>Corresponding Author : Pankaj Kumar
>Article Type : Case Report
>Volume : 4 | Issue : 3
>Received Date : 28 Jan, 2024
>Accepted Date : 12 Feb, 2024
>Published Date : 16 Feb, 2024
>DOI : https://doi.org/10.54289/JCRMH2400115
>Citation : Kumar P, Shakya S, Singh H and Singh K. (2024) Dengue Fever with Hemolysis: Unmasking Beta-Thalassemia. J Case Rep Med Hist 4(3): doi https://doi.org/10.54289/JCRMH2400115
>Copyright : © 2024 Kumar P, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Case Report | Open Access | Full Text
1Junior Resident, Government Medical College, Chandigarh, India
2Junior Resident, Government Medical College, Chandigarh, India
3Senior Resident, Government Medical College, Chandigarh, India
4Professor, Government Medical College, Chandigarh, India
*Corresponding author: Pankaj Kumar, Junior Resident, Government Medical College, Chandigarh, India
Abstract
Intravascular hemolysis is a rare but known complication of Dengue infection. Following is the description of a patient who presented with features of intravascular hemolysis with other sequelae of Dengue infection. Clinical stigmata of chronic iron overload led to a search for the aetiology of chronic hemolysis, which resulted in a diagnosis of non-transfusion-dependent beta-thalassemia.
Keywords: Secondary Iron Overload; Intravascular Hemolysis; Medicine in Resource Limited Areas; Complications of Dengue Fever; Β-Thalassemia
Abbreviations: EDS: Expanded Dengue Syndrome, DHF: Dengue Hemorrhagic Fever, DF: Dengue Fever, DSS: Dengue Shock Syndrome, AIH: Acute Intravascular Hemolysis, G6PD: Glucose-6-Phosphate Dehydrogenase
Introduction
Expanded Dengue Syndrome (EDS) is a novel term coined by the World Health Organization (WHO) to include manifestations of Dengue infection that do not fit into the categories of Dengue Fever (DF), Dengue Hemorrhagic Fever (DHF) or Dengue Shock Syndrome (DSS) [1]. Hemolysis is a rare complication in EDS with an unclear pathogenesis. Both immune and non-immune hemolytic anemia have been reported in the literature to be associated with EDS [2-4].
This young gentleman had never contracted adequate medical care due to socio-economic limitations. At presentation, the clinical resemblance was with EDS with intravascular hemolysis. However, upon historical and ancillary investigations, beta-chain hemoglobinopathy was detected.
Case Presentation
A 50-year-old patient with Behçet's disease inaugurated at the age of 49 by bipolar aphthosis and revealed by vascular involvement consisting of deep venous thrombosis of the left lower limb and ocular involvement consisting of bilateral panuveitis, for which he received high-dose corticosteroid therapy, azathioprine and oral anticoagulation with good improvement. One year later, the patient presented with deep vein thrombosis of both lower limbs, with loss of consciousness and paraparesis, concomitant with an attack of mouth ulcers. Cerebral-medullary MRI revealed multiple segmental arterial stenoses of inflammatory appearance in the cerebrum, and spondylodiscitis of probably tuberculous origin centred on D12 with vertebral compression in the medulla. in addition to the vascular work-up, a fortuitous discovery of bilateral proximal pulmonary embolism with no impact on the cardiac chambers, no focus of pulmonary infarction, no image of an aneurysm or focus of pleuropulmonary tuberculosis. Therapeutic options were limited by the presence of tuberculous spondylodiscitis. The evolution was very satisfactory, with improvement in motor deficit, loss of consciousness, deep vein thrombosis and pulmonary embolism. The follow-up brain MRI came back without any particularities.
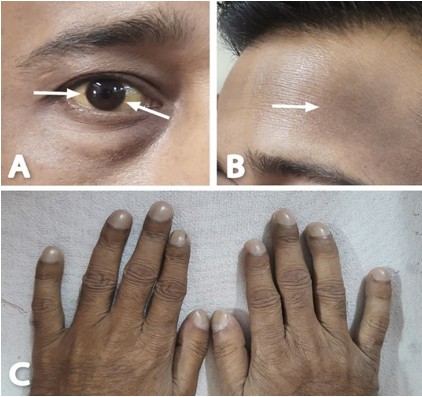
Figure 1: Patient images depicting A: Icterus and limbic iron deposits (arrows), B: Brownish discoloration of forehead skin, C: Grade 3 digital clubbing.
Routine investigation results are summarised in Table 1.
