>Corresponding Author : Sai Sandeep V
>Article Type : Case Report
>Volume : 4 | Issue : 2
>Received Date : 15 Jan, 2024
>Accepted Date : 25 Jan, 2024
>Published Date : 29 Jan, 2024
>DOI : https://doi.org/10.54289/JCRMH2400108
>Citation : Sandeep SV, Ahuja I, Rana A, Kumar P and Dhiman A. (2024) Tubercular Meningitis Mimicking Acute Disseminated Encephalomyelitis (ADEM)- A Case Report. J Case Rep Med Hist 4(2): doi https://doi.org/10.54289/JCRMH2400108
>Copyright : © 2024 Sandeep SV, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Case Report | Open Access | Full Text
1Junior Resident, Department of General Medicine, GMCH, Chandigarh, India
2Assistant Professor, Department of General Medicine, GMCH, Chandigarh, India
3Senior Resident, Department of General Medicine, GMCH, Chandigarh, India
*Corresponding author: Sai Sandeep V, Junior Resident, Department of General Medicine, GMCH, Chandigarh, India.
Abstract
Tuberculosis remains endemic in India, and its manifestation in the central nervous system (CNS) poses significant challenges in diagnosis and management. We present a rare case of a 65-year-old male with tubercular meningitis exhibiting atypical features of acute disseminated encephalomyelitis (ADEM). The patient presented with a month-long history of fever, severe headache, altered sensorium, and neurological signs including brisk reflexes, neck rigidity, and bilateral motor weakness. Initial investigations revealed elevated inflammatory markers and abnormal cerebrospinal fluid (CSF) findings consistent with tubercular meningitis. Despite negative CSF culture and nucleic acid amplification tests (NAATs) for Mycobacterium tuberculosis, the patient displayed characteristic asymmetrical bilateral cerebral lesions on MRI suggestive of ADEM. Given the diagnostic ambiguity and a high suspicion of CNS tuberculosis with concurrent ADEM, the patient was treated with anti-tubercular therapy (ATT) and a course of intravenous methylprednisolone followed by oral prednisolone. Subsequent clinical improvement prompted gradual tapering of prednisolone, leading to a full recovery at discharge. This case highlights the complexity of diagnosing CNS tuberculosis coexisting with ADEM, emphasizing the importance of a comprehensive clinical assessment and tailored therapeutic interventions in managing such intricate neurological presentations.
Abbreviations: CNS: Central Nervous System, ADEM: Acute Disseminated Encephalomyelitis, CSF: Cerebrospinal Fluid, NAATs: Nucleic Acid Amplification Tests, ATT: Anti-Tubercular Therapy, VZV: Varicella-Zoster Virus, HSV: Herpes Simplex Virus, EBV: Epstein-Barr Virus, HAV: Hepatitis A Virus, HCV: Hepatitis C Virus, PCR: Polymerase Chain Reaction, MS: Multiple Sclerosis
Introduction
Tuberculosis is endemic in India with an incidence of 210 cases per 100,000 people [1]. Among all cases of TB, 1% occurs in the CNS, and 6% of total extrapulmonary TB in immunocompetent adults affects the CNS [2]. Tuberculosis of the central nervous system (CNS) typically manifests as meningitis and is known to be associated with significant morbidity and mortality [3]. On the other hand, acute disseminated encephalomyelitis (ADEM) is an inflammatory monophasic demyelinating disorder of the CNS [4]. The estimated incidence of ADEM in children varies from 0.07 cases per 100,000 individuals per year in Germany to 0.64 cases per 100,000 individuals per year in Fukuoka, Japan [5]. ADEM typically occurs after an infection or vaccination in children. The precise pathophysiology of ADEM is not fully understood; however, it is hypothesized that the condition involves autoimmune activation of T-lymphocytes against myelin and other self-antigens. Additionally, there may be cross-reactivity between microbial peptides and host peptides, which further contributes to the disease process. As a result, activated T-lymphocytes infiltrate the central nervous system (CNS) and recruit additional mononuclear cells, causing an inflammatory response and subsequent demyelination. This complex interplay between immune cells and self-antigens is thought to be central to the development of ADEM [2]. It is very rare for CNS TB to present with ADEM. In the literature, there are only a few case reports linking Mycobacterium tuberculosis to ADEM. We present a case of Tubercular meningitis which presented with features of ADEM.
