>Corresponding Author : Sabir Soukaina
>Article Type : Case Report
>Volume : 4 | Issue : 8
>Received Date : 05 June, 2024
>Accepted Date : 21 June, 2024
>Published Date : 24 June, 2024
>DOI : https://doi.org/10.54289/JCRMH2400143
>Citation : Soukaina S, Hajar E, Fadwa A, Leila E, Oumnia E, et al. (2024) Nodular Pseudoangiomatous Stromal Hyperplasia in A 22-Year-Old Woman: A Case Report. J Case Rep Med Hist 4(9): doi https://doi.org/10.54289/JCRMH2400143
>Copyright : © 2024 Soukaina S, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Case Report | Open Access | Full Text
1Resident Physician, Department of Gynecology and Obstetrics, at Ibn Rochd University Hospital, Casablanca, Morocco
2Professor in the Department of Gynecology and Obstetrics at the Ibn Rochd University Hospital in Casablanca, Morocco
*Corresponding author: Sabir Soukaina, Resident Physician, Department of Gynecology and Obstetrics, Ibno Rochd University Hospital, Casablanca, Morocco
Abstract
Pseudoangiomatous breast stromal hyperplasia (PASH) is a rare benign mastopathy, characterized by its particular histological aspect with the presence of pseudovascular clefts in a collagenous stroma. Immunohistochemical analysis is the cornerstone of the diagnosis. The PASH mainly affects premenopausal women and often goes unnoticed, its discovered by chance during pathological examination. Pseudoangiomatous stromal hyperplasia can manifest itself in several clinical forms, but rarely in the nodular form of PASH. This lesion deserves to be recognized in daily practice, so as not to be confused with a low-grade angiosarcoma. The object of this article is to clarify this rare benign mastopathy and it’s different clinical, radiological, and anatomopathological aspects.
Keywords: Pseudoangiomatous stromal hyperplasia, Breast, Benign mastopathy, PASH
Abbreviations: PASH: Pseudoangiomatous Breast Stromal Hyperplasia
Introduction
Pseudoangiomatous breast stromal hyperplasia (PASH) is a rare, benign mastopathy that mainly affects premenopausal women [1]. Pseudoangiomatous hyperplasia lesions are often discovered incidentally during histological study of a breast biopsy [2]. Rarely, it presents clinically as a palpable nodule that rapidly increases in volume and frequently recurs. Anatomopathological examination reveals pseudovascular fissures in a collagen-rich fibrous stroma, enabling the diagnosis to be made [1]. The term "pseudoangiomatous" has been attributed to the similarity of it’s histological appearance, simulating vascular proliferation, notably angiosarcoma. We report a case of PASH in a 22-year-old woman, with the aim of outlining the various clinical, radiological and pathological aspects of this pathology.
Case Report
The patient was a 22-year-old woman with no previous pathological history, who presented with a rapidly enlarging mass in the left breast. Clinical examination revealed a supraareolar mass, measuring 5 cm in long axis, well limited, mobile, with no cutaneous signs or palpable adenopathies. On ultrasonography, it was a heterogeneous formation measuring 44 x 21 mm, with regular contours and a cystic component with central vascularization on doopler (Figures 1 and 2).
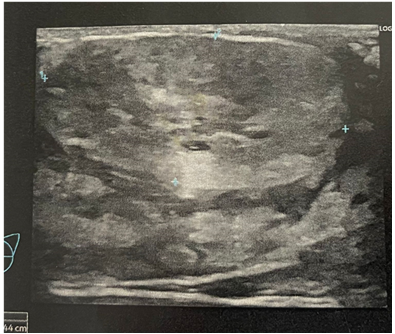
Figure 1. An ultrasonography image of an heterogeneous formation measuring 44 x 21 mm, with regular contours, with cystic component ( PASH)
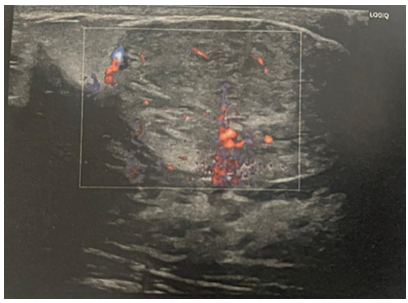
Figure 2. A doopler image of a PASH formation with central vascularization the tumor was classified as American College of Radiology (ACR) BI-RADS 4, pointing to a phyllodes tumor.