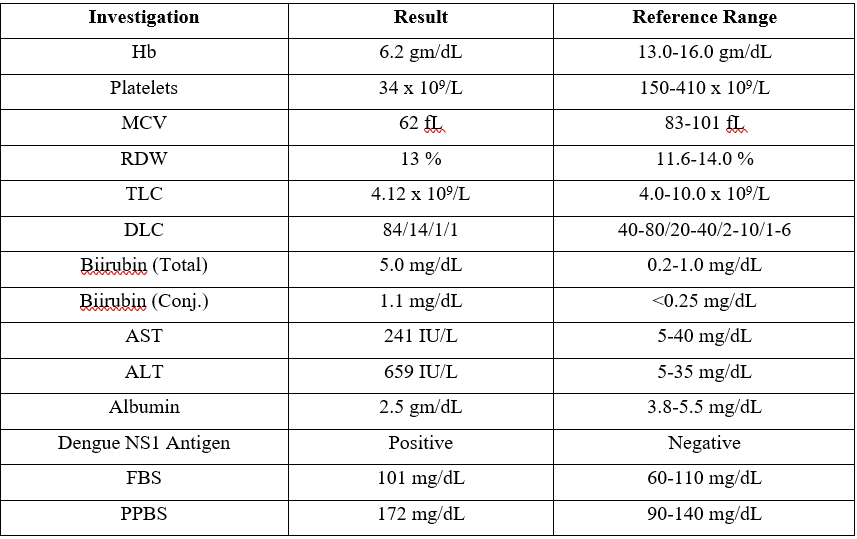
Table 1: Laboratory investigation results at presentation
Peripheral blood film: Microcytes, tear drop cells, target cells and giant platelets were seen. Schistocytes and Malarial parasite were absent (Figure 2A). Rapid diagnostic test for Malaria was also negative. Coagulation profile was normal. 2D transthoracic echocardiogram was suggestive of mild mitral regurgitation with normal cardiac chambers. USG Abdomen: Liver size 16.5 cm, Spleen size: 14 cm, Portal vein normal, no ascites (Figure 2B, 2C).
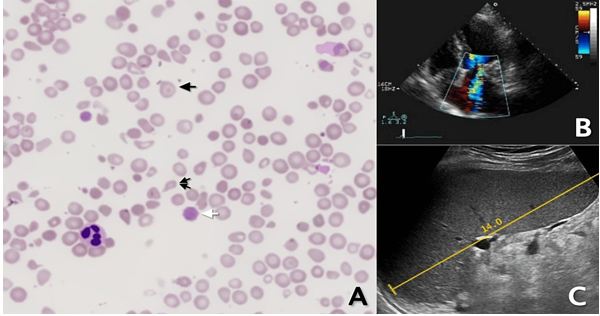
Figure 2: A: Peripheral blood film showing target cells (black arrow), giant platelets (white arrow), teardrop cell (double arrows), B: 2D echo showing MR jet, C: USG abdomen showing splenomegaly.
Hemolytic workup revealed non-immune Acute Intravascular Hemolysis (AIH) with elevated urine and plasma hemoglobin concentrations, and negative Coombs' test. Glucose-6-phosphate dehydrogenase (G6PD) levels and Hemoglobin electrophoresis were performed due to evidence of chronic hemolysis and iron overload (cutaneous and corneal deposits, Impaired blood sugar levels, abnormal cardiovascular examination). The results were the following (Table 2).
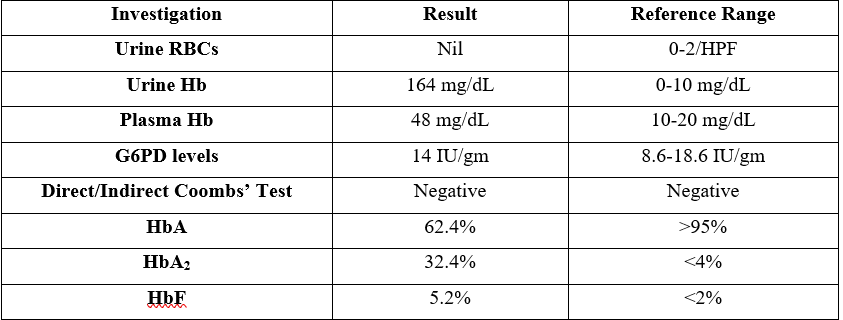
Table 2: Results of hemolytic workup
Profile correlated with non-transfusion dependent beta-thalassemia (formerly beta-thalassemia intermedia). The patient was managed with IV crystalloids, antipyretics, and transfusion of 2 units of packed Red Cells (pRBC). Urine color cleared spontaneously on Day 2 of admission and all lab parameters normalised by Day 5. The patient was subsequently discharged with an Hb level of 8.6 gm/dL and was then lost to follow-up.
