>Corresponding Author : Zahri S
>Article Type : Case Report
>Volume : 4 | Issue : 1
>Received Date : 19 Dec, 2023
>Accepted Date : 04 Jan, 2024
>Published Date : 08 Jan, 2024
>DOI : https://doi.org/10.54289/JCRMH2400101
>Citation : Zahri S, Belhakim M, Chbir N, Zagdane S and Habbal R. (2024) Cardiovascular Evaluation in Pre-Anesthetic Consultations: A Prospective Descriptive Study. J Case Rep Med Hist 4(1): doi https://doi.org/10.54289/JCRMH2400101
>Copyright : © 2024 Zahri S, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Case Report | Open Access | Full Text
Cardiology department UHC Ibn Rochd, Casablanca
*Corresponding author: Zahri Soukaina, Cardiology department UHC Ibn Rochd, Casablanca
Abstract
Pre-anesthetic consultations play a pivotal role in assessing potential risks associated with planned surgeries. Cardiovascular evaluation, a crucial component of these consultations, holds significant implications for perioperative anesthetic management. This study, conducted prospectively on 72 out of 2284 patients undergoing specialized pre-anesthetic cardiology consultations at the Hospital 20 August, spans four months from June 1 to October 1, 2019. This research highlights the crucial significance of preoperative cardiovascular evaluations conducted in dedicated pre-anesthetic cardiology consultations. The study reveals epidemiological peculiarities and discrepancies compared to other research, underscoring the necessity for a personalized approach to perioperative cardiovascular risk assessment. The intricate decision-making involved, guided by diverse clinical and paraclinical parameters, points towards opportunities for enhancing future research and clinical protocols.
Abbreviations: ECG: Electrocardiograms, LVEF: Left Ventricular Ejection Fraction
Introduction
The cardiovascular assessment is a vital component of pre-anesthetic consultations, given that cardiac function is a crucial hemodynamic determinant allowing for better perioperative management from an anesthetic perspective. Preoperative cardiovascular evaluation serves to identify and assess the severity of pre-existing cardiac conditions that could impact vital prognosis and evaluate perioperative cardiovascular risk, considering patient risk factors, including functional capacity, surgery-related risk factors, and the degree of urgency. This assessment can lead to various measures, all aimed at reducing perioperative morbidity and mortality, including optimizing medical treatment of underlying heart conditions, defining hemodynamic goals, modifying the surgical and/or anesthetic technique, intraoperative monitoring, and specific postoperative surveillance or collective reassessment of the risk-benefit ratio for a scheduled surgical intervention. The cardiovascular assessment primarily focuses on risk stratification related to surgery using established scoring systems by professional societies, developing a strategy for ordering additional tests, and identifying appropriate therapeutic measures for primary prevention pre and post-operatively [1-3]. This study aims to identify pre-existing cardiac pathologies, assess perioperative cardiovascular risk, and implement preventive measures.
Methods
This prospective descriptive study focused on 72 patients, out of 2284, undergoing specialized pre-anesthetic cardiology consultations at Hospital 20 August. The study duration was four months, from June 1 to October 1, 2019.
1. Inclusion criteria
Our study included:
- Any adult patient over 15 years of age, presenting at the anaesthesia consultation for scheduled surgery in Otolaryngology or Ophthalmology or Maxillofacial Surgery during the study period requiring referral to a specialist cardiology opinion.
2. Exclusion criteria
- Any patient presenting for urgent surgery
Results
The average age of patients was 66 years, with a female predominance (52.77%). The majority of patients (56.3%) were admitted for ophthalmic surgery. The main cardiovascular risk factors were menopause (45%) and smoking (36.2%) (figure1). Eight patients had a history of cardiovascular events, primarily involving cardiac arrhythmias. Twenty-six patients had medical histories, with 11.11% being diabetic. Nineteen patients (26.38%) were taking cardiovascular medications. ASA II was the most common class (68.05%). Clinical examination revealed dyspnea in 66.2% of patients(figure2). Electrocardiograms (ECGs) showed anomalies in 63.88% of patients, including complete arrhythmia due to atrial fibrillation (4.16%). Echocardiography detected abnormalities in 34.28% of patients, with an average left ventricular ejection fraction (LVEF) of 59.71%. Coronary angiography was performed in one patient, revealing stenosis of the circumflex artery. Preoperative preparation involved discontinuing certain cardiovascular medications in 17.7% of patients.

