>Corresponding Author : Ziad Imane
>Article Type : Case Report
>Volume : 4 | Issue : 7
>Received Date : 09 May, 2024
>Accepted Date : 20 May, 2024
>Published Date : 28 May, 2024
>DOI : https://doi.org/10.54289/JCRMH2400136
>Citation : Younes B, Imane Z, Doha EK, Sara T, Mustapha B, et al. (2024) Phyllodes Tumor in a Young Girl: One Case Report. J Case Rep Med Hist 4(7): doi https://doi.org/10.54289/JCRMH2400136
>Copyright : © 2024 Younes B, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Case Report | Open Access | Full Text
1Professor in the Department of Gynecology and Obstetrics at the Ibno Rochd University Hospital in Casablanca, Morocco
2Resident Physician, Department of Gynecology and Obstetrics, at Ibno Rochd University Hospital, Casablanca, Morocco
*Corresponding author: Ziad Imane, Resident Physician, Department of Gynecology and Obstetrics, at Ibno Rochd University Hospital, Casablanca, Morocco
Abstract
Phyllodes tumors (PT) of the breast represent less than 1% of all mammary tumors, particularly in adolescent girls and young women with the ability to recur and metastasize, and it behaves biologically like a stromal neoplasm. Traditionally, phyllodes tumors are graded by the use of a set of histologic data into benign, borderline, and malignant.
Keywords: Phyllodes Tumor; Breast Masses; Adolescent Girl
Abbreviations: PT: Phyllodes Tumors
Introduction
Phyllodes tumors (PT) of the breast are rare biphasic breast tumor neoplasms. They represent less than 1% of all mammary tumors and 2% to 3% of fibroepithelial neoplasms of the breast and are typified by stromal proliferation. They are more common in genitally active women than in post-menopausal women, and are frequently large (4 to 5 cm) at the time of diagnosis.
It is a mixed tumor, known as fibro-epithelial, characterized by the proliferation of epithelial cells and connective tissue cells, whereas the majority of breast cancers affect glandular cells. These tumors can be malignant or benign.
We report the clinical observation, imaging data, pathological findings and management of a phyllodes tumor in a 14-year-old girl.
Case Report
We report the observation of a 14-year-old girl, menarche at the age of 13, with no particular personal or family pathological history, who consulted for a right breast mass. The symptoms began 3 months previously with the self-examination of a firm, painless mass in the left breast, which was progressively increasing in size, prompting a consultation. The breast examination revealed a mass covering the entire upper internal quadrant of the right breast, firm, painless and mobile both within the breast tissue and related to the chest wall and skin, with no inflammatory signs or skin lesions (Figure 1). Examination of the lymph nodes revealed no palpable adenopathy. The rest of the somatic examination revealed no abnormalities elsewhere. A breast ultrasound scan revealed a large, slightly hypoechoic mass with lobulated contours in favor of a phyllodes tumor in the upper-internal quadrant (Figure 2). The patient underwent lumpectomy and pathological analysis (Figure 2) concluded that the tumor was a grade 2 phyllodes with the resection margins > 1 cm (Figure 3).

Figure 1. A mass covering the entire right upper medial quadrant.

Figure 2. Ultrasound findings in favor of a phyllodes tumor.
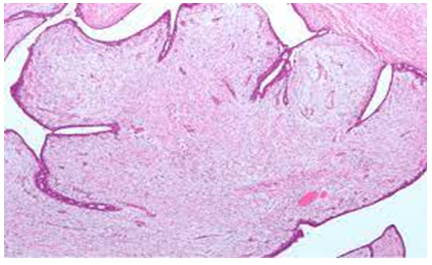
Figure 3. Histological appearance of a grade 2 phyllodes tumor.
Discussion
This case study is a presentation of a benign phyllode tumor occurring in a 14-year-old girl. Phyllodes tumors represent only 0.3 - 1% of breast tumors occurring in young women aged 20-45 rarely in adolescence [1,2].
Phyllodes tumors usually present as a rapidly growing but clinically benign breast mass [3]. In some patients, a lesion may have been presented for several years, with clinical presentation precipitated by a sudden increase in size. They are most frequently found in the upper-external quadrant, with an equal proportion occurring in either breast [4]. The skin may show stretch marks or inflammatory signs only if the tumor is large or superficial, but retraction of the nipple is rare. Attachment to the skin or pectoral muscles has been reported, but ulceration is rare, even in patients with histologically malignant tumors [4], pressure necrosis of the overlying skin may occur. A palpable axillary adenopathy may be identified, but this remains a rare occurrence [5]. our case, the tumor was located in the upper-internal quadrant with no inflammatory signs.
