>Corresponding Author : Atlas I
>Article Type : Case Report
>Volume : 5 | Issue : 4
>Received Date : 23 April, 2025
>Accepted Date : 23 April, 2025
>Published Date : 02 June, 2025
>DOI : https://doi.org/10.54289/JCRMH2500118
>Citation : Atlas I, Mounssif A, Megzari M, Bouziane M, Haboub M, et al. (2025) Spontaneous Coronary Dissection: An Unusual Etiology of Acute Coronary Syndrome. J Case Rep Med Hist 5(4): doi https://doi.org/10.54289/JCRMH2500118
>Copyright : © 2025 Atlas I, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Case Report | Open Access | Full Text
Cardiology Department, Ibn Rochd hospital university, Casablanca, Morocco
*Corresponding author: Atlas I, Cardiology Department, Ibn Rochd hospital university, Casablanca, Morocco
Abstract
Spontaneous coronary dissection is a rare condition characterized by a non-traumatic tear in the wall of a coronary artery, with no atherosclerotic or traumatic cause. It mainly affects women and is an infrequent but significant cause of acute coronary syndrome. In this article, a clinical case is presented of a 47-year-old woman with no previous cardiovascular history, presenting with acute chest pain. Investigative findings, including an electrocardiogram, elevated troponin levels and echocardiography, pointed towards an acute coronary syndrome due to coronary dissection.
The discussion highlights the rare nature of this condition, mainly seen in women, and points out that it may be associated with pregnancy in a small proportion of cases. Clinical presentation varies from asymptomatic to severe complications such as sudden death. Diagnosis is usually confirmed by coronary angiography, with a specific classification for types of dissection. The article also discusses treatment options, highlighting the lack of consensus on optimal management. Drug treatments are aimed at reducing thrombus formation, while coronary revascularization may be considered in some cases, although this is associated with increased risks of complications.
In conclusion, coronary dissection is a rare but significant cause of acute coronary syndrome, especially in young women. Diagnosis relies on coronary imaging, with invasive imaging techniques used in cases of doubt. Management requires an individualized approach, in the absence of a clear consensus on best practice.
Keywords: Spontaneous, Coronary Artery, Dissection, Etiology, Acute Coronary Syndrome
Abbreviations: IVUS: Intravascular Ultrasound, OCT: Optical Coherence Tomography
Introduction
Spontaneous coronary dissection is defined as a non-traumatic, non-atherosclerotic, unprovoked tear in the wall of a coronary artery following an intimal tear or spontaneous hemorrhage [1]. It predominantly affects women [1], and accounts for 0.1 to 4% of the etiologies of coronary syndromes [2].
We report the case of a young woman who presented with acute coronary syndrome following spontaneous coronary dissection.
Case Presentation
We describe the case of a 47-year-old female patient, with no particular pathological history and no cardiovascular risk factors, who presented to the emergency department of our facility with acute chest pain, evolving for 18 hours, retrosternal and constrictive, non-radiating, with no other associated functional signs. Clinical examination on admission revealed a neurologically conscious patient, normotensive to 127/78 mmHg, normocardial to 82 bpm, with normal oxygen saturation and temperature.
The ECG performed (Figure 1) within 10 minutes of the consultation showed a regular sinus rhythm at 85bpm, a fixed PR space at 0.12 seconds, and fine QRS at 0.08 seconds. There was a discrete ST-segment depression in the septo-apico-lateral and inferior regions, with an St segment elevation in the AVr region.

Figure 1: Image of the electrocardiogram.
A troponin assay was ordered, which came back positive at 592 ng/L (for a normal value of less than 35). The rest of the biological work-up, including a blood count, hemostasis and electrolyte balance with renal, liver, lipid and thyroid function tests, came back normal. The diagnosis was a non-ST-segment elevation myocardial infarction, based on chest pain, electrical signs and elevated troponins.
On transthoracic echocardiography (Figure 2), the left ventricle was non-dilated, non-hypertrophied and of good contractility, with an LVEF of 58% in Simpson biplane. Filling pressures of the left ventricle were not elevated, and there was no significant mitro-aortic valve disease nor indirect evidence of pulmonary hypertension. The right ventricle was non-dilated and of good function, with a dry pericardium, a normalcaliber aorta and non-dilated, compliant inferior vena cava.
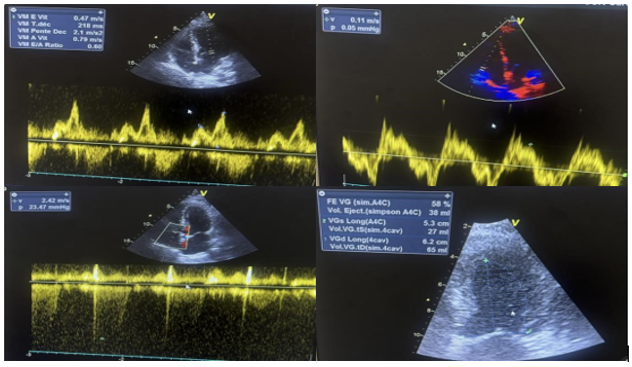
Figure 2: Images of the echocardiogram with no significant abnormalities.
The patient subsequently underwent coronary angiography (Figure 3), which revealed a coronary network with no significant lesions and a dissection of the second marginal.
Therapeutically, the patient was put on Aspirin 100mg/d and Atenolol 100mg/d.

Figure 3: Caudal coronary angiography showing dissection of the second margin (red arrow).
Discussion
Coronary artery dissection is a rare but potentially serious etiology of acute coronary syndromes. In angiographic studies, its prevalence has been estimated at 0.1-1.1% [3].
