>Corresponding Author : I Atlas
>Article Type : Case Report
>Volume : 4 | Issue : 6
>Received Date : 23 March, 2024
>Accepted Date : 03 April, 2024
>Published Date : 08 April, 2024
>DOI : https://doi.org/10.54289/JCRMH2400127
>Citation : Ettagmouti Y, Atlas I, Hayar S and Habbal R. (2024) Non-Obstructive Thrombosis of Mechanical Mitral Prosthesis: About a Case Report and Literature Review. J Case Rep Med Hist 4(6): doi https://doi.org/10.54289/JCRMH2400127
>Copyright : © 2024 Ettagmouti Y, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Case Report | Open Access | Full Text
Cardiology Department, Ibn Rochd hospital university, Casablanca, Morocco
*Corresponding author: I Atlas, Cardiology Department, Ibn Rochd hospital university, Casablanca, Morocco
Abstract
Introduction: Mechanical mitral valve prostheses are vital for patients with mitral valve disease. While obstruction is a well-recognized complication, non-obstructive dysfunction remains less understood. We present a case of non-obstructive mechanical mitral prosthesis to highlight its clinical importance and management challenges.
Case Presentation: A 45-year-old female, who had undergone mechanical mitral valve replacement 9 years prior, presented with dysarthria and facial paralysis. Transthoracic echocardiography revealed preserved prosthesis function with no apparent obstruction. However, transesophageal echocardiography confirmed the non-obstructive thrombosis of the mitral prothesis. We opted for a medical treatment consisting in optimizing anticoagulation with the addition of aspirin. The evolution was favorable with complete regression of the thrombus at the control TEO.
Discussion: Non-obstructive mechanical mitral prosthesis is a rare entity, often characterized by atypical symptoms. This case emphasizes the importance of comprehensive assessment beyond prosthetic valve gradients. as well as the importance of combining several imaging methods, including radio cinema and TEO. Surgical intervention wasn’t necessary, as the medical treatment was sufficient.
Conclusion: Non-obstructive mechanical mitral prosthesis dysfunction can be challenging to diagnose but is crucial to consider in symptomatic patients with mechanical valves. This case underscores the need for a multidimensional approach, including advanced imaging techniques, to uncover and manage non-obstructive prosthesis dysfunction, ultimately improving patient outcomes and quality of life.
Keywords: Thrombosis; Non-Obstructive; Mechanical Mitral Valve; Case Report
Abbreviations: TEE: Transesophageal Echocardiography, CT: Computed Tomography, MRI: Magnetic Resonance Imaging, INR: Index National Ratio
Introduction
Prosthesis thrombosis is a relatively rare entity, but it can be very serious, threatening the patient's vital prognosis. There are two types of prosthesis thrombosis: obstructive and non-obstructive. Non-obstructive prosthetic valve thrombosis is frequently detected by transesophageal echocardiography (TEE), which is the method of choice for detecting the thrombosis of prosthetic valves [1]. The frequency, clinical significance, and outcome of this event are not clear, which makes treatment difficult [2]. We aim to report the clinical and radiological of this case in order to clarify the attitude to adopt when faced with non-obstructive prosthetic mitral valve thrombosis.
Case presentation
We describe the case of a 45-year-old female who underwent mitral valve replacement for very tight mitral narrowing in 2014 with a Saint-Jude double-fin prosthesis with tricuspid plasty, with a history of ischemic stroke in 2016 on antivitamin K (VKA) based anticoagulation, who presents to the emergency department with dysarthria and facial paralysis evolving since 48h.
Clinical examination revealed a conscious patient 15/15, normotensive to 127/72 mmHg, normocardial to 67 bpm, who was 98% saturated with air, with no clinical signs of heart failure.
The electrocardiogram showed atrial fibrillation at 60 bpm with no repolarization disorders.
Cerebral computed tomography (CT) scan revealed a subacute left capsulothalamic ischemic lesion with no hemorrhagic infarction.
Cerebral magnetic resonance imaging (MRI) revealed several bilateral ischemic lesions of different ages with no abnormalities on the angiographic sequences.
Ultrasound of the supra-aortic vessels revealed diffuse atheromatous disease with no significant stenosis or hemodynamic impact.
Transthoracic echocardiography revealed a non-dilated, non-hypertrophied left ventricle with good global and segmental contractility; ejection fraction was 57% in Simpson biplane. The mechanical double-winged prosthesis in the mitral position with good mobility, mean gradient was at 4 mmHg, patency index was 0. 95, effective valve area was 2.1cm2, mitral E wave of 1.07 m/s, and absence of any thrombus detectable or cardiac vegetation. Right ventricle function was altered; excursion of the tricuspid ring at 14mm. There was no pulmonary hypertension or significant aortic valve disease.
