>Corresponding Author : Bouyalik Fadwa
>Article Type : Case Report
>Volume : 5 | Issue : 3
>Received Date : 01 April, 2025
>Accepted Date : 14 April, 2025
>Published Date : 07 May, 2025
>DOI : https://doi.org/10.54289/JCRMH2500115
>Citation : Fadwa B, Leila E, Oumnia E, Bonga BM, Houssine B, et al. (2025) Primitive Fallopian Tube Tumor Without Ovarian Involvement (Case Report). J Case Rep Med Hist 5(3): doi https://doi.org/10.54289/JCRMH2500115
>Copyright : © 2025 Fadwa B, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Case Report | Open Access | Full Text
1Resident Physician, Department of Gynecology and Obstetrics, at Ibno Rochd University Hospital, Casablanca, Morocco
2Professor in the Department of Gynecology and Obstetrics at the Ibno Rochd University Hospital in Casablanca, Morocco
*Corresponding author: Bouyalik Fadwa, Resident Physician, Department of Gynecology and Obstetrics, Ibno Rochd University Hospital, Casablanca, Morocco
Abstract
Primitive fallopian carcinoma is rare; its frequency does not exceed 1% of gynecological cancers and its diagnosis is most often performed pre or post operative. we report a case of a 25-year-old patient, the patient presented a chronic pelvic, pain and the clinical examination was within normal limits. The Pelvic ultrasound revealed a bilateral cystic parauterine, mass and the CT scan performed has revealed two oval formations, well limited of regular contours hypodense without endocystic vegetations, CA125: 107 U/ml. A surgical excision (annexectomy) revealed invasive high-grade sero papillary adenocarcinoma and infiltration of the chorion. The treatment was followed by a complementary total hysterectomy.
Keywords: Cancer, Fallopian, Tumor, Adenocarcinoma
Introduction
Primitive tubal carcinoma is rare; its frequency does not exceed 1% of gynecological cancers and its diagnosis is most often performed pre or post operative [1]. Because of the proximity of the uterus and ovary, the diagnosis of primary cancer of the fallopian tube is very difficult to assert and is based on very rigid criteria: Presence of a macroscopic lesion in the fallopian tube, Absence of tumor of the ovary or uterus, or, if necessary, tumor of a histological type different from that of the uterus and ovary [2]. We report the case of an exceptional bilateral form of primitive tubal carcinoma without ovarian involvement.
Case Report
Our observation concerns a 25-year-old patient, mother of one child, with no pathological history, who consulted for chronic pelvic pain without other associated signs and in whom the examination was without particularity.
Pelvic ultrasound finds bilateral cystic parauterine mass on the right of 90x55mm and on the left of 70x50mm without peritoneal effusion (Figure 1). The abdominal and pelvic CT showed bilaterally two oval formations, well limited of regular contours hypodense without endocystic vegetations measuring 85x77mm and 69x54mm, these formations exert a mass effect on the cervico-isthmic uterine region with upstream fluid retention (Figure 2). The biological rate of CA125: 107U/ml. A surgical excision(annexectomy) that came back in favor of invasive high-grade sero papillary adenocarcinoma and the treatment was followed by a complementary total hysterectomy.
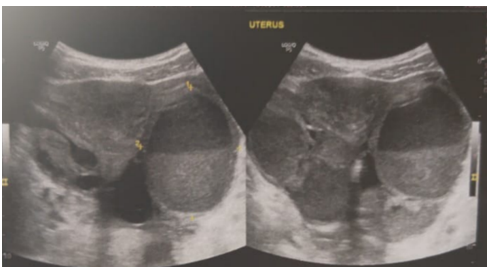
Figure 1: Pelvic ultrasound revealing a bilateral cyst.
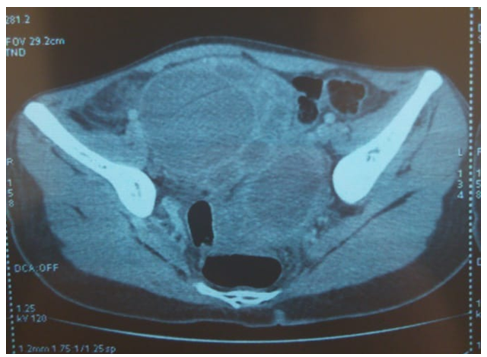
Figure 2: Abdominal and pelvic CT showing bilateral formations.
Discussion
Malignant tumors of the fallopian tube are rare and are dominated by adenocarcinomas. Borderline epithelial tumors of the fallopian tube are exceptional. They can be serous, mucinous or endometroidal [3].
Overall, the literature reports only about 1,200 cases and about 20 new cases each year. It is diagnosed between 19 and 85 years of age, mainly in the peri- and post-menopausal ages, in patients with a high incidence of sterility [4]. This is consistent with our patient who was 25 years old.
Inclusions of endometrial cell nests in the tubal epithelium are considered to be contributory factors of the tumor. These tumours are associated with pelvic inflammatory disease (salpingitis) and other tubal conditions such as tuberculosis, pseudoadenomatous hyperplasia and endometriosis, as well as benign and malignant uterine and ovarian tumours. Cancer can coexist with intra-uterine (even full-term) and extra-uterine pregnancy [4].
The cancer originates in the ampullary part of the endosalpinx and slowly invades the tubal light with luxuriant vegetations which, during the first phase of development, do not infiltrate the wall. It is bilateral in a quarter of cases and, when it is unilateral, it affects the right tube more frequently. It is possible that the two lesions are independent, as often the two tumors are of equal size and because the intertubal endometrium and peritoneum remain unharmed, but the remarkable frequency (30%) It is not possible to rule out that metastases are involved.
