>Corresponding Author : Zeinab Tardeh
>Article Type : Case Report
>Volume : 3 | Issue : 9
>Received Date : 02 Dec, 2023
>Accepted Date : 15 Dec, 2023
>Published Date : 20 Dec, 2023
>DOI : https://doi.org/10.54289/JCRMH2300145
>Citation : Makhsosi BR and Tardeh Z. (2023) Laparoscopic Surgery of an Isolated Splenic Hydatid Cyst in a 43- Year- Old Man: A Case Report. J Case Rep Med Hist 3(9): doi https://doi.org/10.54289/JCRMH2300145
>Copyright : © 2023 Tardeh Z, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Case Report | Open Access | Full Text
1Department of Laparoscopic Surgery, Imam Reza Hospital, Kermanshah University of Medical Sciences, Kermanshah, Iran
2Department of General Surgery, Faculty of Medicine, Kermanshah University of Medical Sciences, Kermanshah, Iran
*Corresponding author: Zeinab Tardeh, Department of General Surgery, Faculty of Medicine, Kermanshah University of Medical Sciences, Kermanshah, Iran
Abstract
Introduction: Hydatid disease is a type of parasitic disease mainly affect the lungs and the liver and splenic hydatid cyst is a rare disease. We hereby present a rare case of splenic hydatid disease.
Case report: A 43-years-old man with a history of left upper quadrant pain (LUQ) pain, anorexia, weakness, and weight loss was admitted to the surgery department in Iran. The imaging studies showed a cystic mass in the gastro-splenic ligament extending up to below the left diaphragm with adhesion to the spleen capsule and the fundus of the stomach caused focal elevation of this part of the diaphragm. A laparoscopic surgery was performed and splenic hydatid cyst with adhesion to the stomach and the left lobe of the liver and with penetration into the left hemi thorax was observed. Splenectomy, hepatectomy of the left segment of the liver, repair of diaphragmatic defect and stomach release was done.
Conclusion: Splenic hydatid cyst surgery can be difficult and requires appropriate diagnostic evaluations and examination for adhesions and invasion to other organs.
Keywords: Hydatid Disease; Laparoscopic Surgery; Case Report
Abbreviations: LUQ: Left Upper Quadrant, CT: Computerized Tomography, IV: Intravenous, CBC: Complete Blood Count, ELISA: Enzyme-Linked Immunosorbent Assay
Introduction
Hydatid disease is a type of parasitic disease in which humans are accidental hosts of Echinococcus granulosus tapeworms, and the organs mainly affected by this disease are the lungs and the liver [1,2]. Hydatid disease has a geographical distribution in livestock breeding areas [3]. In addition to the liver and lungs, which are common organs of involvement, hydatid disease can affect other parts of the body such as the spleen for which splenic hydatid cyst is a rare disease [4]. Splenic hydatid cyst can be primary or secondary, with the primary type being rarer than the secondary type. Splenic hydatid cyst symptoms vary based on size, proximity to different organs, and disease complications [5,6]. Manifestations of splenic hydatid cysts range from asymptomatic and incidental cases to largely symptomatic or complicated cases [7,8]. Despite the existing hydatid cyst diagnostic methods including ultrasound, computerized tomography (CT) scan, and serological tests, hydatid cyst remains difficult to diagnose [9]. The treatment of choice for splenic hydatid cyst is splenectomy [10]. Due to the advantages of laparoscopic splenectomy, such as less morbidity and shorter hospitalization, this method is more popular than open surgery [11]. However, when it comes to hydatid cysts, laparoscopic splenectomy could be a challenging procedure.
Case report
A 43-years-old man with a history of left upper quadrant pain (LUQ) pain, anorexia, weakness, and weight loss of about 10 kilograms in 4 months was admitted to the surgery department of Imam Reza Hospital, Kermanshah, Iran. He had no symptoms of nausea and vomiting or fever. The patient had a history of occasional salty taste in the mouth. He was from a village and had a history of contact with dogs and sheep. The patient had no history of underlying disease but had a history of skin graft surgery due to burn injury. On the abdominal examination, the patient had splenomegaly, but there was no distention, tenderness, or guarding.
In the abdominopelvic CT scan with intravenous (IV) contrast report in the gastro-splenic ligament, a 66× 62 × 86 millimeters (mm) cystic mass extending up to below the left diaphragm was diagnosed, with adhesion to the spleen capsule and the fundus of the stomach. The upper extension of the lesion to anterior part of the left diaphragm caused focal elevation of this part of the diaphragm. The lesion had a thick wall and contained multiple internal septa and loculations with the appearance of a daughter cyst, typical of an active hydatid cyst.
