>Corresponding Author : Ziad Imane
>Article Type : Case Report
>Volume : 4 | Issue : 10
>Received Date : 11 June, 2024
>Accepted Date : 25 June, 2024
>Published Date : 03 Oct, 2024
>DOI : https://doi.org/10.54289/JCRMH2400155
>Citation : Ziad I, Tossi S, Elkaroini D, Boufettal H, Mahdaoui S, et al. (2024) Giant phyllode sarcoma: one case report. J Case Rep Med Hist 4(10): doi https://doi.org/10.54289/JCRMH2400155
>Copyright : © 2024 Ziad I, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Case Report | Open Access | Full Text
1Resident Physician, Department of Gynecology and Obstetrics, at Ibn Rochd University Hospital, Casablanca, Morocco
2Professor in the Department of Gynecology and Obstetrics at the Ibn Rochd University Hospital in Casablanca, Morocco
*Corresponding author: Ziad Imane, Resident Physician, Department of Gynecology and Obstetrics, at Ibn Rochd University Hospital, Casablanca, Morocco
Abstract
Malignant phyllodes tumor of the breast (MPTB) is a rare but distinct clinico-pathological entity representing <1% of all malignant tumors of the breast Malignant tumors are usually rhabdomyosarcoma and liposarcoma symptoms can mimic other types of breast carcinoma, particularly if the mass ulcerates and bleeds Surgery is the typical treatment of choice for MPTB, and radiotherapy is recommended for those at high risk of local recurrence. Chemotherapy is used to treat patients at high systemic metastatic risk. we report the case of a 27-year-old woman with a giant phyllode sarcoma.
Keywords: Malignant phyllodes tumor of the breast, Breast Cancer, giant phyllode sarcoma
Abbreviations: MPTB: Malignant phyllodes tumor of the breast; LCA: Leukocyte Common Antigen, SMA: Smooth Muscle Actin
Introduction
Malignant phyllodes tumor of the breast (MPTB) is a rare but distinct clinico-pathological entity representing <1% of all malignant tumors of the breast with an incidence of approximately 2.1 per million [1]. These tumors usually occur in women in the 4th or 5th decade of life. They can develop rapidly, and the associated symptoms can mimic other types of breast carcinoma, particularly if the mass ulcerates and bleeds. The bulk of this tumor is made up of connective tissue with mixed cystic and solid gelatinous areas [2]. Malignant tumors are usually rhabdomyosarcoma and liposarcoma rather than fibrosarcoma, and the number of mitoses may help in the diagnosis of the malignant subtype [3]. Surgery is the typical treatment of choice for MPTB, and radiotherapy is recommended for those at high risk of local recurrence. Chemotherapy is used to treat patients at high systemic metastatic risk [3]. The cut-off point for giant phyllodes tumor is 10 cm, this size presents management problems for the surgeon and given its rarity, decisions on treatment options are based on small-scale retrospective clinical trials or case reports. What was fascinating in our case was not just the initial presentation, but the aggressiveness of this phyllodes variation given bilaterality, recurrence and bone metastases.
Case Report
We present our patient that was aged 27 years old with pathological history of being followed for a high-grade phyllodes tumor of the left breast since 2019 with a second recurrence in 2021 having had a left mastectomy + axillary dissection and the anatomopathological study reveals a high-grade phyllodes tumor, 4 mm from the lower margin and remains distant from the others, 0N+/5N. Clinical examination revealed a bilobed mass covering the entire right breast, movable relative to the two planes, with no nipple discharge or inflammatory signs, and no axillary adenopathy (figure 1).

Figure 1. Clinical Appearance of the breast
Mammography reveals two voluminous masses distorting the mammary contours and occupying almost all the right internal quadrants. The larger mass is located on the upper inner quadrant of the right breast, while the second is located in the lower inner quadrant of the right breast, they are high in tone, well-defined, with regular contours (figure 2).
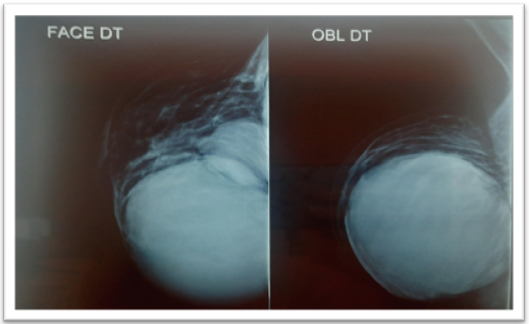
Figure 2. Mammographic Appearance
On mammary ultrasound: two well-limited, rounded masses with discreetly irregular contours, hypoechoic and heterogeneous, the larger one with a few central cystic cubicles measuring 88 x84 x81 mm in the upper inner quadrant of the right breast and the other lesion in the right lower inner quadrant measuring 39 x37 x35 mm (figure 3). The two lesions were classified as BIRADs 4.

Figure 3. Ultrasonographic Appearance of The Mass.
A tru-cut biopsy revealed a fibroepithelial tumor possibly related to a high-grade phyllodes tumor. An extension work-up revealed secondary lesions in the liver (nodule in the segment VI measuring 9 x 8 mm) and thorax (left scissural nodule, right sub pleural nodule), probable bronchopneumonia and a probable secondary bone location (osteolytic lesion of the right femoral shaft).