The caricatural clinical picture is constituted by the triad combining abdominal-pelvic pain, vaginal discharge (metrorragia, leucorrhoea or haematorhea) and a pelvic mass. In front of these symptoms, abdominal pelvic ultrasound is the key examination of the diagnostic approach and the discovery of a suspicious annexic mass leads to the realization of a pelvic MRI and, if necessary, a surgical exploration. However, the pre-operative diagnosis of cancer of the fallopian tube is difficult and a challenge for the sonographer because the incidence of this pathology, is low and its detection requires some ultrasound experience of the annexic masses. It is only performed in pre-operation in 0.3 to 15% of cases [5].
Usually, the tubal cancer is discovered per-operative during a laparotomy for initial suspicion of ovarian cancer or after the pathological examination of the operating parts, including the tubes. The diagnosis of primary tubal carcinoma is based on strict criteria:
- Endometrium not neoplastic or with superficial neoplastic grafts of a carcinoma compatible with a tubal origin.
- Non tumor ovaries or having at most a superficial neoplastic graft of much smaller size than the tubal tumor, having the same histological type and not included in a cystic formation
- Uterine tube macroscopically recognizable or after histological examination (thanks to the muscular tunics) interposing between the tumor and the ovary [6].
In more than 80% of patients with tubal cancer, the CA 125 rate is increased and, at the Immunohistochemical analysis of the surgical parts, 87% of the tumors are positive for CA 125 [7].
Given the scarcity of this type of tumour, its microscopic presentation, its immunohistochemical and genetic profile, its locoregional evolutionary profile, its response to treatment, clinicians are managing this tumour in the same way as ovarian tumours, including it even very often in common therapeutic trials. There is no specific prospective test for tubal carcinoma [8].
The basic intervention is the enlarged colpohysterectomy with lymphadenectomy, omentectomy and maximum cytoreduction in cases with strictly pelvic extension of multiple peritoneal biopsies (parietological gutters, diaphragm and viscera) and picking systemic lumbo-aortic ganglionic. Because of the risk of neoplastic transplants, conservative treatment would almost never be indicated in tubal cancer [2]. If it cannot be complete immediately, it will be performed after 3 or 4 neoadjuvant chemotherapy treatments [8].
Currently, post-operative radiation is no longer recommended due to the frequency of extra-pelvic relapses (more than half of patients treated with total abdominal radiation) and the importance of side effects. However, radiation therapy has maintained symptomatic palliative indications [8].
ROSEN, after comparing the survivals of patients with stages I and II of ova and tubal cancer, concluded that the latter had a more severe prognosis. Therefore, systemic adjuvant therapy is recommended [9].
Complete response rates observed with platinum salt chemotherapy ranged from 64% to 75% in patients with advanced stage or relapse of fallopian tube carcinoma. Baekelandt et al. administered chemotherapy combining paclitaxel (175 mg/m2) and carboplatin (AUC 6) to 8 patients with tubal cancer, including 4 naives of any chemotherapy that relapsed after at least 6 months without platinum salts. The overall response rate was 87%. There are currently no data on intraperitoneal chemotherapy in fallopian tube carcinoma [8].
The overall five-year survival of fallopian tube carcinomas is approximately 30-50% (about 40% in ovarian carcinomas). The classic factors of poor prognosis are: advanced stage (62-73% survival at 5 years for stage I versus 36-37% for stage II, 17-29% for stage III and 0-12% for stage IV) existence of a post-operative macroscopic residue > 2 cm, high age, significant preoperative CA125, relapse within the first six months after initial treatment.
Conclusion
Fallopian tube cancers are very rare and are only a small percentage of gynecological cancers. bilateral forms are even more exceptional. Diagnosis is difficult due to the proximity of the uterus and ovary and usually discovery intraoperatively. Its treatment and monitoring is similar to that of the ovary.
References
- Shneider C., Wight E., Perucchini D., Haller U., Fink D. Primary carcinoma of fallopian tube. A report of 19 cases and literature review. Eur J Gynaecol Oncol. 2000; 21:578–82. [PubMed.]
- Kasse A A., Deme A., Diop M., Fall M C., et al. Trunk Carcinomas About a case of bilateral papillary cancer and literature review. Black African Medicine 2000; 47:(8/9). [Ref.]
- Alvarado Cabrero I., Navani SS., Young RH., Scully RE. Tumors of the fimbriated end of the fallopian tube: a clinicopathologic analysis of 20 cases, including nine carcinomas. Int J Gynecol Patol. 1997; 16:189–96. [PubMed.]
- Nappi L and Nappi R. Tumors of the fallopian tube. Encycl Méd Chir (Editions Scientifiques et Médicales Elsevier SAS, Paris, all rights reserved), Gynaecology. 689-A-10. 2002;7. [Ref.]
- Balaya V., et al. Contribution of ultrasound in the pre–operative diagnosis of primary malignant tumors of the fallopian tube. J Gynecol Obstet Biol Reprod (Paris). 2015. [PubMed.]
- Philippe E., Charpin C. Gynaecological and obstetrical pathology. masson, paris. 1992;153–173. [Ref.]
- Hsu Y., Hung J., Yue C. Preoperative diagnosis of fallopian tube carcinoma by transvaginal sonography, MRI and CA125. Tzu Chi Med J. 2010; 22:225–8. [Ref.]
- P Boudou, P Morice., P Duvillard., P Pautier. Tumors of the fallopian tube. [Ref.]
- Rosen A., Sevelda P., Klein M., Graf A., Lahousen M., Reiner A., et al. A comparative analysis of the management and prognosis in stage I and II fallopian tube carcinoma and epithelial ovarian cancer. Br. J. Cancer. 1994; 69:577–79. [PubMed.]