>Corresponding Author : Janice Lim Wan Lin
>Article Type : Case Report
>Volume : 4 | Issue : 5
>Received Date : 11 March, 2024
>Accepted Date : 23 March, 2024
>Published Date : 27 March, 2024
>DOI : https://doi.org/10.54289/JCRMH2400124
>Citation : Cheng YL, Lim JWL. (2024) Assessing Expected Neurological Deficit with Spinal Anesthetic Before Removal of Spinal Needle – A Case of Failed Spinal Anesthesia Due to Drug Failure. J Case Rep Med Hist 4(5): doi https://doi.org/10.54289/JCRMH2400124
>Copyright : © 2024 Cheng YL, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Case Report | Open Access | Full Text
1Consultant, Department of Anesthesiology, Ng Teng Fong General Hospital
2Medical Officer, Department of Anesthesiology, Ng Teng Fong General Hospital
*Corresponding author: Janice Lim Wan Lin, Medical Officer, Department of Anesthesiology, Ng Teng Fong General Hospital
Keywords: Spinal Anesthesia; Regional Anesthesia; Drug Failure
Abbreviations: CSF: Cerebrospinal Fluid
Introduction
We report a novel way of performing spinal anesthetics.
Instead of removing the needle immediately after injecting local anesthetic LA (traditional method), we propose keeping the spinal needle in-situ while determining if the block is truly working.
We saved a patient from painful experiences of a failed spinal, repositioning, more injections or conversion to general anaesthesia.
We could apply this new method to troubleshoot and manage in other scenarios.
Case Description
Our patient is an 89-year-old lady with past medical history of atrial fibrillation, cardiomyopathy (ejection fraction 48-55%), tricuspid regurgitation, pulmonary hypertension.
She had fractured her left neck of femur and was planned for bipolar arthroplasty. She consented for central neuraxial block.
Spinal anesthesia was performed in right lateral decubitus. Midline approach through L4/5 space yielded good cerebrospinal fluid (CSF) flow. Intrathecal 2.5ml 0.5% PLAIN bupivacaine was given via 25G Quincke spinal needle. Smooth aspiration of CSF was seen.
The stylet was reinserted (without moving needle) to prevent CSF and LA from leaking.
After 10 minutes, she did not develop any weakness or numbness. No sedation was given.
Intrathecal 2.5ml 0.5% HEAVY bupivacaine was given through the needle in-situ. CSF was flowing and aspiration was easy. Bilateral lower limbs sensory and motor loss and sensory level T10/11 was achieved within 1-2 minutes of administration. Her operation was uneventful.
In view of another recent case with failed spinal anesthesia using 0.5% plain bupivacaine, there was high suspicion of drug failure. The bupivacaine batch was within expiry and has been quarantined for investigation by hospital pharmacy.
Discussion
How to troubleshoot failed spinal [1,2]
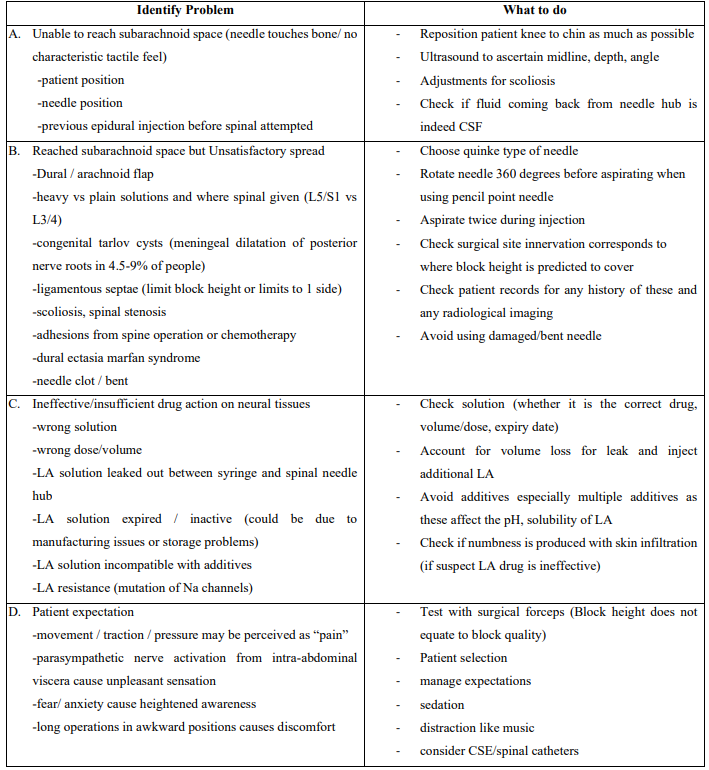
Figure 1: Histopathological examinations of the core liver biopsy specimens revealed hepatocellular carcinoma: positive expression of cytokeratin AE1/AE3 antibodies (A: H&E, 100×) and synaptophysin (B: H&E, 10×).
Advantages of needle kept in-situ method
1. Less wastage of time, sterile equipment, patient discomfort in event of repeat spinal injection
2. We can ascertain if needle is intrathecal (bedside CSF glucose testing)
3. We can top up intrathecal medication (more LA, different LA, opioids)
4. We can use it to barbotage to increase block height
The onset of intrathecal bupivacaine is usually within 5-8 minutes [3]. The smaller autonomic fibers are blocked first, followed by sensory and lastly motor [4]. In patients who do not report any sensory or motor loss within 10-15 minutes, clinicians should suspect failed spinal anesthesia.
Spinal failure due to ineffective LA is not uncommon [1]. AstraZeneca received 562 ‘product defect notification’ reports in 6 years to Dec 21, 2007, all ascribing failed spinal to ineffective bupivacaine from every country it was marketed. The numbers could be higher from under reporting.
Conclusion
By leaving the spinal needle in-situ until the assessment of the spinal anaesthsia is complete allows time and opportunity for the anesthetist to troubleshoot a failed spinal anesthesia.
Acknowledgements
We have the written consent from our patient. No external funding nor competing interests.
Conflicts of Interest: The authors declare no conflicts of interest
References
- P W D Fettes. (2009) Failed spinal anaesthesia: mechanisms, management, and prevention BJA .102(6): 739-748. [PubMed.]
- Keten S Parikh, S Seethatramaiah. (2018) Approach to failed spinal anaesthesia for caesaren section IJA. 62(9): 691-697. [Ref.]
- Olawin AM, Joe MD. (2022) Spinal Anesthesia - StatPearls - NCBI Bookshelf. [Ref.]
- Tomes S. (2023) Differential Spinal Blockade. Openanesthesia. [Ref.]