>Corresponding Author : S Haddadi
>Article Type : Case Report
>Volume : 4 | Issue : 11
>Received Date : 13 Nov, 2024
>Accepted Date : 25 Nov, 2024
>Published Date : 29 Nov, 2024
>DOI : https://doi.org/10.54289/JCRMH2400154
>Citation : Haddadi S, El Mammeri M, Amamra H, Kouachi W, Moudir M, et al. (2024) Caecal Tumour Perforation. A Case Series and Litterature Review. J Case Rep Med Hist 4(11): doi https://doi.org/10.54289/JCRMH2400154
>Copyright : © 2024 Haddadi S, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Case Report | Open Access | Full Text
1Department of General Surgery, Central Hospital of the Army. Dr Mohamed Seghir Nekkache. BP 244 Kouba Alger. Algeria
2Algiers Faculty of Medicine. Algiers University 1 Benyoucef Benkhedda
3Regional University Military Hospital of Béchar. Algeria
4Faculty of Medicine, Béchar University Tahri Mohammed. Algeria
5Mother and Child Hospital. Béni-Messous. Algiers. Algeria
6Regional University Military Hospital of Constantine. Algeria
7Constantine Faculty of Medicine. Constatine University 3 Salah Boubnider. Algeria
*Corresponding author: Said Haddadi, Department of General Surgery, Central Hospital of the Army. Dr Mohamed Seghir Nekkache. BP 244 Kouba Alger. Algeria and Algiers Faculty of Medicine. Algiers University 1 Benyoucef Benkhedda
Abstract
Although colonic tumour perforation is rare (2.6-9% of all colon cancers), it is associated with a high morbidity and mortality rate of around 30-40% and 10-12% respectively. This complication is unique to mucinous carcinomas, which are characterised by local aggressiveness and frequent recurrence after surgical resection.
In this paper, we present two observations of perforated colonic tumours operated on in two different circumstances, and which had two equally different outcomes.
This entity poses two major therapeutic problems for the surgeon. One is neoplastic (the tumour), the other septic (peritonitis). The spread of this infection to the anterior abdominal wall, or to the lower limb in some cases, further complicates therapeutic management.
Only complete carcinological treatment of the tumour and its spread can guarantee an acceptable prognosis.
Keywords: Colonic tumour perforation- Peritonitis- Recurrences- Prognosis
Abbreviations: MSI: Micro Satellite Instability, MSS: Micro Satellite Stability
Introduction
Right-sided colonic tumour perforation is a rare and misleading complication of colon cancer. In addition to its diagnostic problem, this entity presents two major therapeutic problems for the surgeon. Firstly, treatment of the peritonitis, and secondly, treatment of the cancer. This complicated condition requires tumour resection, in addition to treatment of the peritoneal spread of the infection, with restoration of digestive continuity in a previously septic site. In this article, we report two cases of colonic perforation.
The first case was a perforated caecal cancer resected as an emergency procedure, and the2nd case was a right colonic peri-neoplastic perforation operated in elective surgery. The immediate post-operative period were straightforward. However, several locoregional recurrences (colonic, parietal) occurred after the operation and were resected each time. It was only at this cost that one of the patients was able to have an acceptable survival of over ten years.
Clinical case
Patient N.Y aged 69 years, hypertensive on treatment (LOXEN*), who consulted in an emergency for an acute febrile pain syndrome of the flank and right iliac fossa.
On examination, the patient was febrile at 38.5°C and normotensive at 120/80 mmHg. In the abdomen, there was painful impaction of the right iliac fossa (FID) and tenderness of the right flank. Rectal examination was unremarkable.
Biologically, there was a hyperleukocytosis of 13600/mm3, with a hypochromic microcytic anaemia of 08.7 g/dl. There was also a positive CRP of over 96 mg/l. Radiological examination of the abdomen without preparation showed no abnormalities.
In view of these findings, the decision was made to undergo emergency surgery. Intraoperative exploration revealed a congestive appendix. There was a malignant tumour covering the entire cecum, perforated posteriorly with a right retro-colic abscess (peri-neoplastic abscess). Several lymph nodes were noted. The rest of the colon appeared healthy. There were no liver metastases or nodules of peritoneal carcinosis. A right hemi-colectomy with ileo-colic anastomosis and peritoneal lavage was performed, and a cholecystectomy for lithiasis of the gallbladder was also carried out. The immediate post-operative course was straightforward.
