>Corresponding Author : Wissal Bencherifi
>Article Type : Case Report
>Volume : 4 | Issue : 7
>Received Date : 09 May, 2024
>Accepted Date : 20 May, 2024
>Published Date : 24 May, 2024
>DOI : https://doi.org/10.54289/JCRMH2400133
>Citation : Bencherifi W, Badi H, Ouladlahsen A, Ihbibane F, Sodqi M, et al. (2024) Acute Pyelonephritis with Renal Vein and Inferior Vena Cava Thrombosis: A Case Report. J Case Rep Med Hist 4(7): doi https://doi.org/10.54289/JCRMH2400133
>Copyright : © 2024 Bencherifi W, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Case Report | Open Access | Full Text
Department of infectious and tropical diseases, CHU Ibn Rochd Casablanca, Morocco
*Corresponding author: Wissal Bencherifi, Department of infectious and tropical diseases, CHU Ibn Rochd Casablanca, Morocco
Abstract
Acute pyelonephritis might be complicated by the formation of renal and perirenal abscesses and very rarely by renal vein thrombosis (RVT), which is a life-threatening condition. We report a case of 35-year-old female with no significant past medical history, who presented a week history of fever, hematuria, flank pain, and lower urinary tract symptoms. Physical examination showed a shivering young woman with fever 39°C of temperature, left flank pain and tenderness was observed on palpation. Laboratory test results showed elevated CRP level at 210 mg/L, white blood cell count at 23000/mm3 with 14000/mm3 neutrophil. Urinalysis showed pyuria, bacteriuria and nitrites presence. Urine cultures grew Escherichia coli and blood cultures were sterile. Unfortunately, after 2 days of antibiotic therapy the patient flank pain worsened, and further imaging evaluation with Abdominal CT scan showed extensive thrombosis of the left renal vein and its branches protruding to the inferior vena cava. The patient improved after intravenous antibiotics and anticoagulation treatment. At 1-month follow-up, the patient was asymptomatic. At 3 months follow-up, CECT showed complete resolution of the IVCT and attenuated renal vein with atrophic small kidney. In conclusion, renal venous thrombosis secondary to acute pyelonephritis is very rare. It is very important to treat it rapidly because it can lead to pulmonary embolism, thrombosis of the inferior vena cava or renal failure, thus jeopardizing the patient's vital and functional prognosis.
Keywords: Acute Pyelonephritis; Renal Vein Thrombosis; Inferior Vena Cava Thrombosis; Antibiotics; Anticoagulation
Abbreviations: RVT: Renal Vein Thrombosis, IVCT: Inferior Vena Cava Thrombosis, ESR: Erythrocyte Sedimentation Rate, PAI: Plasminogen Activator Inhibitor, MRI: Magnetic Resonance Imaging
Introduction
Renal vein thrombosis (RVT) and inferior vena cava thrombosis (IVCT) are uncommon and life-threatening complications of acute pyelonephritis. RVT is a common condition amongst patients with nephrotic syndrome, most commonly seen in patients with membranous glomerulonephritis. Other etiologies include membranoproliferative glomerulonephritis, minimal change disease, diabetic nephropathy, trauma, malignancy and hypercoagulable states. However, only few cases of RVT and IVCT complicating acute pyelonephritis have been described in the literature. It is difficult to distinguish between acute pyelonephritis and RVT because both present with fever, flank pain, and hematuria. We report a case of severe acute pyelonephritis due to Escherichia coli complicated with RVT and IVCT.