A small part of the posterior wall of the lesion was calcified. Inside the parenchyma of the upper part of the spleen, a completely calcified mass 20 mm in diameter was evident, suggesting an old calcified and inactive hydatid cyst. Bilateral lipomatosis was seen in the kidney, and other organs were reported to be normal (Figure1). No pathological findings were found in the chest CT scan. The patient's complete blood count (CBC) and biochemistry tests were within normal ranges. The Enzyme-linked immunosorbent assay (ELISA) test was also positive.
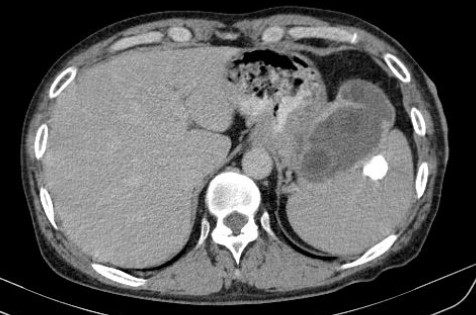
Figure 1. Abdominopelvic CT scan in the patient with splenic hydatid cyst
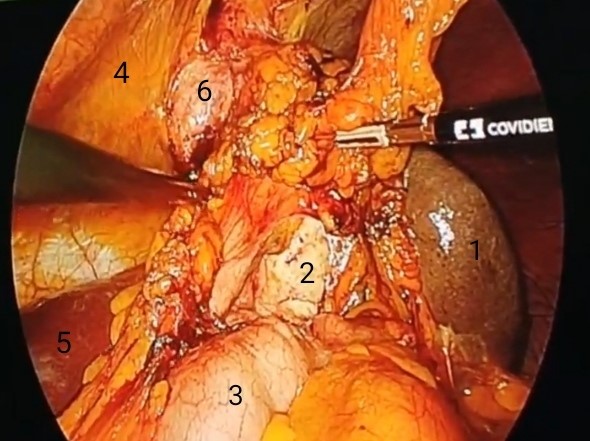
Figure 2. Intraoperative photo: spleen (1), hydatid cyst (2), stomach (3), diaphragm (4), liver (5), hydatid cyst penetrated into the left hemithorax (6).
The patient was diagnosed with splenic hydatid cyst and underwent surgery. The patient was placed in the right lateral decubitus position. First, a 10 mm umbilical trocar was placed and the abdomen was inflated. After the camera was inserted, under direct vision, a 5-mm trocar was placed in the sub-xiphoid on the left side of the falciform ligament, a 5-mm trocar was placed in the inferior pole of the spleen on the left side, and a 10-mm port was placed in the midclavicular line.
A splenic hydatid cyst with penetration into the left hemi thorax and adhesion to the stomach and the left lobe of the liver was observed. A piece of gauze impregnated with hypertonic saline was placed around the cyst, and then the contents of the cyst were aspirated with a veres needle. Then 100 cc of 70% alcohol was injected into the cyst which was aspirated 5 minutes later. This procedure was repeated twice. After adhesionolysis, the gastro-splenic ligament was released and the splenic vein and artery were ligated. The spleno-phrenic and spleno-colic ligaments were also released, and then hepatectomy of the left segment of the liver was done and due to adhesion of the stomach to the cyst, it was released with a stapler.
Due to the penetration of the mass into the left hemi thorax, an attempt was made to release the mass, but during the release process, a defect was created in the left hemi-diaphragm. Then splenectomy was done, which involved removing the spleen out of the abdomen using a sac. After hemostasis was done, the left side of the diaphragm was repaired. Then the peritoneal cavity was irrigated using 1000 cc normal saline. A hemovac drain was placed into the splenic cavity, and then the trocars were removed. The pathology report confirmed the diagnosis of hydatid cyst. After surgery, the patient was transferred to the ward, and Albendazole 400 milligrams(mg) every 12 hours was started for the patient and continued until 6 months later. The patient was followed-up every one month, and he was still asymptomatic. The feeling of salty taste in the mouth, which suggested hydatid cyst fistula to the stomach, also disappeared.
Discussion
Hydatid cyst affects different parts of the body, and sites most commonly affected by this disease include the liver and the lungs [12]. Involvement of the spleen, especially isolated and primary, is rare in hydatid disease, which may make splenic hydatid cysts difficult to diagnose, especially in non-endemic areas [13,14]. An important differential diagnosis in patients with cystic lesions of the spleen in endemic areas is hydatid cyst [12]. A splenic hydatid cyst can lead to life-threatening conditions such as an anaphylactic reaction, rupture into the pleura, or hollow viscera, and therefore its treatment is of utmost importance [5]. Splenic hydatid cysts must be surgically removed due to the risk of rupture, and the best surgical method in adults is splenectomy, which has been associated with good results and low recurrence rate [14]. Treatment varies based on individual characteristics, degree of disease, and experience of the surgeon [15]. Total splenectomy is the surgical method of choice for the treatment of splenic hydatid cyst, especially in underdeveloped countries. The laparoscopic approach has comparable or even better results than open surgery, as its advantages include less trauma, minimal postoperative pain, reduced wound infections, and shorter hospital stays [3,16]. Total splenectomy brings about a reduction in the duration of hospitalization, complications, the cost of care, and the rate of recurrence. Therefore, it should be considered in endemic areas in underdeveloped countries [6,16]. Spleen preservation methods can prevent postoperative infections [17]. In previous studies, laparoscopic partial pericystectomy with omentoplasty has been introduced as a safe and effective method for splenic hydatid cysts [9,18]. There is still controversy about the best surgical method, which calls for careful examination of various factors. In children, however, spleen preservation methods are recommended [19].