Histological examination of the operative specimen, 05 cm from one end, revealed a malignant epithelial tumour proliferation, ulcerating and infiltrating down to the muscularis, with a glandular appearance and rich in atypia. The fibrous tumour stroma is remodelled with necrotic and haemorrhagic foci consistent with a well-differentiated adenocarcinoma. The resection limits are satisfactory. The appendix contains lesions of acute appendicitis. No lymph node infiltration. In conclusion, well-differentiated adenocarcinoma. After a negative extension work-up, this neoplasia was classified as pT4aN0M0 (UICC Stage IIB) and the patient received 06 courses of adjuvant chemotherapy.
Three years later, a colonoscopy performed as part of the investigation of recurrent sub-occlusive syndromes revealed an anastomotic tumour formation in favour of a tubulo-papillary and mucosal colloid carcinoma after examination of samples of a core biopsy. The extension work-up was negative, and a2nd colectomy was performed, passing very widely over the colonic tumour recurrence and ensuring carcinological resection with ileocolic anastomosis. The patient had an acceptable survival of more than 10 years, after resection of two other recurrences, one ileal and the other in the abdominal wall.
Clinical case
Patient O.Z aged 72, with no particular history, who has been presenting with right iliac fossa pain with vomiting for 06 months, prompting the patient to seek medical attention. Patient classified as ASA I, WHO 0, underweight with a BMI of 18 kg/m2. Examination revealed a 10 cm mass extending from the right iliac fossa to the right flank, which was hard and deeply fixed. Colonoscopy revealed an ulcerative process in the right colon, with biopsies revealing a low cohesive cell carcinoma.
Biological findings included normocytosis of 9000/mm3 and anaemia of 9.5 g/dl.
A thoracic-abdomen-pelvic CT scan revealed a process occupying the entire cecum and extending upwards to the ascending colon, with significant densification of the peri-lesional mesenteric fat and multiple satellite adenopathies.
An MRI scan showed an abscess of the right iliac psoas measuring 83 x 84 cm and extending over a height of 105 mm (Figure 1).
The patient's case was presented at our multidisciplinary consultation meeting, where primary surgery was decided.
The patient underwent right hemicolectomy by laparotomy for a locally advanced tumour perforated posteriorly at the level of the right psoas muscle, with immediate restoration of continuity, abundant peritoneal cleansing and lamellar drainage. The post-operative course was straightforward. The histological study classified the adenocarcinoma with poorly cohesive cells as pT3N0M0(UICC Stage II) and the patient did not receive any adjuvant treatment despite our insistence on the perforated nature of the mass and the risk of peritoneal spread. Two years later, the patient presented with a recurrence in the form of a huge right psoas mass containing fine calcifications (Figure 2). It was only then that the oncologists decided to start her on chemotherapy. The patient died a few months later.

Figure 1. MRI showing a psoas abscess (red arrow) complicating a perforated right colon tumour
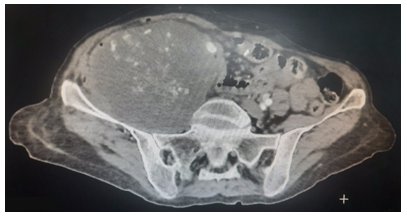
Figure 2. Tumour recurrence in the right psoas two years after surgery
Discussion
Colonic tumour perforation, although rare (2.6-9% of all colonic cancers), is associated with a high morbidity and mortality of the order of 30-40% and 10-12% respectively [1,2]. Two-thirds of patients with this complication have symptoms suggestive of common colonic disease, which delays therapeutic management. In addition, pneumoperitoneum is present in only one in five patients. This severe complication is generally associated with mucinous carcinomas, which are characterised by slow growth and local aggressiveness. This histological type was not found in our observation during the perforative episode, but at a distance at the time of recurrence. The2nd observation involved a carcinoma with poorly cohesive cells, known to be aggressive both locally and at a distance. In contrast to diastatic perforations due to downstream occlusive cancer, perforation occurs directly opposite the most advanced part of the tumour at depth, as a result of tumour necrosis of the colonic wall [3]. In some unfortunate cases, perforation may be associated with tumour occlusion and necrotising colitis due to intestinal ischaemia. This colonic ischaemia must be recognised by radiologists pre-operatively on CT scan, to better guide the extent of surgical removal [4]. The tumour may be opened posteriorly as in our two observations, or present as a buttock abscess [5]. Once the psoas has been infiltrated, the tumour may spread to the lower limb via the funnel or trigonum femorali represented by Scarpa's triangle, which worsens the prognosis and further complicates treatment [6]. The right colonic tumour may also open anteriorly towards the anterior abdominal wall, causing skin fasciitis requiring extensive parietal resection [7]. Rarely, perforation occurs in the free peritoneum, due to the slow progression of the tumour, which gives the omentum time to gradually fill in the colonic parietal microcracks as they appear.