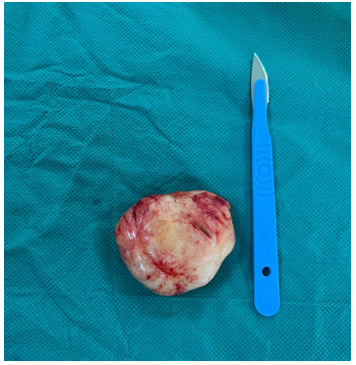
Figure 3. A lumpectomy of the tumor that was classified as American College of Radiology (ACR) BI-RADS 4, pointing to a phyllodes tumor.
A biopsy was performed, which was consistent with an adenofibroma. A lumpectomy was undertaken, and histology revealed a benign proliferation of myofibroblasts forming a network of slits lined with myofibroblasts, creating pseudovascular spaces in inter- and intra-lobular connective tissue (Figure 3). On immunohistochemical examination, the conjunctival cells lining the slits were positive for fibroblast markers: CD34 +, vimentin + and negative for endothelial cell markers for CD31 and factor VIII, thus ruling out a vascular lesion. The diagnosis of pseudoangiomatous hyperplasia of the mammary stroma was therefore accepted. Progression was favourable, with no recurrence over one year.
Discussion
PASH is a rare benign formation, first described by Vuitch, Erlandson and Rosen in 1986 [3]. They reported a series of nine cases of mammary formations characterized by a network of anastomotic clefts lined with endothelial-like cells, simulating vascular clefts. These empty spaces are arranged in a characteristic collagen-rich stroma around the lobules. Since then, around 100 cases have been reported in the literature [4].
This lesion is characterized by a large proliferation of the breast stromal collagen, creating a pseudovascular appearance bordered by myofibroblasts [4]. It mainly affects premenopausal women with an average age of 40. It can also affect older women, particularly those on hormone therapy. Pseudoangiomatous stromal hyperplasia is mostly discovered by chance, during the anatomopathological study of a breast biopsy [5].
Pseudo angiomatous stromal hyperplasia manifests itself clinically in a wide variety of ways , PASH therefore covers a very broad clinical spectrum: nodular PASH , bilateral diffuse PASH , PASH and gynecomastia , PASH and adenofibroma , bilateral diffuse PASH , PASH and fibrocystic dystrophy. As in our patient's case, it can sometimes present as a malignant picture, with a rapid increase in the size of the mass [1]. Therefore, Pseudo angiomatous stromal hyperplasia may present as a palpable, mobile, firm nodular formation, often mistaken for an adenofibroma or a phyllodes tumor. Cases of PASH have been described in male subjects revealed by gynecomastia [6].
Radiologically, PASH is non-specific on imaging, the mammography often shows a well-limited, dense, homogeneous, rounded opacity with no microcalcifications [4]. Ultrasonographically, it appears as a heterogeneous solid formation that is mainly hypoechogenic with cystic inclusions [7].
Macroscopically, pseudoangiomatous stromal hyperplasia in its nodular form presents as a well-limited, firm, smooth-surfaced, non-encapsulated mass ranging in size from 1 to 18 cm [1]. On section, the contents of the PASH are pinkish-beige, sometimes containing a few cystic cavities without necrosis or hemorrhage, simulating a fibroadenoma. In its diffuse form, the specimen does not contain a macroscopically identifiable mass, despite its perception on physical examination [8].
Histologically, PASH corresponds to a double proliferation of epithelial and conjunctival cells, formed mainly by myofibroblasts expressing both myoid and fibroblastic features [1]. On immunohistochemistry, vimentin is consistently positive, while actin is less so, and is present in proliferative PASH lesions [9]. In addition, CD34 positivity is generally constant, and the absence of expression of vascular markers (Factor VIII, CD31) by cleft cells is pathognomonic of PASH lesions, and thus helps to rule out a low-grade angiosarcoma, whose infiltrative appearance is at odds with the lobulocentric architecture of PASH [10]. The highly cellular form of the stroma may also be confused with a phyllodes tumor [10].
The term "pseudoangiomatous" was coined to characterize its distinctive histological appearance, which can be mistaken for vascular proliferation [11]. As a result, the main differential diagnosis is with low-grade angiosarcoma, formed by vascular clefts bordered by irregular endothelium and filled with erythrocytes [4]. Immunohistochemical analysis is therefore an essential tool for distinguishing PASH from angiosarcoma.
