>Corresponding Author : Sanaa Benrahhal
>Article Type : Case Report
>Volume : 5 | Issue : 2
>Received Date : 20 Jan, 2025
>Accepted Date : 11 Feb, 2025
>Published Date : 05 March, 2025
>DOI : https://doi.org/10.54289/JCRMH2500104
>Citation : Benrahhal S, Lyafi Y, Driss E, Moutaabide R, Mediani H, et al. (2025) The Torsion of the Sessile Hydatid of Morgagni. J Case Rep Med Hist 5(2): doi https://doi.org/10.54289/JCRMH2500104
>Copyright : © 2025 Benrahhal S, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Case Report | Open Access | Full Text
Department of Maternity, Centre Hospitalo Universitaire Elharouchi Casablanca Morocco Gynecologic Obstetric, Casablanca, Morocco
*Corresponding author: Sanaa Benrahhal, Department of Maternity, Centre Hospitalo Universitaire Elharouchi Casablanca Morocco Gynecologic Obstetric, Casablanca, Morocco
Case Report
The torsion of the sessile hydatid of Morgagni is a pathology that can occur when the hydatid is not directly inserted at its base and is associated with a pedicle [1,2]. There is a great variety of embryonic formations known as hydatids of Morgagni or Rosenmüller organs [3].
The sessile hydatid of Morgagni corresponds to the remnants of the Müllerian duct, presenting in the form of cysts [4]. The Müllerian duct refers to the structures present in the embryo that will give rise to the fallopian tubes and part of the vagina [5,6]. This remnant is located on the head of the epididymis or on an oviduct, another name for the fallopian tube, which connects the ovary to the uterus and allows the passage of the ovum released from the ovary [7,8].
We report the case of a 19-year-old female, single, with menarche at age 13, with no particular medical history, who presented to the emergency department with acute pelvic pain evolving over the past 3 days without any other associated signs. On examination, the patient was conscious (15/15 Glasgow), normotensive, normocardiac, and afebrile, with normally colored conjunctivae and abdominal tenderness with defense in the right iliac fossa, without gynecological bleeding.
Abdominal-pelvic ultrasound: minimal fluid collection in both iliac fossae. Abdominal-pelvic CT scan: well-defined, regular-edged, oval-shaped right lateral-uterine formation with a thin wall of liquid density, containing a fine septum measuring 40.5x30mm.
Biological work-up: Hb: 14.4, WBC: 10,220, Platelets: 237,000, CRP: 0.25, BHCG: negative, Urine culture: sterile.
Exploration findings: • Minimal peritoneal effusion (Figure1) • Presence of a torsion of a right bilobed hydatid of Morgagni due to 3 twists of necrotic appearance (Figure 2) • Detorsion and removal performed (Figures 2 and 3) • Presence of a ruptured functional right ovarian cyst, 6 cm, with yellow citrine fluid aspirated • Presence of a left pedunculated hydatid of Morgagni with the same appearance as the contralateral one, untwisted, removal of the latter + abundant saline lavage (Figure 1).
These formations must be recognized, as they can sometimes be mistaken for one or more follicles, a hydrosalpinx [9,10], or an ovarian cyst when they are large, or even a full bladder (and may go unnoticed in such cases) [11,12]. On ultrasound, it is the persistence of the image that should raise suspicion of the diagnosis. Laparoscopy is generally the only method to confirm the diagnosis. While small formations likely have no significant role, large ones can lead to mechanical infertility [13-16].

Figure 1
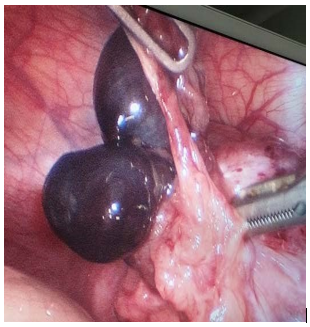
Figure 2

Figure 3
References
- Weitzman VN., DiLuigi AJ., Maier DB., et al. Prevention of recurrent adnexal torsion. Fertil Steril. 2008;90(5):2018. e1–3. [PubMed.]
- Oelsner G., Stockheim D., Soriano D., et al. Pregnancy outcome after laparoscopy or laparotomy in pregnancy. J Am Assoc Gynecol Laparosc. 2003;10(2):200–4. [PubMed.]
- Zanetta G., Mariani E., Lissoni A., et al. A prospective study of the role of ultrasound in the management of adnexal masses in pregnancy. BJOG Int J Obstet Gynaecol. 2003;110(6):578–83. [PubMed.]
- Kumari I., Kaur S., Mohan H., et al. Adnexal masses in pregnancy: a 5-year review. Aust N Z J Obstet Gynaecol. 2006;46(1):52–4. [PubMed.]
- Zweizig S., Perron J., Grubb D., et al. Conservative management of adnexal torsion. Am J Obstet Gynecol. 1993;168(6 Pt 1):1791–5. [PubMed.]
- Abu-Musa A., Nassar A., Usta I., et al. Laparoscopic unwinding and cystectomy of twisted dermoidcyst during second trimester of pregnancy. J Am Assoc Gynecol Laparosc. 2001;8(3):456–60. [PubMed.]
- Pansky M., Smorgick N., Herman A., et al. Torsion of normal adnexa in post menarchal women and risk of recurrence. Obstet Gynecol. 2007;109(2 Pt 1):355–9. [PubMed.]
- Tepper R., Zalel Y., Goldberger S., et al. Diagnostic value of transvaginal color Doppler flow in ovarian torsion. Eur J Obstet Gynecol Reprod Biol. 1996;68(1-2):115–8. [PubMed.]
- Djavadian D., Braendle W., Jaenicke F. Laparoscopic oophoropexy for the treatment of recurrent torsion of the adnexa in pregnancy: case report and review. Fertil Steril. 2004;82(4):933–6. [PubMed.]
- Jardon K., Bothschorisvili R., Rabischong B., et al. [How I perform an ovariopexy after adnexal torsion]. Gynécologie Obstétrique Fertil. 2006;34(6):529–30. [PubMed.]
- Lansac J., Goffinet F., Carbonne B., et al. [Recommendations for clinical practice: treatment of ovarian cysts presumed to be benign? Gynécologie Obstétrique Fertil. 2002;30(6):544–9. [PubMed.]
- Mathevet P., Nessah K., Dargent D., et al. Laparoscopic management of adnexal masses in pregnancy: a case series. Eur J Obstet Gynecol Reprod Biol. 2003;108(2):217–22. [PubMed.]
- Oelsner G., Cohen SB., Soriano D., et al. Minimal surgery for the twisted ischaemic adnexa can preserve ovarian function. Hum Reprod Oxf Engl. 2003;18(12):2599–602. [PubMed.]
- Boughizane S., Naifer R., Hafsa A., et al. [Laparoscopic management of adnexal tumors after the first trimester of pregnancy]. J Gynécologie Obstétrique Biol Reprod. 2004;33(4):319–24. [PubMed.]
- Graif M., Shalev J., Strauss S., et al. Torsion of the ovary: sono graphic features. AJR Am J Roentgenol. 1984;143(6):1331–4. [PubMed.]
- Dolgin SE., Lublin M., Shlasko E. Maximizing ovarian salvage when treating idiopathic adnexal torsion. J Pediatr Surg. 2000;35(4):624–6. [PubMed.]