Peritoneal cleansing must be abundant in this case. The use of an antiseptic solution based on povidone-iodine is recommended [8]. In animal experiments, this has been shown to have anti-mitotic properties. In the adjuvant treatment of stage IIB colon cancer, the addition of adjuvant chemotherapy depends on MSI (Micro Satellite Instability) or MSS (Micro Satellite Stability) status, i.e. whether or not DNA mismatches are micro-satellite instable. This status can be determined either by molecular biology or immunohistochemistry. In the case of MSI status, neoadjuvant chemotherapy is not recommended (grade B) or even contraindicated [9]. In the case of MSS status, there are no references. In this case, adjuvant chemotherapy is proposed on a case-by-case basis, in the absence of co-morbidity and in the presence of poor prognostic factors (T4, fewer than 12 lymph nodes examined, poorly differentiated tumour, vascular emboli, perforation) [10]. In our first patient, adjuvant chemotherapy was started without taking into account the DNA micro-satellite status, as this was not available in our hospital. Finally, this chemotherapy was instituted in view of the advanced and perforated nature of the tumour. However, in the2nd observation, chemotherapy was not instituted as adjuvant treatment until the recurrence appeared 2 years later. Before operating on the2nd patient, an opinion was sought from Professor Yves Panis (world expert in colorectal surgery), who recommended that the patient be given neoadjuvant radio-chemotherapy before surgery to increase the chances of an R0 excision.
These two observations show very different courses of the same neoplastic pathology. The fact that the first patient underwent emergency surgery in a septic state did not compromise her chances of recovery. In addition, the early adjuvant chemotherapy she received did not prevent recurrences. These recurrences, having been treated surgically, enabled him to have a very acceptable survival. In the case of the2nd patient, the delay in starting chemotherapy until the onset of recurrence meant a loss of opportunity for her and a shortening of her survival.
Conclusion
Perforated cancer of the cecum is a rare and misleading pathology due to its semiological variants. At the slightest suspicion of this possibility, an abdominal CT scan should be performed to determine both the local extent of the tumour and the degree of peritoneal and/or parietal spread of the infection, which will help guide the therapeutic strategy. Perforation is not the final stage of the disease, as the prognosis depends more on the presence of co-morbidities, the extent of sepsis and the presence of distant metastases. This pathological entity is characterised by the frequency of both endo and exo-luminal recurrences, as described in our two observations. Surgical treatment of peritonitis and cancer must be accompanied by adjuvant chemotherapy, and sometimes even neo-adjuvant radio-chemotherapy, to increase the chances of carcinological resection (R0), the only guarantee of an acceptable prognosis.
Bibliography
- Anwar MA., D'Souza F., Coulter R., Memon B., Khan IM., et al. Outcome of acutely perforated colorectal cancers: experience of a single district general hospital. Surg Oncol. 2006;15:91-6. [PubMed.]
- Jover naval JM., et al. Perforaciones por tumores de colon: 24 casos. Cir Esp. 1985;39:638-644. [Ref.]
- Rahili A. Péritonites d’origine colique. Fascicule de l’Association Française de Chirurgie. [Ref.]
- Satyam S., Jain K., Pradhan G. Necrotizing Colitis with Perforation Proximal to Obstructive Ascending Colon Cancer: A Case Report. Euroasian J Hepato-Gastroenterol. 2022;12(2):95-97. [PubMed.]
- Mohandas SK., Mazarello F., Bisset R. Right Gluteal Abscess: An Unusual Presentation of Perforated Caecal Adenocarcinoma. J Gastrointest Canc. 2010;41:285-287. [PubMed.]
- Timberl SJ., Straiton D., Breaks E., Sillah K., Khan N. Necrotising soft tissue infection of the lower limb due to a perforated caecal carcinoma: a case report. Journal of Medical Case Reports. 2014;8:80. [PubMed.]
- Marron CD., Mc Ardle GT., Rao M., Sinclair S., Moorehead J. Perforated carcinoma of the caecum presenting as necrotising fasciitis of the abdominal wall, the key to early diagnosis and management BMC Surgery 2006;6:11. [PubMed] [Ref.]
- Favoulet P., Benoit L., Guiu B., Rat P., Chauffert B., et al. Evaluation des lavages par la polyvidone iodée dans la prévention de l’ensemencement néoplasique péritonéal: étude expérimentale chez le rat. Annales de Chirurgie. 2002;127(8):600-605. [Ref] [Ref.]
- Bibeau F. Instabilité micro-satellitaire dans le cancer colorectal. Oncologie. 2012;14:525-529. [Ref.]
- Thésaurus National de Cancérologie Digestive de la Fédération Française de Cancérolgie Digestive (FFCD). 2013. [Ref.]