According to studies [1], spontaneous coronary dissections predominantly affect women, with a prevalence ranging from 81% to 92%, and among women under 50 with ACS, the prevalence of SCAD is reported to be as high as 8.7% [4]. In the same vein, it has been reported that pregnancy and peripartum account for only a small proportion of coronary dissections, around 10% in most studies [5]. In some studies, it has been reported that fibromuscular dysplasia, an arteriopathy that can cause stenosis, dissections or aneurysms, is associated with spontaneous coronary dissections in around 60% of cases, and an etiological work-up may be requested if associated dysplasia is suspected [6].
In terms of clinical presentation, it can range from asymptomatic to sudden death, with the majority presenting with a clinical picture of acute coronary syndrome. Case series including spontaneous coronary dissections suggest that it presents as STEMI in 48% of cases, as NSTEMI in 36% and as unstable angina in 6.5% [7]. Like acute coronary syndromes, dissections can be complicated by ventricular rhythm disturbances, cardiogenic shock or sudden death [8]. The severity of the dissection depends essentially on its location and extent.
In the majority of cases, coronary angiography is used to establish the diagnosis. Once the diagnosis has been confirmed, the angiographic type of dissection must be determined. The classification of Saw and AL [9] describes the angiographic signs that are adopted and help to confirm the diagnosis of coronary dissection. Coronary dissections most often affect the middle and distal parts of the coronary arteries, with the anterior interventricular artery the most affected, the left common trunk only in around 2% of cases, and multiple involvement in a quarter of cases [2].
If diagnostic doubt persists, two techniques can be used: intravascular ultrasound (IVUS) or optical coherence tomography (OCT), the latter being more effective. Non-invasive imaging, essentially coroscanner and cardiac MRI, is not very sensitive in the case of coronary dissection, and is therefore not the imaging technique of first choice in the event of dissection [3]. That said, non-invasive imaging can be used for accurate assessment of coronary dissections.
In terms of treatment, there is no informed consensus or recommendations for the management of these coronary dissections. There is no specific medical treatment, but antiplatelet agents and anticoagulation can be used, as in the case of atherosclerotic acute coronary syndrome, to reduce thrombus formation in the false channel [10]. Beta-blockers can be useful in reducing parietal vascular stress, and statins are prescribed in the presence of dyslipidemia or coronary lesions, even if insignificant [11].
Coronary revascularization by angioplasty or bypass may be proposed but should be reserved for patients with persistent ischemia and favorable anatomy [12]. Some authors [13] report that revascularization in the setting of a coronary dissection is correlated with high rates of failure, recurrence or complications. Coronary dissections generally have a good prognosis, with 10-year survival rates in excess of 90% [14].
Conclusion
Coronary dissections are a relatively rare etiology of acute coronary syndromes. They mainly affect young women and generally have a good prognosis. Positive diagnosis relies on coronary angiography, sometimes coupled with invasive imaging techniques in certain doubtful situations. There is no consensus on management, which is discussed on a case-by-case basis.
References
- Saw J., Aymong E., John Mancini GB., Tara S., Andrew S., Donald R. Nonatherosclerotic coronary artery disease in young women. Can J Cardiol. 2014;30(7):814‒819. [PubMed.]
- Hassan S., Prakash R., Starovoytov A., Saw J. Natural history of spontaneous coronary artery dissection with spontaneous angiographic healing. JACC Cardiovasc Interv. 2019;12:518‒527. [PubMed.]
- Alfonso F., Bastante T., Rivero F., Cuesta J., Benedicto A., Saw J., et al. Spontaneous coronary artery dissection. From diagnosis to management. Circ J. 2014;78(9):2099‒110. [PubMed.]
- Saw J. Spontaneous coronary artery dissection. Can J Cardiol. 2013;29(9):1027‒33. [PubMed.]
- Elkayam U., et all. Pregnancy-associated. Acute myocardial infarction: a review of contemporary experience in 150 cases between 2006 and 2011. Circulation. 2014;129:1695‒1702. [PubMed.]
- Saw J., Starovoytov A., Humphries K., et al. Canadian spontaneous coronary artery dissection cohort study: in-hospital and 30-day outcomes. Eur Heart J. 2019; 40:1188‒97. [PubMed.]
- Wonnacott D., Berringer R. Dissection spontanée de l’artère coronaire: Rapport de cas et revue de la littérature. Can Fam Physician. 2016;62(12):e721‒e723. [PubMed.]
- Hill SF., Sheppard MN. Nonatheerosclerotic coronary artery disease associated with sudden cardiac death. Heart. 2010;96:119‒25. [PubMed.]
- Saw J. Coronary angiogram classification of spontaneous coronary artery dissection. Catheter Cardiovasc Interv Off J Soc Card Angiogr Interv. 2014;84(7):1115‒22. [PubMed.]
- D’Ovidio C., Sablone S., Carnevale A. Spontaneous coronary artery dissection: case report and literature review. J Forensic Sci. 2015;60(3):801‒806. [PubMed.]
- Alfonso F. Spontaneous coronary artery dissection: new insights from the tip of the iceberg? Circulation. 2012;12:667‒670. [PubMed.]
- Vrints CJM. Spontaneous coronary artery dissection. Heart. 2010;96:801‒808. [PubMed.]
- Tweet MS., Eleid MF., Best PJM., et al. Spontaneous coronary artery dissection revascularization versus conservative therapy. Circ Cardiovasc Interv. 2014;7(6):777‒786. [PubMed.]
- Giacoppo D., Capodanno D., Dangas G., Tamburino C. Spontaneous coronary artery dissection. Int J Cardiol. 2014;175(1):8‒20. [PubMed.]