>Corresponding Author : Ziad Imane
>Article Type : Case Report
>Volume : 4 | Issue : 10
>Received Date : 16 June, 2024
>Accepted Date : 25 June, 2024
>Published Date : 29 June, 2024
>DOI : https://doi.org/10.54289/JCRMH2400150
>Citation : Fadwa A, Imane Z, Hajar E, Boufettal H, Mahdaoui S, et al. (2024) Primary Ovarian Leiomyoma in a Post-Menopausal Woman: A Rare Ovarian Tumor. J Case Rep Med Hist 4(10): doi https://doi.org/10.54289/JCRMH2400150
>Copyright : © 2024 Fadwa A, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Case Report | Open Access | Full Text
1Resident Physician, Department of Gynecology and Obstetrics, at Ibn Rochd University Hospital, Casablanca, Morocco
2Professor in the Department of Gynecology and Obstetrics at the Ibn Rochd University Hospital in Casablanca, Morocco
*Corresponding author: Ziad Imane, Resident Physician, Department of Gynecology and Obstetrics, at Ibn Rochd University Hospital, Casablanca, Morocco
Abstract
Primary ovarian leiomyoma is a rare benign tumor of the ovary seen in women between 20 and 65 years old. Clinical, ultrasonographic and tumor marker data remain the best preoperative approach currently available for ovarian tumors. Only pathological examination can establish the diagnosis. The major difficulty is to differentiate between ovarian fibroma and other solid ovarian tumors. We report the case of an ovarian fibroma in a postmenopausal patient managed for an adnexal mass in a context of chronic pelvic pain and abdominal distention.
Keywords: Primary Ovarian Leiomyoma; Leiomyoma; Myoma; Ovarian Tumor
Abbreviations: MRI: Magnetic Resonance Imaging, CEA: Carcinoembryonic Antigen
Introduction
Uterine myoma or leiomyoma is a benign tumour of the smooth muscle tissue of the uterus. Ectopic localisations are rare. Ovarian fibroids are rare. They account for 1% of organic ovarian neoplasms [1] and are usually benign. These lesions often occur in older postmenopausal patients. Clinical, ultrasound and tumour marker data remain the best preoperative approach currently available for ovarian tumours. Only pathological examination can establish the diagnosis [2].
We report a case of ovarian fibroma in a postmenopausal patient who was treated for an adnexal mass in the context of chronic pelvic pain and metrorrhagia.
Case Report
We report the case of a 70-year-old patient, with no particular history, who consulted us for abdominal distension and chronic pelvic pain that had been evolving for 8 months, with no associated urinary or digestive signs, all evolving in a context of conservation of general condition.
On clinical examination, the patient was hemodynamically and respiratory stable, with normo-colored conjunctiva, BMI 30 kg/m2, and in good general condition.
Examination under speculum revealed a normal cervix, no vaginal lesions and no bleeding. The size of the uterus was difficult to assess by vaginal touch and abdominal palpation, given the abdominal distension.
Abdominal examination revealed a distended abdomen, with palpation of a painless, hard abdomino-pelvic mass extending beyond the umbilicus.
The rest of the somatic examination was unremarkable.
An ultrasound scan revealed a right latero-uterine mass with ill-defined contours, probably ovarian, 55 mm long, associated with a peritoneal effusion (Figure 1).

Figure 1. Ultrasound appearance of the mass
An MRI scan revealed a poorly defined abdomino-pelvic lesion measuring 120 x 112 x 133.5 mm with a heterogeneous, moderately enhanced signal after injection of the contrast medium. The lesion came into intimate contact with the digestive tract laterally and the uterus inferiorly, compressing the bladder. Infiltration of the surrounding fat. Moderate peritoneal effusion. No individualization of the left ovary (Figure 2).
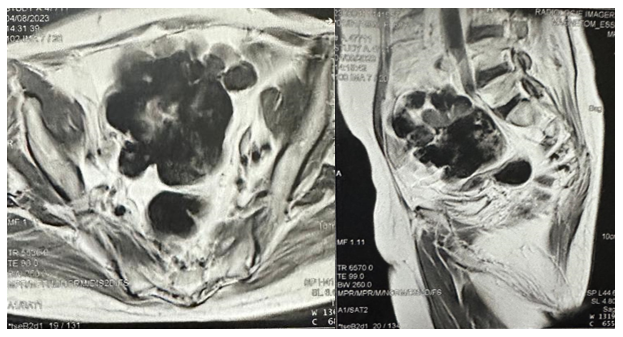
Figure 2. MRI appearance of the mass
The CA125 assay was 10.71 U/ml, ACE 3 ug/l and CA 19-9 8 UI/L.
The patient underwent surgical exploration by median laparotomy under the umbilicus, which revealed a uterus of normal size, a moderate amount of effusion, the presence of a 15 cm multiloculated right latero-uterine mass, the left adnexa was normal, and there was no sign of carcinosis. A sample of the ascites was taken for pathological examination. First, a right adnexectomy was performed for extemporaneous examination, which revealed no signs of malignancy and was in favor of an ovarian fibroid. Total hysterectomy without adnexal preservation was then performed (Figure 3).