Discussion
Infection by any of the four dengue serotypes may be asymptomatic or lead to classic dengue fever (DF) or more severe forms of the disease, DHF and DSS. Other manifestations of Dengue infection are classified as EDS. The patient was managed as per the WHO guidelines for treatment of Dengue infection [1].
The patient had an otherwise uneventful dengue infection. Notable abnormalities were thrombocytopenia and hepatitis. Pre-existing hemoglobinopathy (which is primarily responsible for extravascular hemolysis) could have acted as a substrate for precipitation of intravascular hemolysis or AIH could have been solely attributable to dengue infection.
Existing case reports on hemolysis in dengue describe non-immune AIH more commonly than Coombs' positive AIH. The syndrome is self-limiting, and patients have been successfully managed with crystalloids and forced diuresis. Ruling out other common causes of AIH is paramount before labelling it as a manifestation of EDS [2-4].
Other causes for hemolysis with hemoglobinuria such as autoimmune hemolytic anaemia, falciparum malaria, microangiopathic hemolytic anaemia, incompatible blood transfusions, G6PD deficiency, and ingestion of aniline dyes or other poisons were excluded by a combination of history, examination, and laboratory investigations.
Literature on Dengue in Thalassemia patients is also sparse. The common verdict is that anaemia rather than haemoconcentration is to be expected. Markedly increased AST levels compared to ALT, and severe dengue, especially severe liver involvement, is common [5,6].
The patient was a daily-wage labourer, an immigrant and originally hailed from a tribal area. It has been observed amongst some non-tribal and tribal communities, that the prevalence of beta-thalassemia carriers is much higher (5.3-17.0%) than the projected national average of 3-4% [7].
He had a history of poor exercise tolerance compared to his peers but never considered seeking medical care for the same. This healthcare contact provided a unique opportunity to detect a chronic illness which when adequately managed can significantly improve the patient's quality of life. His previous alleged admission 3 years ago for a similar history might have uncovered the existence of thalassemia but medical records from that time were not available with the patient. Similar events may unfold again in the future unless the records are preserved.
Conclusion
This case report highlights some important medical lessons: emphasis on history and examination in resource-limited settings, pattern recognition, limited healthcare reach to underprivileged classes, and benefits of individualising management rather than managing as a part of a cohort, especially during high burden epidemics as most of the cases of dengue infection are concentrated around a few months of the year. Fall in hemoglobin in dengue infection should alert the physician towards the possibilities of mucosal bleed and hemolysis. Similarly, thalassemia patients with dengue present with anaemia rather than hemoconcentration. Thus, in diagnosed cases of thalassemia, these atypical manifestations should point towards suspicion for dengue. Hemolysis in dengue may require even more liberal crystalloid infusions to prevent nephropathy along with monitoring for fluid overload as 3rd space losses due to capillary leak is a common phenomenon.
References
- Whitehorn J, Simmons CP. (2011) The pathogenesis of dengue. Vaccine. 23: 7221-7228. [Ref.]
- Medagoda K, Gunathilaka SB, De Silva HJ. (2003) A case of self-limiting Coomb's negative haemolytic anaemia following dengue shock syndrome. Ceylon Med J. 48: 147-148. [PubMed.]
- Aye M, Cabot J, William LWK. (2016) Severe Dengue Fever with Haemolytic Anaemia-A Case Study. Trop Med Infect Dis. 1(1): 6. [Ref.]
- Sellahewa KH, Kumaratne MP, Halpe S, Marapana K. (2020) Case Report: A Case of Acute Intravascular Hemolysis in Dengue Fever. Am J Trop Med Hyg. 102: 355-358. [Ref.]
- Natesirinilkul R, Tantiworawit A, Charoenkwan P. (2013) Clinical course of dengue in patients with thalassaemia. Paediatr Int Child Health. 33: 32-36. [PubMed.]
- Pongtanakul B, Narkbunnam N, Veerakul G, et al. (2005) Dengue hemorrhagic fever in patients with thalassemia. J Med Assoc Thai. 88: 8. [PubMed.]
- Colah RB, Gorakshakar A. (2014) Control of Thalassemia in India. Thalassemia Reports. 4(2): 1955. [Ref.]