As with fibroadenomas, phyllodes tumors are well defined on mammography with a smooth and sometimes lobulated border. A radiolucent "halo" may be seen around the lesion, due to compression of the surrounding mammary stroma [6]. Coarse microcalcifications have been reported in fibroadenomas and phyllodes tumors, but so-called "malignant" microcalcifications are rare. There is no mammographic indicator to differentiate benign from malignant tumors. On ultrasound, phyllodes tumors often have smooth contours with homogeneous low-level internal echoes, intramural cysts, and no reliable ultrasound indicator has been identified to differentiate benign from malignant lesions [7]. The role of magnetic resonance imaging in the evaluation of phyllodes tumors and fibroadenomas remains to be defined. The main differential diagnosis for phyllodes tumors is adenofibromas.
Histologically, a phyllode tumor is a fibroepithelial tumor with stromal hyperplasia. The histopronostic grade is established on the basis of the combination of negative histological factors, in particular the number of mitoses per 10 fields, the severity of cellular atypia, the tumor/healthy parenchyma interface, the presence of tumor necrosis and stromal density. The tumor is classified according to its histopronostic grade into 3 grades; grade 1 corresponds to a benign tumor with no histological pejorative factors and no risk of recurrence, grade 2 corresponds to a borderline tumor with the presence of at least one pejorative factor and grade 3 corresponds to a phyllodes sarcoma with at least 3 pejoratives factors and a risk of metastases estimated at 25% at 3 years [8].
Surgical treatment is the standard of care. An enlarged lumpectomy with a safety margin is indicated for grade 1 and 2 tumors [8]. A simple mastectomy without lymph node dissection is indicated for grade 3 tumors, or for tumors larger than 5 cm [9]. Adjuvant radiotherapy is appropriate in the case of a grade 3 tumor, a 3rd local recurrence, or a recurrence after mastectomy. Phyllodes tumors behave relatively benignly, but local recurrence may occur in 25% of cases [10], particularly after conservative treatment.
Conclusion
Phyllodes tumors are rare and should be considered in the presence of a rapidly growing tissue nodule. Imaging is not specific. The diagnosis is made by histopathological examination. Phyllodes tumors, like adenofibromas, are fibro-epithelial tumors, i.e., tumors with double proliferation, both glandular epithelial and connective. It is the histological appearance of the conjunctival component that enables a distinction to be made between benign phyllodes tumors (differential diagnosis with adenofibromas), malignant phyllodes tumors (phyllodes sarcomas) and borderline phyllodes tumors.
Patient's consent: Written informed consent was obtained from the patient for publication and any accompanying images.
References
- Kanouni L, Jalil A, Saâdi I, Sifat H, Hadadi K, et al. (2014) Prise en charge des tumeurs phyllodes du sein à l'Institut national d'oncologie de Rabat, Maroc. Gynécologie Obstétrique & Fertilité. (32): 293-301. [Ref.]
- Adachi Y, Matsushima T, Kido A, et al. (1993) Phyllodes tumor in adolescents. Report of two cases and review of the literature. Breast Dis. 6: 285-293. [Ref.]
- Umpleby HC, Guyer PB, Moore I. (1989) An evaluation of the preoperative diagnosis and management of cystosarcoma phyllodes. Ann R Coll Surg Engl. 71: 285-288. [Ref.]
- Chua CL, Thomas A, Ng BK. (1989) Cystosarcoma phyllodes: a review of surgical options. Surgery. 105: 141-147. [PubMed.]
- Issara K, Houjami M. (2016) Tumeur phyllode chez une jeune adolescente de 12 ans: à propos d’un cas et revue de la littérature. [Ref.]
- Bader L. Isaacson C. (1961) Bilateral malignant cystosarcoma phyllodes. Br J Surg. 48: 519-521. [PubMed.]
- Blanco AJ, Serrano BV, Romero RR, et al. (1999) Phyllodes tumors of the breast. Eur Radiol. 9: 356-360. [PubMed.]
- Bartoli C, Zurrida S, Veronesi P, et al. (1990) Small sized phyllodes Tumor of the breast. Eur J Surg Oncol. 16(3): 215-219. [PubMed.]
- Sorelli Paolo G, Daniel Thomas, Ashley Moore, Mihir Khan, Happy Hoque. (2010) Malignant phyllodes tumor in an 11-year-old premenarchal girl. Journal of Pediatric Surgery. 45(2): E17-E20. [PubMed.]
- Graciela Lewitan, Carolina Goldbergb, Rubén De Sousa Serrob, Cristina Cabaleiroa, Stella Maris Espora. (2010) Tumor phyllodes en una niña de 11 años: communication de un caso. Arch Argent Pediatr. 108(2): 41-43. [PubMed.]