>Corresponding Author : Bouyalik Fadwa
>Article Type : Case Report
>Volume : 5 | Issue : 3
>Received Date : 01 April, 2025
>Accepted Date : 14 April, 2025
>Published Date : 07 May, 2025
>DOI : https://doi.org/10.54289/JCRMH2500114
>Citation : Fadwa B, Leila E, Oumnia EB, Houssine B, Sakher M, et al. (2025) Breast Angiosarcoma (Case Report). J Case Rep Med Hist 5(3): doi https://doi.org/10.54289/JCRMH2500114
>Copyright : © 2025 Fadwa B, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Case Report | Open Access | Full Text
1Resident Physician, Department of Gynecology and Obstetrics, at Ibno Rochd University Hospital, Casablanca, Morocco
2Professor in the Department of Gynecology and Obstetrics at the Ibno Rochd University Hospital in Casablanca, Morocco
*Corresponding author: Bouyalik Fadwa, Resident Physician, Department of Gynecology and Obstetrics, Ibno Rochd University Hospital, Casablanca, Morocco
Abstract
Primary angiosarcoma (SA) of the breast is a rare neoplasia unrelated to radiation exposure. It represents less than 0.05% of all malignant tumors of the breast. This lesion is characterized by aggressive patterns and a poor prognosis, and by the absence of typical features on radiological examination. Currently, there are no evidence-based guidelines for surgical and adjuvant treatment for this tumor, although wide surgical resection followed by chemotherapy appears to improve disease-free and overall survival.
We report a case of primary angiosarcoma in 67-year-old women, without prior radiotherapy, treated with total mastectomy followed by radiochemotherapy.
Total mastectomy appears to be the only known treatment that proved useful. Adjuvant therapy has not been proven to date. The 5-year disease-free survival for first-year tumors can be as high as 76%, and as low as 15% for third-year tumors. Because of the rarity of these tumors, there is no standard therapeutic approach.
Keywords: Angiosarcoma, Breast, Tumor, Mastectomy
Abbreviations: AS: Angiosarcoma, MRI: Magnetic Resonance Imaging
Introduction
Primary breast sarcomas are rare conditions with histological heterogeneity. They are mainly represented by fibrosarcoma’s, angiosarcomas, myoxia/round cell liposarcomas, phyllodes tumors and malignant fibrous histiocytomas [1]. Angiosarcoma (AS) of the breast accounts for 1% of all mammary soft-tissue tumours. It originates in the connective tissue of the breast and may extend to the overlying skin [2]. AS can occur de novo with a median age at onset of 40 years or can be a secondary radiation treatment of an epithelial breast cancer with a median age at onset of 70 years (5 or 10 years after radiation therapy) [3-5].
The overall incidence rate of primary angiosarcomas is less than 0.05% of all malignant breast tumours. In 1907, Borrman described the first documented case of angiosarcoma of the breast [6]. Three main histopathological patterns have been described: type I, characterized by vascular channels invading the breast tissue with low endothelial proliferation; type II, showing features of papillary endothelial components; and type III, with evidence of endothelial components, necrosis and hemorrhage [7].
We report an observation of a mammary angiosarcoma in a woman, with discussion of the epidemiological, diagnostic and therapeutic aspects of this type of tumor.
Case Report
Mrs O.K, aged 67, with a history of osteoporosis complicated by a femoral neck fracture, had consulted for a swelling of the right breast evolving for 8 months associated with inflammatory signs and mastodynia. The breast examination revealed a 10 cm mass covering the entire right breast, soft, compressible and painful, with a purplish-angiomatous appearance of the skin opposite the tumour, no nipple discharge and no palpable adenopathy. The contralateral breast was normal (Fig 1 and 2). Mammography showed an increased pseudo-nodular opacity, with a watery tone of interest to the QSE, and no microcalcifications (Fig 3). Ultrasound revealed infiltration with thickening of the cellulo-fatty tissues of the breast, with no visible cystic or tissue formation, accompanied by frank hypervascularization on color Doppler. A surgical biopsy was performed. Histological examination revealed a high-grade type III breast angiosarcoma. A mastectomy was performed.
Figure 1 and 2: Breast examination revealing a 10 cm mass covering the entire right breast.
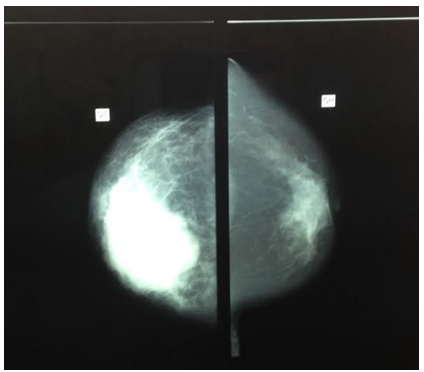
Figure 3: Mammography showing an increased pseudo-nodular opacity.
Discussion
Angiosarcoma of the breast is also known as hemangiosarcoma, hemangioendotheliosarcoma, hemangioblastoma, angioblastoma, malignant hemangioendothelioma. The first case was reported by Borman in 1907.
Angiosarcoma of the breast usually presents as a defined mass in the mammary parenchyma characterized by rapid growth. Large tumours can lead to thrombocytopenia and haemorrhagic manifestations (Kasabach-Merritt syndrome) [8].
Angiosarcoma imaging is not specific. The mammography or ultrasound studies do not show appropriate signs. AS could be diagnosed as a benign lesion, particularly in younger patients.
The most favorable imaging test is considered to be magnetic resonance imaging (MRI), which can show typical malignant signs (hyperintensity on T2 images and a rapid initial intense phase followed by washout) [9].
Fine-needle aspiration or needle biopsy is necessary for a definitive diagnosis [10].