Case presentation
A 65-year-old male presented to the emergency department with a one-month history of high-grade fever, severe bilateral headache, and altered sensorium. The headache was described as dull and rated at 8/10 in severity. Although fever responded to medications, it recurred every 5-6 hours. The patient also reported night sweats, myalgia, fatigue, and nausea. On examination, vital signs were stable except for tachycardia and fever. Systemic examination did not reveal any abnormalities. However, neurological examination revealed brisk reflexes in all extremities with extensor plantar reflexes, and neck rigidity was present. Motor examination showed 4/5 power in all extremities, while there was no sensory loss. The patient denied any history of dysphagia, nasal regurgitation, abnormal involuntary movements, blurred vision, diplopia, or bowel/bladder problems.
A routine febrile workup was sent, including blood culture, and the patient was started on Vancomycin and Ceftriaxone empirically. The total leukocyte count was elevated at 29,000/mm3, and CRP levels were raised to 260mg/dl. Blood culture, as well as tests for dengue, malaria, and scrub typhus, came back negative.
MRI of the brain revealed asymmetrical bilateral high-intensity fluffy lesions in the cerebral hemispheres and ganglio-capsular region on T2-weighted and FLAIR images. Lumbar puncture was performed, and the cerebrospinal fluid (CSF) was sent for analysis and culture. The fluid analysis report, received on the fourth day of admission, showed a low glucose level of 18 mg/dl and a very high protein level of 403 mg/dl. Adenosine deaminase levels in the CSF were within normal limits. A contrast-enhanced CT scan of the chest and abdomen did not reveal any abnormalities. CSF culture came out negative. To further investigate the possibility of tuberculosis, CBNAAT (Cartridge-Based Nucleic Acid Amplification Test) was performed on the CSF, but the results were negative. There was no clinical improvement in patient’s clinical status. So due to a high clinical suspicion of tubercular meningitis along with acute disseminated encephalomyelitis (ADEM), the patient was initiated on anti-tubercular therapy (ATT) and IV Methylprednisolone. The patient started showing clinical recovery, and the IV Methylprednisolone was continued at a dose of 1g/day for five days, followed by oral Prednisolone at 35mg/day. Eventually, the patient's clinical condition returned to baseline, and they were on ATT and oral Prednisolone. During a follow-up visit after two weeks, the Prednisolone dose was tapered and eventually discontinued after six weeks.