A radio cinema was performed (figure 1), revealing a well-functioning mechanical prosthesis with good opening and closing of its wings.
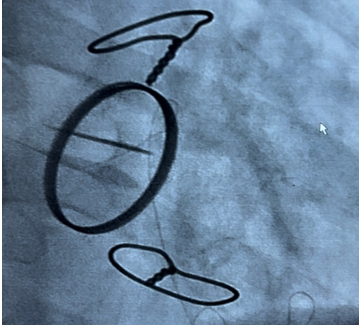
Figure 1: Radio-cinema showing wings of valve mitral prothesis in full opening.
Biological workup on admission showed Hemoglobin 13.8g/dl, normal Leukocytes 8730/mm3, Platelets 234000/mm3, creatinine 8.2mg/L estimating GFR 80ml/min and index national ratio (INR) at 3.22 with Prothrombin 21% with negative protein c reactive (<2mg/ L).
Transesophageal echocardiography (figure 2) showed good mitral valve prosthesis mobility, good wings opening and a non-obstructive thrombus of 4*6 mm on the atrial side of the prosthesis without significant gradient (mean gradient 3.78mmHg).
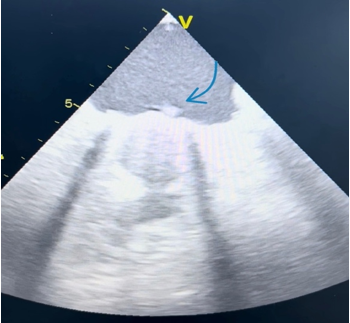
Figure 2: Radio-cinema showing wings of valve mitral prothesis in full opening.
The biological curve of previous INRs over the last two years was in the therapeutic range between 2.5 and 3.5. We decided to increase the target INR to between 3 and 4, with the addition of 160mg aspirin per day because of the small size of non-obstructive thrombosis of the mitral valve prosthesis.
A follow-up transesophageal ultrasound (figure 3) was performed after 1 month, showing complete disappearance of the thrombus. We therefore decided to maintain an INR of between 3 and 4, while continuing to take aspirin at a daily dose of 160mg.
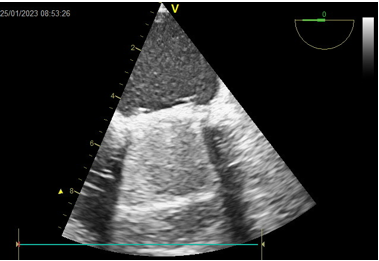
Figure 3: Radio-cinema showing wings of valve mitral prothesis in full opening.
Discussion
Thrombosis of mechanical valve prostheses is a dreadful complication that can occur early or late postoperatively. The incidence of thrombosis in mechanical valve (and also in biological one) is between 0.1 and 5.7% pts/year in patients with uncorrected anticoagulant therapy [3,4]. This risk is higher in patients older than 50 years old, with spherical prosthesis (disused nowadays), with prosthesis in mitral position, with altered left ventricular ejection fraction, in patients with association of atrial fibrillation and a severely dilated left atrium [5].
The most serious form of prosthesis thrombosis is obstructive thrombosis, which can rapidly lead to an intra-cardiac obstruction causing life-threatening hemodynamic instability. Non-obstructive thrombosis is not always benign; it often has a better prognosis and may be the cause of several systemic thromboembolic events, which may be the mode of revelation of this pathology, as in the case of our patient.
The role of transesophageal echocardiography is essential to distinguish malfunctioning due to prosthesis obstruction or to prosthetic thrombosis with blocked moving parts or thrombosis with preserved mobile elements excursion [6].
Medical or surgical treatment are two options to be seriously considered in the event of non-obstructive thrombosis of mechanical prostheses, each with its own indications and limitations [7,8]. Management of non-obstructive prothesis thrombosis is primarily medical: heparin therapy and equilibration of vitamin K antagonist therapy, and in some cases, if the patient is well anticoagulated, an antiplatelet agent (usually aspirin) can be added. Surgery may be considered in the event of a large (> 10 mm), mobile clot, especially if it increases despite optimization of medical treatment. Some authors have also proposed fibrinolysis, but this is not safe from the risk of embolism [9-13].