Figure 3. A: right adnexectomy. B: Total hysterectomy without adnexal preservation
Pathological examination confirmed the presence on the adnexectomy specimen of a solid multilobed tumor with a smooth outer surface measuring 12 cm in diameter and corresponding to an ovarian fibroid.
Post-operative management was straightforward.
Discussion
Uterine myoma or leiomyoma is a benign tumor of the smooth muscle tissue of the uterus [3]. Its extrauterine localization is rare, its physiopathogenesis is poorly understood and it poses a diagnostic problem [4].
Primary ovarian leiomyoma is a rare benign tumor accounting for 0.5-1% of all benign ovarian tumors [5], first described in 1862 by Fallahzadeh et al [6].
It usually occurs between the ages of 20 and 65 years and is usually discovered incidentally. Approximately 85% of cases are detected in perimenopausal and postmenopausal women together. Of these, 16% are found after the menopause [7-10]. The age group for both ovarian and uterine leiomyomas is similar, with a very wide range, but only a few cases have been reported in postmenopausal women as in our case [11]. A review of the literature shows that less than 100 cases of primary ovarian leiomyomas have been reported up to 2020 [11].
They represent an anatomopathological variant of fibrothecal tumors of the ovary, which are stromal tumors associated with spindle-shaped connective cells, thecal cells or both [12].
The exact cause of ovarian leiomyomas is unknown, but it is thought that they arise from smooth muscle and include ovarian hilar blood vessels, ovarian ligament, smooth muscle cells or multipotential cells in the ovarian stroma, undifferentiated germ cells, cortical smooth muscle metaplasia, smooth muscle metaplasia of the endometrial stroma, smooth muscle in mature cystic teratomas, smooth muscle in the walls of mucinous cystic tumors, and metastatic uterine leiomyoma to the ovary [13,14].
Most are usually small (<3 cm) and asymptomatic, and are therefore discovered either incidentally during routine physical examination, incidentally during surgery, or at autopsy after histopathological examination. If the tumor is large, it may cause pelvic pain, a palpable mass, or sometimes present as an acute abdomen due to torsion or necrosis in the tumor. In the present case, the woman presented with abdominal distension and pelvic pain [15].
They may be bilateral in 4-8% of patients and multiple in 10% of cases [16], particularly in Gorlin's syndrome [17], or associated with pleural effusion and ascites in Meigs' syndrome [18]. Bilateral ovarian leiomyomas are seen in pediatric and young women and are usually not associated with uterine leiomyomas as seen in perimenopausal women [19].
There are no pathognomonic symptoms or characteristic imaging findings and therefore it is a diagnostic challenge for clinicians and is mostly misdiagnosed. It should therefore be considered in the differential diagnosis of solid ovarian masses.
The main difficulty is to differentiate ovarian fibroma from other solid ovarian tumors [20]. Cystic degeneration and hemorrhage are common, but calcification in ovarian fibroma is rare.
Radiological examination is often insufficient to make an accurate diagnosis. The sonographic appearance is that of an echogenic mass associated with multiple shadow cones not related to calcifications but to the attenuation of the ultrasound beam by the fibrous tissue [21]. Ultrasound is inconclusive and magnetic resonance imaging (MRI) may be suggested. Ovarian fibromas are described as typically showing low signal intensity on T1-weighted MR images and marked hypointensity on T2-weighted images; contrast enhancement of fibromas is heterogeneous and mild-to-moderate [22].
Serum levels of CA-125, CA 19-9 and carcinoembryonic antigen (CEA) are within the normal range, as in our case. Ovarian leiomyomas occurring synchronously with uterine leiomyomas in 78% of cases suggest identical hormonal stimulation [23,24].
The correct diagnosis of an ovarian fibroid requires identification of the smooth muscle nature of the tumor.
Ovarian leiomyomas must also be differentiated from leiomyosarcomas. Pathologists use criteria such as the number of mitoses, cytological atypia and tumor necrosis. None of these criteria were found in our case [19].
Surgical treatment is recommended. Salpingo-oophorectomy can be considered in perimenopausal or postmenopausal women, and cystectomy can be performed only in young women [25].
Conclusion
Ovarian fibroids are rare, preoperative diagnosis is very difficult, surgery with histological study is used to establish the diagnosis. An updated literature review should describe the incidence of these tumors in order to remove the controversy about their existence, as they are increasingly reported in the literature.
References
- Chechia A, Attia L, Temime RB, Makhlouf T, Koubaa A. Incidence, clinical analysis, and management of ovarian fibromas and fibrothecomas. Am J Obstet Gynecol. 2008;199(5):473.e1-4. [PubMed.]
- Abdeddine F, Meddah J, El Youssfi M, Amrani S, Bargach S. Atypical locations of fibromyomas (ovarian and large ligament): About two cases. Int J Innov Appl Stud. 2020;30(1):336‑9. [Ref.]
- Christin-Maitre S, Wirthner D. Uterine fibromas: classification and physiopathology. J Gynecol Obstet Biol Reprod (Paris). 1999;28(7):707‑14. [PubMed.]