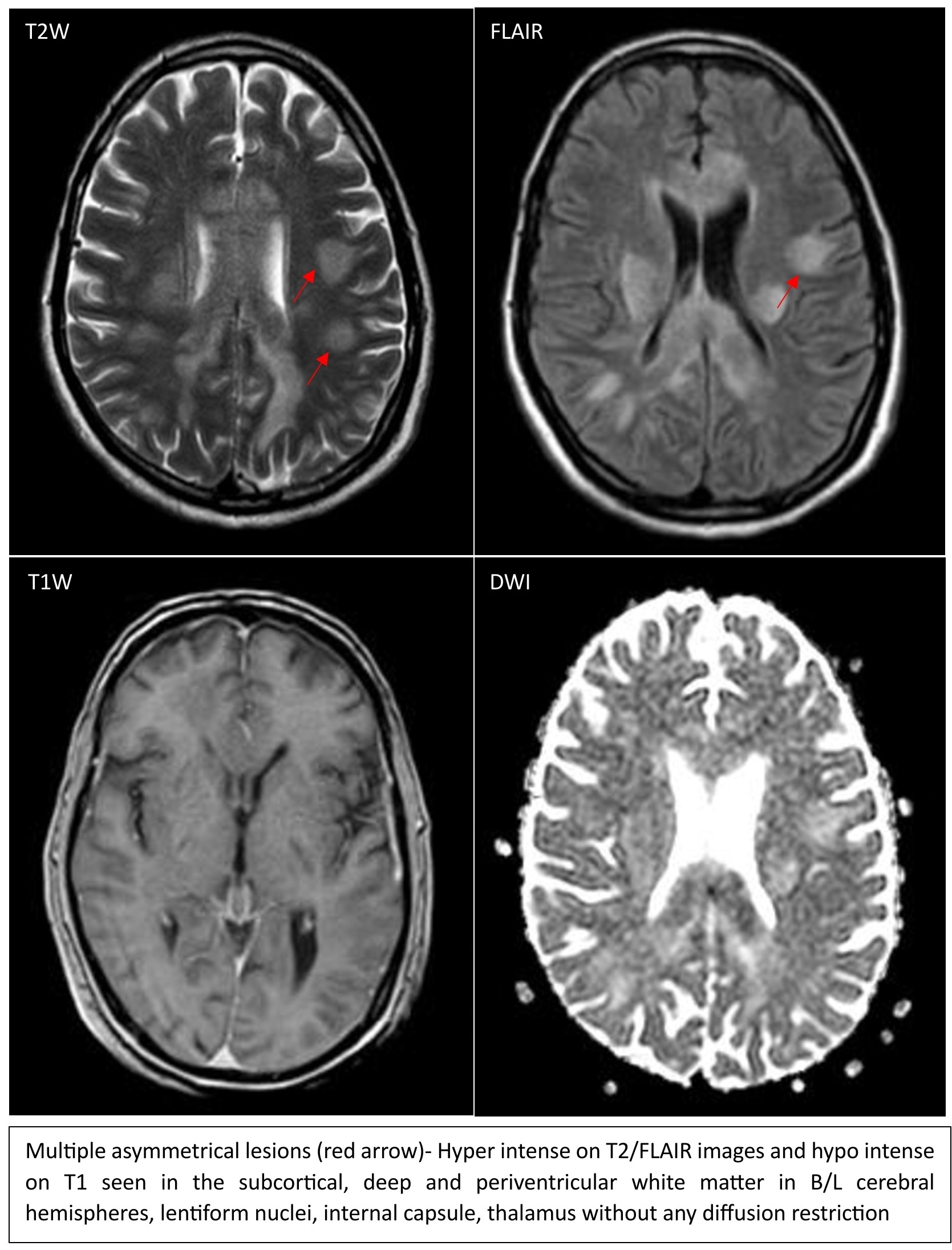
Figure 1
Discussion
The mean age of presentation of ADEM is 5-9 years, with a slight male predominance [5]. ADEM occurs less frequently in adults but cases can be seen. According to its presumed infectious etiologies, disease has a seasonal peak in the winter and spring [6]. In 50-85% of ADEM cases, the condition is preceded by an infection or vaccination. Viruses such as coronavirus, Coxsackie B, varicella-zoster virus (VZV), herpes simplex virus (HSV), Epstein-Barr virus (EBV), hepatitis A virus (HAV), hepatitis C virus (HCV), mumps, and rubella are the most common agents involved. Bacteria such as Streptococcus, Mycoplasma, Legionella, and Chlamydia can also rarely be involved [5]. Post-vaccination ADEM most commonly occurs after MMR vaccination and more rarely after polio, rabies, tetanus, hepatitis B, and influenza vaccination [5].
ADEM syndrome commonly manifests within a timeframe of 6 days to 6 weeks after an infectious disease [7]. It typically presents as a monophasic multifocal demyelinating disease. Prior to the onset of neurological signs and symptoms, individuals may experience systemic symptoms including fever, headache, malaise, myalgia, and nausea. These systemic manifestations may precede the neurological manifestations of ADEM [6]. Our patient also had a month long history of these symptoms. Neurological manifestations of ADEM vary depending on the specific areas of the central nervous system (CNS) that are affected. Common signs include obtundation (reduced alertness), depressed consciousness, unilateral or bilateral long tract signs (such as weakness or loss of sensation in the limbs), acute hemiparesis (weakness on one side of the body), and ataxia (uncoordinated movements). Depressed mental status and signs of meningismus (stiff neck and other symptoms associated with meningeal irritation) may also be observed. In adults, sensory deficits are more commonly observed compared to pediatric patients [6]. Our patient had neck rigidity but there was no sensory loss.