In addition, immunohistochemistry can be useful in identifying CD31 endothelium, an indicator of vascular proliferation. Other specific markers for this type of lesion are factor VIII and FLI1 [11].
The standard treatment for patients with primary angiosarcomas of the breast is a modified radical mastectomy combined, where appropriate, with axial lymph node dissection. Patients with smaller tumours may benefit from breast-conserving surgery [12].
Rosen et al. presented a serie of 63 patients with primary angiosarcoma of the chest from Sloan Kettering Cancer Center; 35 patients underwent axillary lymph node dissection and only one had metastatic lesions [9].
In the available literature, there is no international consensus on the chemotherapy regimens to be used in patients with angiosarcoma. Soft-tissue sarcomas are known to be highly aggressive tumors: the probability of systemic recurrence is around 50%, even in localized disease [13]. Anthracycline-based chemotherapy leads to a significant improvement in disease-free and overall survival [14].
Adjuvant radiotherapy after surgery may be beneficial for breast sarcomas, particularly for patients with microscopically positive margins [15].
Rosen et al. used adjuvant radiotherapy in combination with chemotherapy in 17% of their patients, and radiation alone in 6% of their patients, with no improvement in disease-free or overall survival [9].
The prognosis of angiosarcoma of the chest, like every sarcoma histotype, is related to tumor size, tumor and resection margin status [16].
Conclusion
Primary angiosarcoma of the breast is a malignant vascular neoplasm that occurs in the mammary parenchyma with or without extension into the skin. It should be considered a different neoplasia from radiation-related SA. This neoplasia shows no pathognomonic signs on mammography or ultrasound examination and may present specific radiological features only on MRI. There are few series available analyzing the best option for surgical and adjuvant treatment for primary angiosarcoma of the breast.
An aggressive surgical approach seems to be accepted by most authors, but breast-conserving surgery may be proposed in some cases. Axillary clearance is not necessary in all patients, in fact, the tumor does not follow a lymphatic diffusion pattern; however, large masses invading the axilla require axillary lymph node dissection to obtain free margins.
Although some series show an increase in disease-free survival and overall survival, standard medical regimens in patients with angiosarcoma of the breast remain unclear. Adjuvant chemotherapy with Taxan agents has shown good results, but further research is needed.
References
- Adem C., Reynolds C., Ingle JN., Nascimento AG. Sarcome du sein primaire:séries clinicopathologiques de la Mayo Clinic et revue de la littérature. Fr J Cancer. 2004;91:237-241. [PubMed.]
- Liberman L., Dershaw DD., Kaufman RJ., Rosen PP. Angiosarcome du sein. Radiologie. 1992;183:e649-e654. [PubMed.]
- Lagrange JL., Ramaioli A., Chateau MC. Sarcoma après la radiothérapie. Radiologie. 2000;216:197-205. [PubMed.]
- Blanchard DK., Reynolds C., Grant CS., Farley DR., Donohue JH. Le sarcome du sein induit par rayonnement. Un m J Surg. 2002;184:356-358. [PubMed.]
- Huang J., Mackillop WJ. Risque accru de sarcome des tissus mous après la radiothérapie chez les femmes atteintes d’un carcinome du sein. Cancer. 2001;92:172-180. [PubMed.]
- Borrman R. Metastasenbildung bei histologish gutartigen geschwulsten:tombe von metastasierendem Angiom. Beitr. Pathol. Anat. 1907;40:372-393. [Ref.]
- Donnell RM., Rosen PP., Lieberman PH., Kaufman RJ., Kay S., Braun DW. Angiosarcome et autres tumeurs vasculaires du sein. Analyse pathologique comme guide de pronostic. Un m. J. Surg. Pathol. 1981;5:629-642. [PubMed.]
- Bernathova M., Jaschke W., Pechlahner C. Angiosarcome primaire du syndrome de Kasabach-Merritt associé au sein pendant la grossesse. Sein. 2006;15:255-258. [PubMed.]
- Rosen PP., Kimel M., Ernsberger D. angiosarcome mammaire. La signification pronostique de la différenciation tumorale. Cancer. 1988;62:2145-2151. [PubMed.]
- Bousquet G., Confavreux C., Magne N., de Lara CT., Poortmans P., Senkus E. Résultats et facteurs pronostiques dans le sarcome du sein:une étude multicentrique du réseau de cancer rare. Radiother. Oncol. 2007;85:355-361. [PubMed.]
- Hart J., Mandavilli S. Angiosarcome à l’épithélioïde:un bref examen diagnostique et un diagnostic différentiel. Cambre. Pathol. Laboratoire. Med. 2011;135:268-272. [PubMed.]
- Folpe AL., Chand EM., Goldblum JR. L’expression de Fli-1, facteur de transcription nucléaire., distingue les néoplasmes vasculaires des mimétiques potentiels. Un m J Surg Pathol. 2001;25:1061-1066. [PubMed.]
- Bennani A., Chbani L., Lamchahab M. Angiosarcome primaire de la poitrine: rapport de cas. Diagn Pathol. 2013;8:66. [PubMed.]
- Confavreux C., Lurkin A., Mitton N., Blondet R., Saba C., Ranchère D. Sarcomas et tumeurs malignes des phyllodes du sein – une étude rétrospective. EUR J Cancer. 2006;42:2715-2721. [PubMed.]
- Blanchard DK., Reynolds CA., Grant CS., Donohue JH Les sarcomes des seins nonphyloïdes primaires. Un m J Surg. 2003;186:359-361. [PubMed.]
- Sher T., Hennessy BT., Valero V., Broglio K., Woodward WA., Trent J. Angiosarcomes primaires de la poitrine. Cancer. 2007;110:173-178. [PubMed.]