>Corresponding Author : Safaa Mourabit
>Article Type : Case Report
>Volume : 4 | Issue : 2
>Received Date : 22 Jan, 2024
>Accepted Date : 03 Feb, 2024
>Published Date : 08 Feb, 2024
>DOI : https://doi.org/10.54289/JCRMH2400110
>Citation : Mourabit S, Mhaber S, Elkabli A, Barakat L, Echchilali K, et al. (2024) EBV-Induced Inflammatory Chorioretinitis With Bilateral Retinal Serous Detachment in a Young Immunocompetent Patient. J Case Rep Med Hist 4(2): doi https://doi.org/10.54289/JCRMH2400110
>Copyright : © 2024 Mourabit S, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Case Report | Open Access | Full Text
1Resident Physician, Department of Internal Medicine, Ibn Rochd University Hospital, Casablanca, Morocco
2Professor in the Department of Internal Medicine at the Ibn Rochd University Hospital in Casablanca, Morocco
*Corresponding author: Safaa Mourabit, Resident Physician, Department of Internal Medicine, Ibn Rochd University Hospital, Casablanca, Morocco
Abstract
Epstein-Barr virus (EBV) infection is generally asymptomatic and persists throughout life. Ocular involvement is rare, observed in immunocompromised patients, particularly those infected with HIV, where retinal involvement may occur. Inflammatory chorioretinitis with bilateral retinal serous detachment is a rare entity in EBV infections. This case report describes inflammatory chorioretinitis with bilateral serous retinal detachment in an immunocompetent patient, resulting from Epstein-Barr virus (EBV) infection. Although ocular involvement by EBV is rare in immunocompetent patients, this case highlights the importance of considering this possibility. The patient was successfully treated with acyclovir, highlighting the potential efficacy of antivirals in these situations. This observation highlights the need for early detection to prevent irreversible ocular damage, despite the lack of standard diagnostic algorithms. Optimal clinical management of these cases remains a challenge, underlining the need for further research.
Keywords: Epstein-Barr Virus Infections; Chorioretinitis; Retinal Serous Detachment; Acyclovir; Immunocompetent Patient
Abbreviations: EBV: Epstein-Barr Virus, HIV: Human Immunodeficiency Virus, CMV: Cytomegalovirus, HSV: Herpes Simplex Virus, OCT: Optical Coherence Tomography
Introduction
The Epstein Barr virus is a DNA virus of the herpes family responsible for infectious mononucleosis. Ocular manifestations are rare, and only a few cases involving the posterior segment of the eye have been reported. We report the case of a young immunocompetent patient man with bilateral EBV chorioretinitis and retinal serous detachment.
Case Report
A 32-year-old patient with no prior history presented one month prior to admission with a fever of 39-40 associated with a diffuse rash and bronchial syndrome that resolved with antibiotics.
Three weeks later, the patient suddenly presented with a decrease in visual acuity, bilateral pain and redness, and no other associated clinical manifestations. Ophthalmological examination revealed visual acuity of 4/10 in the OD and 2/10 in the OG, with a whitish retinal patch on the fundus. Angiography: inflammatory chorioretinitis with bilateral macular edema and OCT: inflammatory macular edema with bilateral retinal serous detachment.
Etiological investigations revealed strong positive EBV serology with positive IgM and IgG. A non-exhaustive work-up was requested, including the rest of the serologies, in particular for toxoplasmosis, syphilis, CMV, HSV, as well as a tuberculosis work-up, all of which came back negative.
Treatment with general acyclovir was initiated, with very good progression, with improvement in visual acuity, reapplication of the retina and cleaning of the posterior pole.
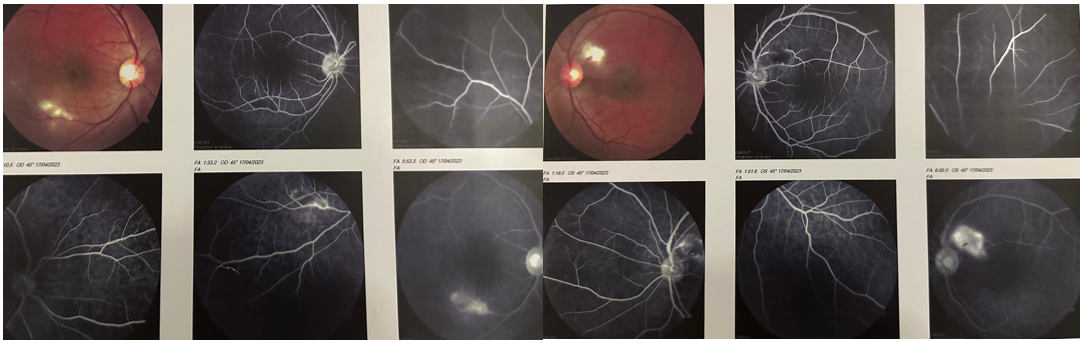
Figure 1: Result of Angiography: inflammatory chorioretinitis with bilateral macular edema
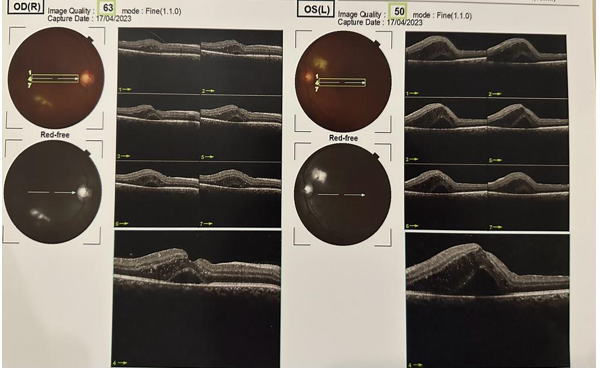
Figure 2: Result of OCT: inflammatory macular edema with bilateral retinal serous detachment
Discussion
Ocular involvement by EBV can include all segments of the eyeball. Posterior pole involvement is not as common an ocular manifestation of this virus as anterior chamber involvement [1,2]. Reported cases to date include conjunctivitis, dacryoadenitis, episcleritis, keratitis, optic neuritis and retinal vasculitis. EBV must be considered in the differential diagnosis, even in immunocompetent patients, leading to the implementation of a mood swab that provides the diagnosis of certainty. The pathogenicity of EBV is well known and it can also cause intraocular inflammation and acute retinal necrosis [3]. However, given its ubiquity, it has also been associated with multiple ocular pathologies ranging from benign conditions to severe visual acuity impairment with retinal detachment. All this has been described in both immunocompetent and immunocompromised patients, including HIV-infected patients where EBV and CMV are responsible for severe necrotizing retinitis [4,5]. Diagnosis of intraocular infection with EBV and other herpesviruses relies on molecular testing, and although genotype detection is not available, it is the only positive test [6,7].