In ADEM, CSF analysis typically reveals inflammatory findings, such as elevated protein levels and lymphocytic pleocytosis, although it can be normal in some patients [5]. In TB meningitis, CSF typically shows low glucose and very high protein levels. Our patient had CSF findings of TB meningitis but negative studies on CSF culture and CBNAAT. Identifying Mycobacterium tuberculosis in cerebrospinal fluid (CSF) poses challenges due to the limited sensitivity of conventional methods such as microscopy and culture. The sensitivity of CSF microscopy is reported to be around 37%, while culture has a sensitivity of approximately 52%. Nucleic acid amplification tests (NAATs), such as polymerase chain reaction (PCR), have shown an average sensitivity of 56% in detecting M. tuberculosis in CSF. Therefore, CSF analysis is often helpful in confirming the presence of TB meningoencephalitis but may not definitively rule it out. The limitations in sensitivity of these tests highlight the need for a comprehensive clinical assessment, including clinical presentation, radiological findings, and other supportive investigations, in addition to CSF analysis, to establish a diagnosis of TB meningoencephalitis.
MRI shows multifocal inflammatory demyelinating lesions with poorly defined margins in the white matter of the CNS. These lesions appear as increased signal intensity on T2-weighted and FLAIR images [5]. Based on the similar MRI findings in our patient, we made a diagnosis of acute disseminated encephalomyelitis (ADEM). It is crucial to differentiate ADEM from multiple sclerosis (MS). Certain factors, such as later age at onset, the presence of prior infection or vaccination, consciousness alteration, characteristic MRI pattern, inflammatory changes in the cerebrospinal fluid (CSF), and the absence of oligoclonal bands, all support a diagnosis of ADEM [5]. In MS, MRI lesions are typically sharp and well-defined [6]. Moreover, compared to MS, brain lesions in ADEM less frequently involve the periventricular white matter and corpus callosum [5].
Treatment options for ADEM include corticosteroids, IVIg, and plasmapheresis, with corticosteroids being the first-line treatment. High-dose intravenous (IV) steroids, specifically IV methylprednisolone, are commonly administered in the treatment of ADEM. The typical dosage is 1g per day for a duration of 3-5 days. Following the IV steroid treatment, an oral corticosteroid, prednisolone, is usually initiated at a dosage of 1-2mg per kilogram of body weight per day. The oral prednisolone treatment is typically continued for 1-2 weeks. Over the subsequent 2-6 weeks, the dosage of prednisolone is gradually tapered to minimize potential side effects [5]. We treated our patient with ATT along with IV methylprednisolone followed by oral prednisolone.
Bibliography
- WHO. (2023) Global TB Report 2022. [Ref.]
- Masoodi I, Farooq O, Ahmad I, et al. (2010) Acute disseminated encephalomyelitis as the first presentation of CNS tuberculosis: report of a case with brief review. Ger Med Sci. 8: Doc32. [Ref.]
- Yang JH, Vuong KT, Moodley A, Chuang NA, Chen DY. (2021) A Case of Tuberculosis-Associated Acute Disseminated Encephalomyelitis in a Seven-Month-Old Infant. Cureus. 16299. [Ref.]
- (2023) Acute Disseminated Encephalomyelitis Following Pulmonary Tuberculosis. [Ref.]
- Berzero G, Cortese A, Ravaglia S, Marchioni E. (2016) Diagnosis and therapy of acute disseminated encephalomyelitis and its variants. Expert Review of Neurotherapeutics. 16(1): 83-101. [PubMed.]
- Noorbakhsh F, Johnson RT, Emery D, Power C. (2008) Acute Disseminated Encephalomyelitis: Clinical and Pathogenesis Features. Neurologic Clinics. 26(3): 759-780. [PubMed.]
- Özden HT. (2016) An Acute Disseminated Encephalomyelitis Case due to Mycobacterium tuberculosis. J Microbil Infect Dis. 6(1): 28-31. [Ref.]