Conclusion
Considering that splenic hydatid cyst is a rare disease, it can be difficult to diagnose splenic hydatid cyst, especially in non-endemic areas. Despite the risks reported for total splenectomy, this method is still the surgical method of choice, especially in endemic areas, and in underdeveloped countries, which is highly efficient when performed laparoscopically. Splenic hydatid cyst surgery can be difficult and requires appropriate diagnostic evaluations and examination for adhesions and invasion to other organs. In the meantime, the scolex should be prevented from spilling into the abdomen to prevent recurrence. On the one hand, it is more difficult to treat the recurrence of the disease and on the other hand Albendazole cannot penetrate to the large volume of the cysts.
Acknowledgments: We thank the patient for his informed consent to publish the case report.
Conflict of interests: None
Informed consent: A written informed consent was obtained from the patient.
Funding: None
References
- Gupta V, et al. (2014) Primary hydatid cyst of spleen: a rare entity. J Trop Dis. 2(2): 1. [Ref.]
- Ramosaço E, et al. (2020) Primary multiple cerebral hydatid cysts in an immunocompetent, low-risk patient. IDCases. 21: e00882. [PubMed.]
- Yotsov TI, S Dyulgerova and D Draganova. (2023) Laparoscopic splenectomy for solitary splenic hydatid cyst: Case report. Journal of Minimal Access Surgery. [PubMed.]
- Malik AA, et al. (2011) Primary splenic hydatidosis. Indian Journal of Gastroenterology. 30: 175-177. [PubMed.]
- Belli S, et al. (2014) Spontaneous giant splenic hydatid cyst rupture causing fatal anaphylactic shock: a case report and brief literature review. Turkish Journal of Gastroenterology. 25(1). [PubMed.]
- Ghabisha S, et al. (2021) Isolated giant primary splenic hydatid cyst in a 10-year-old boy: a case report. Pediatric Health, Medicine and Therapeutics. 55-59. [Ref.]
- Malik AA, et al. (2019) Hydatid Disease of the Liver: Clinical Presentation and Complications. Human Abdominal Hydatidosis. 15-23. [Ref.]
- Singh S, et al. (2022) A case of giant primary splenic hydatid cyst: Case report. Annals of Medicine and Surgery. 84: 104829. [Ref.]
- Milosavljevic V, et al. (2019) Laparoscopic management of initially unrecognized splenic hydatid cysts: a case report and review of the literature. Medicina. 55(12): 771. [Ref.]
- Ramia-Ángel JM, et al. (2011) Hidatidosis of the spleen. Polski przeglad chirurgiczny. 83(5): 271-275. [PubMed.]
- Winslow ER and LM Brunt. (2003) Perioperative outcomes of laparoscopic versus open splenectomy: a meta-analysis with an emphasis on complications. Surgery. 134(4): 647-653. [PubMed.]
- Rawat S, et al. (2019) Pulmonary hydatid cyst: review of literature. Journal of family medicine and primary care. 8(9): 2774. [Ref.]
- Rasheed K, SA Zargar and AA Telwani. (2013) Hydatid cyst of spleen: a diagnostic challenge. North American journal of medical sciences. 5(1): 10. [Ref.]
- Aghajanzadeh M, et al. (2019) Reports of symptoms, diagnosis and management of eight cases of primary and isolated splenic hydatid cyst. JSM Clinical Cytology and Pathology. 4: 5. [Ref.]
- Hashemzadeh S, et al. (2021) A giant splenic hydatid cyst: Why calcified cysts should not be considered as a dead cyst. Clinical Case Reports. 9(1): 269-273. [Ref.]
- Mejri A, et al. (2021) Primitive isolated hydatid cyst of the spleen: total splenectomy versus spleen saving surgical modalities. BMC surgery. 21(1): 1-6. [Ref.]
- Merad Y, et al. (2021) Primary splenic hydatid cyst an unexpected diagnosis: Case report. Annals of Medicine and Surgery. 65: 102293. [Ref.]
- Hoteit A, et al. (2020) Primary splenic hydatid cyst treated with laparoscopic spleen preserving surgery: a case report. International Journal of Surgery Case Reports. 74: 95-98. [PubMed.]
- Jarray L, et al. (2022) Spleen-sparing excision of giant splenic hydatid cyst. Journal of Pediatric Surgery Case Reports. 76: 102088. [Ref.]