>Corresponding Author : Ambadas Rathod
>Article Type : Case Report
>Volume : 5 | Issue : 1
>Received Date : 20 Dec, 2024
>Accepted Date : 06 Jan, 2025
>Published Date : 10 Jan, 2025
>DOI : https://doi.org/10.54289/JCRMH2500101
>Citation : Rathod A, Goyal S, SharmaP and Patle V. (2025) Seizures and Basal Ganglia Calcification Secondary to Hypoparathyroidism: Fahr Syndrome an Intriguing Presentation. J Case Rep Med Hist 5(1): doi https://doi.org/10.54289/JCRMH2500101
>Copyright : © 2025 Rathod A, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Case Report | Open Access | Full Text
1Junior Resident, Department of General Medicine, Government Medical College and Hospital, GMCH, Chandigarh
2Assistant Professor, Department of General Medicine, GMCH, Chandigarh
*Corresponding author: Ambadas Rathod, Junior Resident, Department of General Medicine, Government Medical College and Hospital, GMCH, Chandigarh
Abstract
Intracranial calcification can occur physiologically in some cases, typically without symptoms and is discovered incidentally through neuroimaging. However, pathological calcification in the basal ganglia is often caused by underlying conditions such as metabolic disorders, infections, and genetic diseases.
Here we present a 50-year-old male presented with multiple episodes of generalised tonic-clonic seizures. A brain CT scan revealed extensive symmetrical basal ganglia and periventricular calcification. Further testing showed low calcium levels, high phosphorus levels, and low parathyroid hormone levels, leading to a diagnosis of primary hypoparathyroidism and thereby Fahr Syndrome. The patient was initially treated with intravenous calcium gluconate and calcitriol, which resulted in significant clinical and laboratory improvements, effectively managing the condition and its symptoms.
Abbreviations: PTH: Parathyroid Hormone, GTCS: Generalised Tonic-Clonic Seizure, ECG: Electrocardiogram, BCS: Brain Calcinosis Syndrome, BGCs: Basal Ganglia Calcifications
Introduction
Primary hypoparathyroidism is a rare endocrine disorder characterized by low calcium levels (hypocalcaemia) due to insufficient or absent parathyroid hormone (PTH) production by the parathyroid glands.
Hypoparathyroidism can result from various causes, including congenital disorders, receptor insensitivity, surgical interventions, autoimmune conditions, radiation therapy, and infiltrative disorders, or it can be idiopathic [1].
If left undiagnosed or untreated, hypoparathyroidism can have serious consequences, including the development of renal disease, calcifications in the brain, seizures, neuropsychiatric disorders, and cataracts. However, with proper diagnosis and treatment, hypoparathyroidism is a manageable condition, and its potentially debilitating effects can be mitigated, emphasizing the importance of early detection and intervention [2].
Case Presentation
We report a case of a 50-year-old male who presented to the emergency department with complaints of generalised tonic-clonic seizure (GTCS) 4 episodes at home and each lasted for around 30 seconds to 60 seconds. There was no history of fever, headache, palpitations, vertigo, chest pain, difficulty in breathing, mood swings, constipation, diarrhoea, vomiting, neck surgery and head trauma. There was no family history of similar problems or autoimmune diseases.
On general physical examination patient was conscious, coherent and cooperative following commands. Vital signs were stable (BP- 110/70mm Hg, Respiratory Rate -16/minute, SpO2- 97% under room air and Random blood glucose levels-124 mg/dl). A tongue bite was present and there were no focal neurological deficits and no meningeal signs. Trousseau’s and Chvostek’s signs were positive and other systemic examination was normal.
Laboratory investigations suggested that calcium was low (normal range:8-10.4 mg/dl) and phosphorus was 6.8 mg/dl (Normal range:2.5-4.5 mg/dl). NCCT Brain showed Bilateral symmetrical calcifications in the Basal ganglia (Figure 1. A and Figure 1. B). The patient was loaded with the anti-epileptic drug sodium valproate. The patient was given Calcium Gluconate infusion of 10gm in 1000 ml of NS over 24 hrs, and Calcitriol. Close monitoring of Calcium levels was done and calcium levels improved gradually (As shown in Table 1). Further testing showed decreased Parathyroid Hormone (PTH) level (6.7 pg/ml, normal range 15-85 pg/ml), normal serum Vitamin D3, and serum magnesium levels. So, a diagnosis of primary hypoparathyroidism was made. The electrocardiogram (ECG) showed a prolonged QT interval (Figure 2). However, a subsequent echocardiogram showed normal heart function, dismissing concerns of ventricular dysfunction or structural abnormalities. Ultrasonography of the whole abdomen was done which was not suggestive of any calcifications. The ophthalmological evaluation showed no cataract.

Figure 1. Bilateral symmetrical calcifications in the Basal gangia

Figure 2. ECG- Showing prolonged QT interval
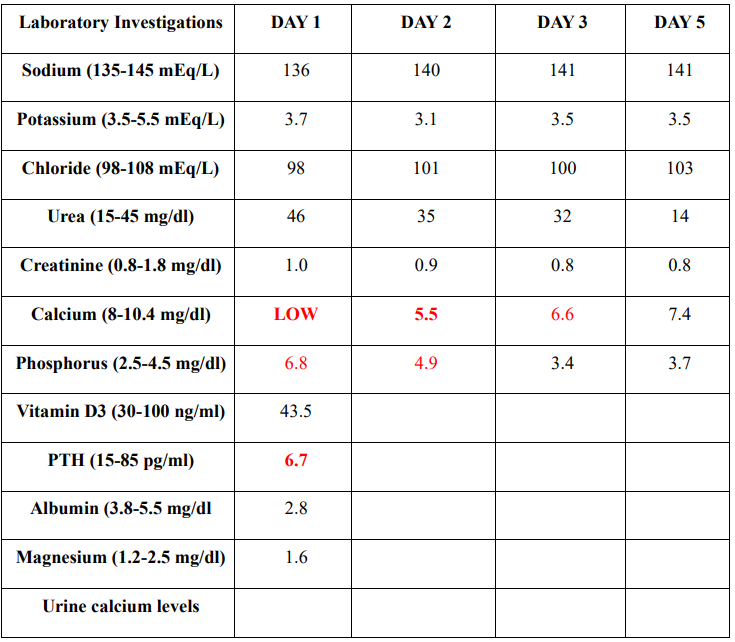
Table 1
After normalization of calcium levels patient was discharged on Tab calcium carbonate 1.5 grams/day and Tab Calcitriol 0.25 mg twice daily. He was advised to follow up on an OPD basis and the patient was reviewed after 2 weeks he was asymptomatic and seizure-free with normal calcium (8.6 mg/dl) levels.