- Kinda B, Ouédraogo C, Ouagré E, Ghilat N, Simporé A, Bonkougou P, et al. Localisation atypique de myomes en peropératoire: à propos de deux cas dont un dans un contexte d’urgence. Pan Afr Med J. 2015;22:79. [Ref.]
- Agrawal R, Kumar M, Agrawal L, Agrawal KK. A Huge Primary Ovarian Leiomyoma with Degenerative Changes-An Unusual. J Clin Diagn Res JCDR. 2013;7(6):1152‑4. [PubMed.]
- Fallahzadeh H, Dockerty MB, Lee RA. Leiomyoma of the ovary: report of five cases and review of the literature. Am J Obstet Gynecol. 1972;113(3):394‑8. [PubMed.]
- Hsiao CH, Wang HC, Chang SL. Ovarian leiomyoma in a pregnant woman. Taiwan J Obstet Gynecol. 2007;46(3):311‑3. [Ref.]
- Asada T, Yamada T, Kumano R. Primary ovarian leiomyoma with predominant cystic change. Radiol Case Rep. 2019;14(11):1315‑9. [Ref.]
- Safaei A, Khanlari M, Azarpira N, Monabati A. Large ovarian leiomyoma in a postmenopausal woman. Indian J Pathol Microbiol. 2011;54(2):413‑4. [Ref.]
- Wei C, Lilic N, Shorter N, Garrow E. Primary ovarian leiomyoma: a rare cause of ovarian tumor in adolescence. J Pediatr Adolesc Gynecol. 2008;21(1):33‑6. [PubMed.]
- Meel M, Hemrajani D, Kumar M, Agnani B. Symptomatic Primary Ovarian Leiomyoma in a Postmenopausal Woman: A Rare Entity. J -Life Health. 2020;11(3):175‑7. [PubMed.]
- Bouab M, Touimi AB, El Omri H, Boufettal H, Mahdaoui S, Samouh N. Primary ovarian fibroma in a postmenopausal woman: A case report. Int J Surg Case Rep. 2022;92:106842. [PubMed.]
- Sushma Bharti, Sudeep Khera, Charu Sharma, and Arsha Balakrishnan. Unilateral primary ovarian leiomyoma masqueraded as ovarian fibroma: A histopathological diagnosis. 2021; 10(9): 3494-3497. [PubMed.]
- Kataria SP, Chawla N, Singh G, Kum S. Ovarian leiomyoma associated with serous cystadenoma–A case report of an uncommon entity. Glob J Pathol Microbiol. 2014;14(4):38‑42. [Ref.]
- Kurai M, Shiozawa T, Noguchi H, Konishi I. Leiomyoma of the ovary presenting with Meigs’ syndrome. J Obstet Gynaecol Res. 2005;31(3):257‑62. [PubMed.]
- Boujoual M, Hakimi I, Kouach J, Oukabli M, Moussaoui DR, Dehayni M. Large twisted ovarian fibroma in menopausal women: a case report. Pan Afr Med J. 2015;20:322. [Ref.]
- Aram S, Moghaddam NA. Bilateral ovarian fibroma associated with Gorlin syndrome. J Res Med Sci Off J Isfahan Univ Med Sci. 2009;14(1):57‑61. [Ref.]
- Biren Parikh, Pragna Sharma, Swati Parikh, Hrushikesh Surti. Ovarian Fibroma Presented As Meigs Syndrome: A Case Report. GCSMC J Med Sci. 2015;4(2). [Ref.]
- Taskin MI, Ozturk E, Yildirim F, Ozdemir N, Inceboz U. Primary ovarian leiomyoma: A case report. Int J Surg Case Rep. 2014;5(10):665‑8. [PubMed.]
- Cherrabi F Zahra, Jaouad Kouach DRM. Fibrome ovarien géant: A propos d’un cas. J Maroc Sci Médicales. 2017;21(4). [Ref.]
- Leung SW, Yuen PM. Ovarian fibroma: a review on the clinical characteristics, diagnostic difficulties, and management options of 23 cases. Gynecol Obstet Invest. 2006;62(1):1‑6. [PubMed.]
- Roue A, Laboisse C, Winer N, Darnis E, Bouquin R, Lopes P, et al. [Extra-uterine pelvic leiomyoma: diagnosis and practical management]. J Gynecol Obstet Biol Reprod (Paris). 2007;36(4):403‑8. [PubMed.]
- Lim S chul, Jeon H jong. Bilateral primary ovarian leiomyoma in a young woman: case report and literature review. Gynecol Oncol. 2004;95(3):733‑5. [PubMed.]
- Pandit MJ, Watson NR, Mackenzie IZ. Leiomyoma of the ovary. J Obstet Gynaecol J Inst Obstet Gynaecol. 1997;17(5):503‑4. [PubMed.]
- Son CE, Choi JS, Lee JH, Jeon SW, Hong JH, Bae JW. Laparoscopic Surgical Management and Clinical Characteristics of Ovarian Fibromas. JSLS. 2011;15(1):16‑20. [Ref.]