The appropriate management of an unknown condition, such as ocular EBV disease, is unclear, as there are no clinical trials on this type of case. Identification of the virus leads to the use of antivirals, particularly in patients with a high viral load [8]. Andersson et al [9]. found a significant decrease in the spontaneous growth of EBV-infected B lymphocytes in vivo after treatment with Acyclovir, but given the small number of cases analyzed, the use of this drug is considered questionable. The review by Rafailidis et al [8]. suggests that antiviral agents could be considered for severe manifestations of EBV infections, including meningitis, meningoencephalitis, peripheral nerve palsy, myocarditis, hepatitis and hematopoietic or renal disease in immunocompetent patients, as well as to complement steroid therapy. Nevertheless, there is no description of management with antivirals for ocular involvement, with only one case described by Keorochana [7] in which the use of antivirals showed a similar result to that obtained in the present case. It remains to be established whether the combined use of steroids reduces the progression of the pathology, and whether it is a determining factor in visual loss in these cases. It is not possible to define whether management with oral acyclovir is the best therapeutic option, as there is no extensive literature on case series or clinical trials with other antivirals, and leaves open the possibility of using such a strategy in the management of this condition.
Conclusion
In conclusion, this case report highlights a rare but significant manifestation of Epstein-Barr virus infection in an immunocompetent patient, presenting with inflammatory chorioretinitis with bilateral serous retinal detachment. Although ocular involvement by Epstein-Barr virus is unusual in immunocompetent individuals, it is crucial to consider this possibility in the evaluation of ocular lesions, particularly chorioretinitis. The case described here was successfully treated with acyclovir, highlighting the importance of early detection and appropriate therapeutic intervention to prevent possible irreversible ocular damage. While the lack of diagnostic algorithms and standard guidelines for this specific manifestation underlines the need for further research, this report also highlights the potential efficacy of antivirals in the treatment of this rare condition. In sum, vigilance for ocular involvement of Epstein-Barr virus, even in immunocompetent patients, is crucial for optimal clinical management and preservation of visual function.
References
- Matoba AY. (1990) Maladie oculaire associée à une infection par le virus Epstein-Barr. Surv Ophthalmol. 35(2): 145-150. [PubMed.]
- Santos-Bueso E, Sáenz-Francés F, Méndez-Hernández C, Martínez-de-la-Casa JM, García-Feijoo J, et al. (2014) Papilite par infection par le virus d'Epstein-Barr chez un patient adulte. Arch Soc Esp of talmol. 89(6): 245-249. [PubMed.]
- Schaal S, Kagan A, Wang Y, Chan CC, Kaplan HJ. (2014) Nécrose rétinienne aiguë associée au virus d'Epstein-Barr: confirmation immunohistopathologique. JAMA Ophtalmol. 132(7): 881-882. [PubMed.]
- Hershberger VS, Hutchins RK, Witte DP, Schneider S, Harris RE, et al. (2003) Nécrose rétinienne aiguë bilatérale liée au virus Epstein-Barr chez un patient atteint d'un trouble lymphoprolifératif lié à l'X. Arc Ophthalmol. 121(7): 1047-1049. [Ref.]
- Hollande GN. (1994) Critères diagnostiques standard pour le syndrome de nécrose rétinienne aiguë. Suis J Ophthal-mol. 117(5): 663-667. [PubMed.]
- Janani MK, Malathi J, Biswas J, Sridharan S, Madhavan HN. (2015) Détection génotypique du virus Epstein Barr chez des patients cliniquement suspectés de rétinite virale dans un centre de soins oculaires tertiaires, Inde. Ocul Immunol Inflamm. 23(5): 384-391. [PubMed.]
- Keorochana N. (2016) Un rapport de cas de vascularite rétinienne associée au virus Epstein-Barr: traitement réussi utilisant uniquement un traitement à l'acyclovir. Représentant international du cas médical J. 9: 213-218. [PubMed.]
- Rafailidis PI, Mavros MN, Kapaskelis A, Fala-gas ME. (2010) Traitement antiviral des infections sévères à EBV chez des patients apparemment immunocompétents. J Clin Virol. 49(3): 151-157. [PubMed.]
- Andersson J, Britton S, Ernberg I, Ander-sson U, Henle W, et al. (1986) Effet de l'acyclovir sur la mononucléose infectieuse: une étude en double aveugle contrôlée par placebo. J Infecter Dis. 153(2): 283-290. [PubMed.]