature and report of a new case in an elderly patient treated by radical operation. Am J Obstet Gynecol. 1955;69(6):1323–1332. [PubMed.]
- Yang S-YV., Lee J-W., Kim W-S., Jung K-L., Lee S-J., Lee J-H., et al. Adenoid cystic carcinoma of the Bartholin’s gland: report of two cases and review of the literature. Gynecol Oncol. 2006;100(2):422–425. [PubMed.]
- Chamlian DL., Taylor HB. Primary carcinoma of Bartholin’s gland: A report of 24 patients. Obstet Gynecol. 1972;39(4):489–494. [PubMed.]
- DePasquale SE., McGuinness TB., Mangan CE., Husson M., Woodland MB. Adenoid cystic carcinoma of Bartholin’s gland: a review of the literature and report of a patient. Gynecol Oncol. 1996;61(1):122–125. [PubMed.]
- Frable WJ., Goplerud DR. Adenoid cystic carcinoma of Bartholin’s gland diagnosis by aspiration biopsy. Acta Cytol. 1975;19(2):152–153. [PubMed.]
- Hou JL., Wu LY., Zhang HT., et al. [Clinicopathological characteristics of six patients with adenoid cystic carcinoma of the Bartholin gland]. Zhonghua Zhong Liu Za Zhi. 2010;32(4):290–293. [PubMed.]
- Van der Zee AGJ., Oonk MH., De Hullu JA., et al. Sentinel node dissection is safe in the treatment of early-stage vulvar cancer. J Clin Oncol. 2008;26(6):884–9. [PubMed.]
- 11. C Mazouni., P Morice., P Duvillard., et al. Contralateral groin recurrence in patients with stage I Bartholin’s gland squamous cell carcinoma and negative ipsilateral nodes: report on two cases and implications for lymphadenectomy. Gynecol Oncol. 2004;94(3):843–5. [PubMed] [PubMed.]
- R J Cardosi., A Speights., J V Fiorica., et al. Bartholin’s gland carcinoma: a 15-year experience. Gynecol Oncol. 2001;82(2):247–251. [PubMed.]
- L J Copeland., N Sneige., D M Gershenson., et al. Adenoid cystic carcinoma of Bartholin gland. Obstet Gynecol. 1986;67(1):115–120. [PubMed.]
- O Balat., C L Edwards., L Delclos. Advanced primary carcinoma of the Bartholin gland: report of 18 patients. Eur J Gynaecol Oncol. 2001;22(1):46–9. [PubMed.]
- Z Chraibi., T Hebert., et al. Cancer de la glande de Bartholin. Gynécologie Obstétrique & Fertilité. 2014;42:540–542. [Ref.]
- H Mansouri., I Ben Safta., et al. Carcinome adénoïde kystique de la glande de Bartholin A propos d’un cas. Journal of Dental and Medical Sciences. 2018;17(10):51–53. [PubMed.]