Figure 1. distribution of different cardiovascular risk factors
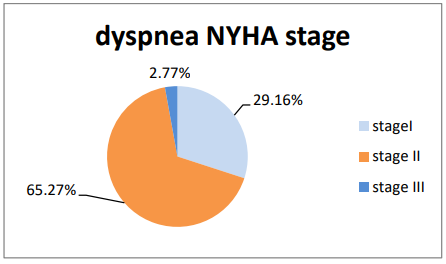
Figure 2. distribution of the different NYHA stage
Discussion
The epidemiological data reveals that the average age of patients in the study is 66.20 years, exhibiting variations compared to other studies such as those by Li Xu et al., Davenport, and KERZAZ [4-6]. The male proportion is 47.22%, varying from other studies, attributed to surgery types and indications, like the prevalence of goiters in women in ENT [7,8]. Major cardiovascular risk factors identified include smoking and menopause, in contrast to other studies that emphasize hypertension and diabetes. The preoperative clinical assessment involves the use of the ASA class, MET functional capacity, NYHA stage for dyspnea intensity, chest pain evaluation, and the Lee score for cardiovascular risk. Clinical examinations aim to detect various conditions, with notable differences from other studies in the prevalence of murmurs and other signs [9].
The preoperative management section details the use of ß-blockers, emphasizing their role in reducing myocardial oxygen consumption and preventing complications. Recommendations for initiation, continuation, and discontinuation of ß-blockers are discussed based on coronary insufficiency, high-risk surgeries, and intermediate-risk surgeries [10]. The section on Renin-Angiotensin System Inhibitors (IEC and ARA II) highlights their potential impact on blood pressure during general anesthesia, necessitating careful decision-making regarding their use. Practical recommendations for stopping or continuing these medications are outlined based on hypertensive or heart failure patients. Results indicate that 11.11% of patients were on Renin-Angiotensin System Inhibitors, which were replaced by calcium channel blockers preoperatively [11]. Calcium channel blockers are discussed in terms of their effects, particularly the dihydropyridine group's impact on baroreflex and heart rate. Vérapamil and diltiazem, with negative chronotropic effects, are mentioned with attention required during anesthesia [12]. Statins are discussed for their beneficial effects on perioperative destabilization of coronary disease, including endothelial function normalization and plaque stabilization. Practical recommendations for statin administration, especially in chronic users, highlight the risk of postoperative complications associated with discontinuation [13]. The anticoagulant section details considerations for anti-vitamin K and heparin use in various patient groups, such as those with atrial fibrillation, mechanical heart valves, and a history of venous thromboembolism. Practical recommendations for surgery types and urgent interventions are provided, emphasizing the need for careful monitoring and decision-making based on individual patient profiles [14].
Conclusion
This study underscores the critical role of preoperative cardiovascular assessments in specialized pre-anesthetic cardiology consultations. Epidemiological specificities and variances from other studies are evident, emphasizing the need for an individualized approach to perioperative cardiovascular risk assessment. The complex decision-making process, guided by diverse clinical and paraclinical parameters, suggests avenues for refining future research and clinical protocols.
References
- K Abbas. (2012) Preoperative cardiac evaluation in proximal femur fractures and its effects on the surgical outcome. [PubMed.]
- P Coriat. (2017) Gestion préopératoire des médicaments cardiovasculaires. Journée monothématique de la Sfar. [Ref.]
- G Weil, J-L Bourgain. (2012) Consultation préanesthésique. EMC - Anesth-Réanimation. [Ref.]
- Lee J Alfred. (1949) The Anaesthetic Out Patient Clinic. Anaesthesia. 221447972. [Ref.]
- (2010) Société française de cardiologie Collège des Enseignants de Cardiologie et Maladies Vasculaires dyspnée. [Ref.]
- T Iaiche Achour. (2019) Intérêt De La Création De Consultation Pré Anesthésique Des Patients À Risque Cardiovasculaire –Revue De L’inpfp. [Ref.]
- GF Fletcher, GJ Balady, EA Amsterdam, et al. (2001) Exercise standards for testing and training: a statement for healthcare professionals from the American Heart Association. Circulation. 104(14): 1694-1740. [PubMed.]
- SD Russell, MA Saval, JL Robbins, et al. (2009) New York Heart Association functional class predicts exercise parameters in the current era. Am Heart J. 158(4): 24-30. [PubMed.]
- CH Shin, SD Grabitz, FP Timm, et al. (2017) Development and validation of a Score for Preoperative Prediction of Obstructive Sleep Apnea (SPOSA) and its perioperative outcomes. BMC Anesthesiology. [Ref.]
- P Diemunsch, O Langeron, M Richard, et al. (2008) Prédiction et définition de la ventilation au masque difficile et de l’intubation difficile. Ann Fr Anesth Réanimation. 27: 3-14. [Ref.]
- S Kheterpal, L Martin, AM Shanks, et al. (2009) and outcomes of impossible mask ventilation: a review of 50,000 anesthetics. Anesthesiology. 110(4): 891-897. [PubMed.]
- L Keay, K Lindsley, J Tielsch, J Katz, O Schein. (2012) Routine preoperative medical testing for cataract surgery. Cochrane Database of Systematic Reviews. 3(3): CD007293. [PubMed.]
- PSA Chung. (2009) Elimination of preoperative testing in ambulatory surgery. 108(2): 467-475. [PubMed.]
- GW Smetana, DS Macpherson. (2003) The case against routine preoperative laboratory testing. 87(1): 7-40. [PubMed.]