The patient had a right mastectomy and sentinel lymph node. Biopsy and postoperative specimens were fixed with formalin, embedded in paraffin, sliced and stained with haematoxylin and eosin. Immunohistochemistry was performed using the dex-tran-polymer method (EnVision+ ; Dako, Glostrup, Denmark) using the following mouse monoclonal anti-human antibodies against Ki-67 , differentiation group (CD)34 , desmin , leukocyte common antigen (LCA), smooth muscle actin (SMA), estrogen receptor, S-100 , CD68 and cytokeratin revealed a high-grade malignant phyllodes tumor with multifocal necrosis The primary tumor measured 19 × 17 × 8 cm, with no involvement of the skin or tissue under the nipple and superficial fascia, and a high mitosis rate with evidence of lymphovascular invasion. Final immunohistochemistry results showed a Ki-67 index of 50% +; negative reactivity for cytokeratin, AE1/AE3, CD34, desmin, LCA, SMA and ER(-); and diffuse positive reactivity for S-100 and CD68. Sentinel lymph nodes was positive with 3N+/3N.
Discussion
Phyllodes sarcomas are rather rare entities, representing only 1% of all breast tumors. In terms of etiology, Li-Fraumeni syndrome (TP53 germline mutation) has been reported to increase the risk of phyllodes tumors. These tumors often occur as a rapidly growing breast mass, considered giant if it exceeds 10cm in size [1]. Giant phyllodes sarcoma can lead to hypoglycemia, resulting from increased levels of insulin-like growth factor 2 produced by the tumor, and a high rate of metastasis in 6.2-25% of cases, most commonly to the lungs, bones and liver [4].
Mammography and breast ultrasound cannot differentiate phyllodes from other benign breast conditions such as fibroadenomas [5]. Fine-needle aspiration cytology or even tru-cut biopsy can establish the diagnosis, which will be confirmed after anathomopathological studies of the surgical specimen.
Surgery is the treatment of choice for phyllodes sarcoma. For years, the choice between breast-conserving surgery and mastectomy has remained controversial. Wide resection with clear margins of ≥1 cm has been recommended [6]. However, the study by Belkacémi et al found that total mastectomy was superior to conservative treatment in malignant phyllodes tumors in order to ensure adequate safety margins [7]. Mituś et al argued that a tumor-free margin of ≥ 1 cm is essential for favorable local control after conservative or radical surgery.
Sarcoma has a rare propensity for axillary lymph node metastasis, described in <10% of cases; consequently, lymph node dissection is not routinely performed [8].
Positive surgical margins, tumor size, high number of mitoses, stromal proliferation and necrosis are factors in poor prognosis and local recurrence. For patients with phyllodes sarcoma measuring > 2 cm after lumpectomy, or tumors > 10 cm after mastectomy, adjuvant radiotherapy is strongly recommended to control the high local relapse rate of ≥ 15% despite healthy margins and reduce local recurrence, which is considered a strong indicator of distant metastases and associated with a significantly increased risk of mortality [9]. Radiotherapy is also an effective treatment for symptomatic phyllodes sarcoma metastases, especially bone metastases [10]. The role of adjuvant chemotherapy remains controversial; cisplatin and etoposide, and ifosfamide alone or in combination with doxorubicin are recommended for large tumors (> 5 cm) or recurrent tumors [11].
Our patient had several factors for a high probability of local recurrence and poor prognosis, including tumor size > 10 cm, high mitosis rate, poorly organized stroma with variable arrangement, marked pleomorphism, focal tumor necrosis. She received postoperative radiotherapy and adjuvant chemotherapy and is currently under strict surveillance.
Conclusion
One of the challenges facing the treating physician in phyllodes sarcoma is finding patients who will develop local recurrence or metastases. Surgical management is the mainstay of treatment, and local recurrence of phyllodes tumors has been associated with several risk factors, the most important of which is postoperative margins.
References
- Yohe S, Yeh IT. "Missed" diagnosis of Phyllodes tumor on breast biopsy: pathological clues to its recognition. Int J Surg Pathol. 2008;16(2):137-42. [PubMed.]
- Lannin DR, Geibel J. Cystosarcoma Phyllode’s. 2014. [Ref.]
- Kumar T, Patel MD, Bhargavan R, Kumar P, Patel MH, Kothari K, et al. Largest Phyllodes Tumor - Case Report and Brief Review Article. Indian J Surg Oncol. 2011;2(2):141-4. [PubMed.]
- Rowe JJ, Prayson RA. Metastatic malignant phyllodes tumor involving the cerebellum. J Clin Neurosci. 2015;22:226-7. [PubMed.]
- Kim JG, Kim SY, Jung HY, Lee DY, Lee JE. Extremely rare borderline phyllodes tumor in the male breast: a case report. Clin Imaging. 2015;39(6):1108-11. [PubMed.]
- Barth RJ. Histologic features predict local recurrence after breast conserving therapy of phyllodes tumors. Breast Cancer Res Treat. 1999;57:291-5. [PubMed.]
- Belkacémi Y, Bousquet G, Marsiglia H, Ray-Coquard I, Magné N, Malard Y, et al. Phyllodes tumor of the breast. Int J Radiat Oncol Biol Phys. 2008;70:492-500. [PubMed.]
- Khosravi-Shahi P. Management of non-metastatic phyllodes tumors of the breast: Review of the literature. Surg Oncol. 2011;20 [PubMed.]
- Pezner RD, Schultheiss TE, Paz IB. Malignant phyllodes tumor of the breast: Local control rates with surgery alone. Int J Radiat Oncol Biol Phys. 2008;71:710-3. [PubMed.]
- Kapiris I, Nasir N, A'Hern R, Healy V, Gui GP. Outcome and predictive factors of local recurrence and distant metastases following primary surgical treatment of high-grade malignant phyllodes tumors of the breast. Eur J Surg Oncol. 2001;27:723-30. [PubMed.]
- Pacioles T, Seth R, Orellana C, John I, Panuganty V, Dhaliwal R. Malignant phyllodes tumor of the breast presenting with hypoglycemia: A case report and literature review. Cancer Manag Res. 2014;6:467-73. [PubMed.]