Discussion
Primary hypoparathyroidism is marked by a deficiency in parathyroid hormone (PTH) production, leading to disrupted calcium balance and homeostasis. hypocalcaemia, hyperphosphatemia, and low or inappropriately normal PTH levels characterize hypoparathyroidism, all the features being fulfilled by our patient. The clinical presentation of this condition varies depending on the degree and rapidity of hypocalcemia onset, with more severe and rapid declines in calcium levels resulting in more pronounced symptoms. The severity and speed of hypocalcemia development dictate the range of clinical manifestations, which can range from mild to life-threatening, highlighting the importance of prompt diagnosis and treatment.
Acute hypocalcemia can lead to a range of severe symptoms, including respiratory distress characterized by laryngospasm, stridor, and airway obstruction. Neuromuscular manifestations are prominent, featuring numbness and tingling around the mouth, muscle cramps, spasms, and tetany. Hyperreflexia is a hallmark, often demonstrated by positive Trousseau's sign (carpal spasms) and Chvostek's sign (facial spasms). Additionally, acute hypocalcemia can cause cognitive impairment, cardiac arrhythmias, and prolongation of the QT interval, which can rarely progress to depressed systolic function and heart failure. In extreme cases, seizures may also occur, emphasizing the need for prompt recognition and treatment of this potentially life-threatening condition. Chronic hypocalcemia can lead to symptoms resulting from the deposition of ectopic calcium-phosphorus complexes. These symptoms may include extrapyramidal signs like parkinsonism, cognitive impairments such as dementia, and cerebellar dysfunction.
These conditions are typically associated with intracranial calcifications [2].
Our patient reported experiencing muscle spasms and seizures, symptoms commonly associated with hypoparathyroidism. Seizures in this condition are linked to hypocalcemia, which increases neuronal excitability by lowering the concentration of extracellular calcium [1].
Radiologically, hypoparathyroidism frequently leads to calcification, most often in the bilateral basal ganglia, with the globus pallidus being the most common site. Calcification can also appear in the cerebellum, subcortical white matter, corona radiata, and the thalamus. Movement disorders such as chorea or parkinsonism occur in 20–30% of patients with basal ganglia calcification, though some patients may remain asymptomatic [3].
Brain calcinosis syndrome (BCS) is typically characterized by the bilateral accumulation of calcium within the brain parenchyma, most commonly in the basal ganglia. Various terms have been used to describe this intracranial calcification, including basal ganglia calcification(s), Fahr syndrome, intracranial calcification, pallidal calcification, and striopallidodentate calcinosis [4].
The acute and long-term management of hypoparathyroidism should focus on maintaining serum calcium levels within the low-normal range, while keeping serum phosphorus levels in the high-normal range. It's crucial to avoid significant deviations in calcium levels, whether hypo- or hypercalcemia, to minimize symptoms and prevent serious complications such as cardiac arrhythmias and seizures. Long-term management also aims to prevent excessively high serum calcium levels, which can lead to complications like ectopic soft tissue deposition, nephrolithiasis, nephrocalcinosis, and kidney dysfunction issues often encountered in patients with hypoparathyroidism. Therefore, regular monitoring of vitamin D, phosphorus, and calcium levels, along with assessing renal calcium excretion, is essential [5].
Conclusion
This case report highlights the presence of basal ganglia calcifications (BGCs) on imaging should prompt further investigation for hypoparathyroidism, as early detection and timely intervention can significantly impact outcomes. Identifying and treating hypoparathyroidism early on can prevent long-term complications, emphasizing the need for a proactive approach to diagnosis and management. By doing so, healthcare providers can mitigate the risk of permanent damage and improve patient outcomes.
References
- Nageen T., Muhammad SZ., Jamal A. Seizures and Basal Ganglia Calcification Caused by Hypoparathyroidism. Cureus. 2020;29:12(4):e7888. [PubMed.]
- Mendes EM., Meireles-Brandão L., Meira C., Morais N., Ribeiro C., Guerra D. Primary hypoparathyroidism presenting as basal ganglia calcification secondary to extreme hypocalcemia. Clin Pract. 2018;8:8(1):1007. [PubMed.]
- Basak RC. A case report of Basal Ganglia calcification - a rare finding of hypoparathyroidism. Oman Med J. 2009;24(3):220-2. [PubMed.]
- Fulop M., Zeifer B. Case report: extensive brain calcification in hypoparathyroidism. Am J Med Sci 1991;302(5):292-295. [PubMed.]
- Bollerslev J., Rejnmark L., Marcocci C., Shoback DM., Sitges-Serra A., van Biesen W., Dekkers OM. European Society of Endocrinology. European Society of Endocrinology Clinical Guideline: Treatment of chronic hypoparathyroidism in adults. Eur J Endocrinol. 2015;173(2):G1-20. [PubMed.]