In our patient's case, in line with the literature, given that the thrombus was small (less than 10mm) and not very mobile, and given that she was well anticoagulated, we opted to increase the therapeutic target of her INR (current target between 3 and 4), with the addition of 100mg of aspirin per day, while making the patient aware of the risk of bleeding. As shown in the presentation above, the evolution was marked by the disappearance of the thrombus at the one-month follow-up transesophageal echocardiogram, with no notable hemorrhagic events.
Conclusion
In conclusion, this case report sheds light on the rare yet clinically significant occurrence of non-obstructive mitral valve thrombosis. While typically overshadowed by obstructive forms of thrombosis, non-obstructive thrombi can pose diagnostic and management challenges. Through a thorough analysis of this case, we underscore the importance of considering this entity in the differential diagnosis of patients with mitral valve pathologies. Early detection, careful monitoring, and tailored anticoagulation strategies are essential in preventing embolic complications and improving patient outcomes. Further research and awareness in this area are crucial for enhancing our understanding and management of non-obstructive mitral valve thrombosis.
Consent for publication: Written informed consent was obtained from the patient for publication of this case report and any accompanying images.
Ethical approval: As international standard, written ethical approval has been collected and preserved by the authors.
Availability of data and material: All data generated or analyzed during this study are included in this published article.
Competing interests: The authors declare that they have no competing interests.
Author contributions: This work was carried out in collaboration among all authors:
Y. Ettagmouti: writing paper;
I. Atlas: study concept literature;
S. Hayar: care of the patient;
R. Habbal: Interpretation and analysis.
References
- Alton ME, Pasierski TJ, Orsinelli DA, Eaton GM, Pearson AC. (1992) Comparison of transthoracic and transesophageal echocardiography in evaluation of 47 Starr-Edwards prosthetic valves. J Am Coll Cardiol. 20: 1503-1511. [PubMed.]
- Vahanian A, Baumgartner H, Bax J, Butchart E, Dion R, et al. (2007) Guidelines on the management of valvular heart disease. European Heart Journal. [PubMed.]
- Tang GH, Rao V, Siu S, Butany J. (2005) Thrombosis of mechanical mitral valve prosthesis. J Card Surg. 20(5): 481-486. [PubMed.]
- Bottio T, Gerosa G, Basso C, Thiene G, Casarotto DC. (2002) Unexpected mechanical bileaflet valve thrombosis in mitral position: what is better to do, re-replacement or thrombolysis. Langenbeck's Arch Surg. 387: 166-169. [PubMed.]
- Martinel J, Jiminez A, Rabago G, Artiz V, Fraile J, et al. (1991) Mechanical cardiac valve thrombosis: is thrombectomy justified? Circulation. 84(suppl III): 70-75. [PubMed.]
- Lus P, Giacomin A, Cavarzarani A, Valfrè C. (1994) Detection of acute thrombosis of mitral tilting disk prosthesis by transesophageal echocardiography. Int J Card Imaging. 10(4): 305-308. [PubMed.]
- Silber H, Khan SS, Matloff JM, Chaux A, De Robertis M, et al. (1993) The St. Jude valve: thrombolysis as the first line terapy for cardiac valve thrombosis. Circulation. 87: 30-37. [PubMed.]
- Rizzoli G, Guglielmi C, Toscano G, Pistorio V, Vendramin I, et al. (1999) Reoperation for acute prosthetic thrombosis and pannus: an assesment of rates, relationship and risk. Eur J Cardiothorac Surg. 16(1): 74-80. [PubMed.]
- Roudaut R, Dijos M, Réant P et al. (2014) Complications thromboemboliques des prothèses valvulaires. Modalités diagnostiques et thérapeutiques. In:” Cardiopathies valvulaires de l’adulte”. Lavoisier, Médecine Sciences. 596-603. [PubMed.]
- Roudaut R, Serri K, Lafitte S. (2007) Thrombosis of prosthetic heart valves: diagnosis and therapeutic considera-tions. Heart. 93: 137-142. [Ref.]
- Gürsoy Mo, Kalçik M, Yesin M et al. (2016) A global perspective on mechanical prosthetic heart valve thrombosis: Diagnostic and therapeutic challenges. Anatol J Cardiol. 16: 980-989. [PubMed.]
- Poli D, Antonucci E, Pengo V et al. (2018) Italian Federation of Anticoagulation Clinics. Mechanical prosthetic heart valves: Quality of anticoagulation and thromboembolic risk. The observa-tional multicenter Plectrum study. Int J Cardiol. 267: 68-73. [PubMed.]
- Dangas Gd, Weitz Ji, Giustino G, et al. (2016) Prosthetic Heart Valve Thrombosis. J Am Coll Cardiol. 68: 2670-2689. [PubMed.]