The surgical procedure for pseudoangiomatous stromal hyperplasia (PASH) is based on a simple removal of the lesion if it is unique and symptomatic, or if there is a fast increase in the size of the mass, or if there is a suspicion of malignancy [8]. However, the recurring and diffuse type of PASH is difficult to treat and may require a mastectomy [9].
On the other hand, simple surveillance may be warranted if the lesion is small, following histological confirmation of the PASH diagnosis on a biopsy sample of the lesion [12].
Pseudoangiomatous stromal hyperplasia lesions have a favorable prognosis [4].
Indeed, no distant metastases have been reported in the literature. Nevertheless, 15% to 22 % of local recurrences have been reported, which may be explained by incomplete exeresis of PASH or the persistence of inaccessible microscopic lesions. Recurrences of PASH can occur from 1 month to 1 year after the initial diagnosis, and may be combined with a recurrence of PASH in the opposite breast [12]. Therefore, a periodic mammographic follow-up is recommended [11].
Conclusion
The PASH is a rare benign pathology does not increase the risk of subsequent breast cancer. Its prognosis is excellent and the recurrence is exceptional in cases of complete resection. Histological diagnosis can only be established by microbiopsy. The immunohistochemical analysis is a crucial element for the diagnosis. Surgical treatment is recommended for tumoral forms, but is not mandatory for sub-clinical forms. The prognosis is generally excellent, with a recurrence rate of around 10%. This lesion deserves to be recognized in daily practice, so as not to be confused with low-grade angiosarcoma.
References
- Mansouri D, Mrad K, Sassi S, Driss-Fourati M, Abbes I, Koobaa-Mahjoub W, et al. L’hyperplasie pseudo-angiomateuse du stroma mammaire. Ann Pathol. 2004;24:179-82. [PubMed.]
- Vuitch MF, Rosen PP, Erlandson RA. Pseudoangiomatous hyperplasia of mammary stroma. Hum Pathol. 1986;17:185-91. [PubMed.]
- Sng KK, Tan SM, Mancer JFK, Tay KH. The contrasting presentation and management of pseudoangiomatous stromal hyperplasia of the breast. Singapore Med J. 2008;49:82-5. [PubMed.]
- Okashi K, Ogawa H, Suwa H, Saiga T, Kobayashi H. A case of nodular pseudoangiomatous stromal hyperplasia (PASH). Breast Cancer. 2006;13:349-53. [PubMed.]
- Ibrahim RE, Sciotto CG, Weidner N. Pseudoangiomatous hyperplasia of mammary stroma. Cancer. 1989;63:1154-60. [Ref.]
- Taira N, Ohsumi S, Aogi K, Maeba T, Kawamura S, Nishimura R, et al. Nodular pseudoangiomatous stromal hyperplasia of mammary stroma in a case showing rapid tumor growth. Breast Cancer. 2005;12:331-6. [PubMed.]
- Tavassoli FA. Pathology of the breast. New York: McGraw Hill; 1999. [Ref.]
- Powell CM, Cranor ML, Rosen PP. Pseudoangiomatous Stromal Hyperplasia (PASH). A mammary stromal tumor with myofibroblastic differentiation. Am J Surg Pathol. 1995;19:270-7. [PubMed.]
- Mansouri D, Mrad K, Sassi S, Driss-Fourati M, Abbes I, Koubaa-Mahjoub W, Ben Romdhane K. L’hyperplasie pseudo-angiomateuse du stroma mammaire. Ann Pathol. 2004;24(2):179-82. [Ref.]
- Kallel R, Mnif H, Gouiaa N, Khadhrawi H, Daoud E, Ayadi L, Sellami Boudawara T. Hyperplasie pseudoangiomateuse du stroma mammaire nodulaire chez une jeune femme de 19 ans. Imagerie de La Femme. 2009;19(2):117-20. [Ref.]
- Wieman SM, Landercasper J, Johnson JM, Ellis RL, Wester SM, Lambert PJ, et al. Tumoral pseudoangiomatous stromal hyperplasia of the breast. Am Surg. 2008;74:1211-4. [PubMed.]
- Lee JS, Oh HS, Min KW. Mammary pseudoangiomatous stromal hyperplasia presenting as an axillary mass. Breast. 2005;14:61-4. [Ref.]