Case Report
A 35-year-old female with no significant past medical history, with no history of diabetes mellitus nor high blood pressure, a nonsmoker, with no family history suggestive of thromboembolic disorder. The patient was admitted with a week history of fever, hematuria, flank pain, and lower urinary tract symptoms, she also complained of recurrent shaking and chills. Physical examination at admission showed a shivering young woman with fever 39°C of temperature, blood pressure of 120/ 60 mmHg, heart rate 120 beats per minute, respiratory rate 14 breaths per minute with an oxygen saturation of 100% on room air. She weighed 71 kg with a height of 168 cm and a BMI of 25.1. The abdominal examination revealed a left flank pain and tenderness was observed on palpation. The remainder of the examination was unremarkable. Laboratory test results showed elevated CRP level at 210 mg/L, white blood cell count at 23000/mm3 with 14000/mm3 neutrophil. Her erythrocyte sedimentation rate (ESR) was 70 mm at the end of 1 h and the random blood sugar was normal. The prothrombin time, the prothrombin index, and the activated partial thromboplastin time were normal. Renal, hepatic and coagulation parameters were normal. Urinalysis showed pyuria, bacteriuria and nitrites presence. Urine cultures grew Escherichia coli (sensitive to nitrofurantoin, ciprofloxacin, cefuroxime, cotrimoxazole, ceftriaxone, norfloxacin and amoxicillin-clavulanate). Blood cultures were sterile.
Initial imaging evaluation of the left kidney and ureter with renal ultrasound showed an enlarged globular left kidney. Unfortunately, after 3 days of antibiotic therapy the patient flank pain worsened, and further imaging evaluation with abdominal computed tomography (CT scan) with intravenous iodine contrast showed extensive thrombosis of the left renal vein and its branches protruding to the inferior vena cava, with à thickening of the renal fascia, and infiltration of peri-renal fat, with no signs of renal or prirenal abscess (Figure. 1).
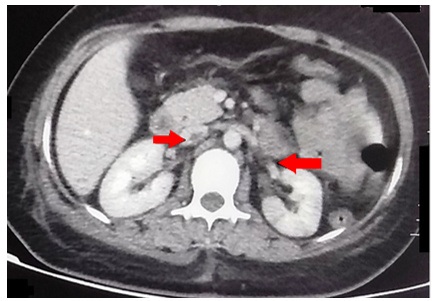
Figure 1. CT scan abdomen axial image shows thrombosis of the left renal vein and the inferior vena cava, (red arrow)
The patient was treated with intravenous ceftriaxone (2g/d) for 14 days, combined with gentamycin (160mg/d) for 48 hours. An anticoagulation treatment was initiated with Low Molecular Weight Heparin (Enoxaparin sodium 0, 6 UI/12h), which was transitioned to oral rivaroxaban, a non-vitamin K antagonist oral anticoagulant (15 mg/12h).
The patient improved after intravenous antibiotics and anticoagulation treatment, she became asymptomatic and afebrile the third day of her hospitalization with gradual reduction of inflammatory markers; she was discharged after 14 days of inpatient hospitalization. At 1-month follow-up, the patient was asymptomatic. At 3 months follow-up, CECT showed complete resolution of the IVCT and attenuated renal vein with atrophic small kidney.
Discussion
Renal vein thrombosis (RVT) is an unusual complication of acute pyelonephritis and only few cases are described in the literature. The most common cause of RVT is nephrotic syndrome notably membranous nephropathy secondary to urinary losses of anticoagulant proteins [1,2]. Other etiologies include renal cell carcinoma, renal transplantation, antiphospholipid antibody syndrome, lupus, trauma, postpartum, oral contraceptive use, xanthogranulomatous pyelonephritis and sepsis [3]. In contrast with thrombosis in other contexts, the cause of the thrombosis during infection is the inflammation triggered by pathogen which is common in gram-negative septicaemia. These gram-negative bacteria release their endotoxin and promote thrombosis by inducing an endothelial surface change (less anticoagulant), increasing the expression of the gene encoding tissue factor (a procoagulant molecule) and rising endothelial cell production of the fibrinolytic inhibitor plasminogen activator inhibitor-1 (PAII) [3, 4]. It is difficult to diagnose RVT or IVCT in the presence of pyelonephritis because both clinical conditions are characterized by fever, haematuria and flank pain [1]. Our patient was initially treated with antibiotics only; when the patient did not respond to antibiotic therapy, a CT scan with intravenous iodine contrast was done and showed extensive thrombosis of the left renal vein and its branches protruding to the inferior vena cava. A high index of suspicion is needed in such cases to diagnose RVT and IVCT, especially in adults without any previous illness [5]. Diagnosis of RVT can be made by ultrasonography, CT scan or magnetic resonance imaging (MRI). Doppler ultrasonography (US) is operator dependent and present a sensitivity of 85% and specificity of 56% [6]. CT scan will demonstrate a thrombus in the renal vein. MRI is as effective as CT scan for diagnosing RVT and has several advantages (good safety profile with no evidence of nephrotoxicity and no need for radiation), so this test can be repeated for follow-up purposes [7]. Many studies have linked the improvement of thrombosis with the resolution of abscess and infection focus. However, in addition to source control, the combination of antibiotics and anticoagulation is important and beneficial in most patients as it can prevent pulmonary embolism, thrombosis of the inferior vena cava, renal failure, renal atrophy and papillary necrosis. Low Molecular Weight Heparin, warfarin or non-vitamin K antagonist oral anticoagulants are effective as illustrated in some case reports [8,9]. Duration of anticoagulation is 3 months like other provoked VTE (venous thrombo embolism). The thrombotic risk induced by the infection decreases spontaneously after several weeks. Therefore, the recurrence rate after anticoagulation has been discontinued is less than that for patients with VTE, suggesting renal vein thrombosis is a distinct clinical entity associated with its underlying cause [10].
Discussion
This case of a young 35-year-old female with no significant past medical history, highlights the need to recognise renal vein thrombosis and inferior vena cava as complications of acute pyelonephritis, even in patients with no risk factors. One should keep in mind the possibility of RVT in cases of unresolved pyelonephritis, because sepsis can create a predisposed environment for hypercoagulability. Moreover, it may trigger the coagulation cascade for thrombus formation. Treatment consists of managing the infection and anticoagulation.
Conflict of interests: The authors have declared that no conflict of interest exists.
References
- Fadeyi O, Gupta L, Sovyanhadi Z, et al. (2023) Thrombosis, Septic Emboli, and Multiple Abscesses Triggered by Klebsiella pneumoniae: A Case Report and Review of Literature. J Investig Med High Impact Case Rep. 11: 23247096231179441. [PubMed.]
- Kumar S, Singh SK, Mavuduru RS, Acharya NC, Agarwal MM, et al. (2009) Acute pyelonephritis with renal vein and inferior vena cava thrombosis in a case of hyperhomocysteinemia. Int Urol Nephrol. 41(1): 185-188. [PubMed.]
- Czaja CA, Scholes D, Hooton TM, Stamm WE. (2007) Population-based epidemiologic analysis of acute pyelonephritis. Clin Infect Dis. 45: 273-280. [PubMed.]
- Lurz KL, Hanna DN, Mcgreen BH, et al. (2018) A rare case of renal vein thrombosis secondary to Klebsiella pneumoniae pyelonephritis: a case report. Urol Ann. 10: 103-105. [PubMed.]
- Harris LA, Van Every MJ, Fundell LJ. (2012) Acute bilateral renal vein thrombosis secondary to sepsis from pyelonephritis. Int Braz J Urol. 38(1): 132-134. [PubMed.]
- Wolak T, Rogachev B, Tovbin D. (2005) Renal vein thrombosis as a presenting symptom of multiple genetic procoagulant defects. Nephrol Dial Transplant. 20: 827-829. [PubMed.]
- Bassilos N, Tassart M, Restoux A, et al. (2004) Inferior vena cava thrombosis due to acute pyelonephritis. Nephrol Dial Transplant. 19: 981-983. [PubMed.]
- Llach F. (1985) Hypercoagulability, renal vein thrombosis, and other thrombotic complications of nephrotic syndrome. Kidney Int. 28: 429-439. [PubMed.]
- Jain A, Mehra K, Manikandan R, Dorairajan LN. (2019) Renal vein and vena caval thrombus: a rare presentation of emphysematous pyelonephritis. BMJ Case Rep. 12(9): e231455. [PubMed.]
- Semeraro N, Ammollo CT, Semeraro F, Colucci M. (2010) Sepsis-associated disseminated intravascular coagulation and thromboembolic disease. Mediterr J Hematol Infect Dis. 2: e2010024. [PubMed.]